Causes of elbow bursitis
Factors that provoke the occurrence of bursitis of the elbow joint can be divided into 2 groups:
Infectious bursitis occurs:
- As a complication of bacterial and viral processes
- As a result of the introduction of microbes with the flow of lymph or blood from foci of purulent inflammation, for example, from abscesses
Non-infectious bursitis occurs as a result of:
- Minor but frequently recurring elbow injuries
- Posterior elbow injury
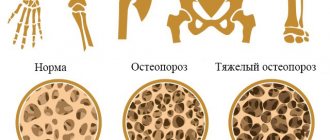
- Arthrosis of the joint is the most common cause of chronic bursitis as a result of constant irritation of the joint by osteophyte bone spines.
- Excessive stress on the elbow joint, for example in heavyweight athletes
- Metabolic disorders, such as gout
- Hormonal changes
- Rheumatoid arthritis, psoriasis
Causes of bursitis
Inflammation of the bursa of the elbow joint can be caused by:
- arthritis (rheumatoid, psoriatic, gouty);
- microtraumas (damage associated with constantly repeating monotonous movements or constant support of the elbow on a hard surface);
- mechanical injury to the elbow (for example, falling on it);
- infection (can penetrate from the outside through the wound surface or come with the blood and lymph flow from other areas of the body);
- provoking factor (diabetes mellitus, reduced immunity, metabolic disorders, use of steroid hormones).
Stages of development of bursitis of the elbow joint
Joint inflammation occurs in several successive stages: acute, subacute, chronic.
Acute stage
Most cases of bursitis begin in the acute stage. As a result of the injury, the synovial bursa becomes inflamed, which in turn is manifested by pain that increases with movement, as well as swelling and increased temperature over the affected joint.
Subacute stage
Swelling and temperature decrease, acute pain is replaced by dull, aching sensations while moving the arm.
Chronic stage
In the absence of timely treatment, acute inflammation becomes chronic. Chronic bursitis also occurs when the elbow joint is constantly irritated, for example, by bone spikes that form during arthrosis. With chronic bursitis, there is constant pain, swelling in the elbow area, and limited mobility in the elbow joint.
Recurrent variant of elbow bursitis
With this variant of the course of the disease, periods of exacerbation are replaced by periods of remission, when inflammation and associated symptoms are absent. The provocateur of the next episode of exacerbation, as a rule, is infection, injury, or decreased immunity.
Bursitis of the feet and heels
Inflammation in this area occurs due to:
- constant increased loads (in weightlifters, overweight patients);
- congenital foot abnormalities (valgus deformity of the big toe, flat feet);
- traumatic injuries to the foot (deep wounds/cuts in the area of the synovial bursae);
- arthritis of the foot;
- chronic inflammatory processes (abscesses, boils).
Bunions can occur in women who wear high-heeled shoes. However, an absolutely flat sole also acts as a provoking factor in the development of inflammation of the synovial bursa. Bursitis of the feet and heels can be a consequence of constantly wearing poorly fitting shoes. The unnatural position of the foot causes deformation of the synovial bursa, which is why the inflammatory process develops. Achilles bursitis (calcaneal) is an inflammation of the synovial bursa located between the Achilles tendon and the heel bone. One of the causes of the disease is traumatization of the synovial bursa by the hard back of the shoe.
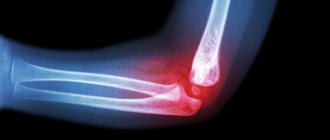
Symptoms of elbow bursitis
The main symptoms are pain and swelling in the elbow joint. Initially, symptoms appear only with movement; as the disease progresses, especially in the absence of treatment, the pain becomes constant. In the acute period, a local increase in body temperature (in the elbow area) is observed, patients may complain of malaise, weakness, loss of appetite and headache. In people with weakened immune systems, in the absence of comprehensive treatment, a serious complication may develop - purulent inflammation (purulent bursitis, abscess or phlegmon). The pain becomes pulsating, the skin over the joint turns red, becomes swollen and hot to the touch. Accompanied by increased body temperature and enlarged axillary lymph nodes.
Symptoms and treatment of bursitis
Bursitis is an inflammation of one or more synovial bursae (bursae) in the joint area.
The cavity of the bursae is lined with a synovial membrane that secretes a lubricating fluid. There are about 160 synovial bursae in the human body. With inflammation of the bursa of any location, for example, with bursitis of the ankle joint, the slightest movement causes pain. Symptoms of bursitis range from erythema to swelling, severe pain in the joint and spread of inflammation to adjacent tissue. The pain usually worsens during and after loading the joint.
Treatment of elbow bursitis
Treatment of elbow bursitis is prescribed individually depending on the cause of the disease, the severity of its course, the presence of complications, and the patient’s health condition.
General principles of therapy for non-purulent bursitis:
- Eliminating the root cause of elbow bursitis
- Rest for the hand - a special bandage, like a “scarf”, so that the hand lies in it
- Cool compresses to reduce swelling
- Pain relief and reduction of inflammation with nonsteroidal anti-inflammatory drugs (NSAIDs), and in severe cases, corticosteroid hormones
- Removing fluid accumulated in the joint cavity. The procedure is performed under local anesthesia and ends with antiseptic treatment of the joint capsule.
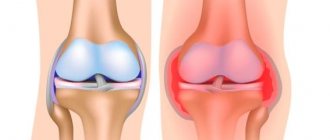
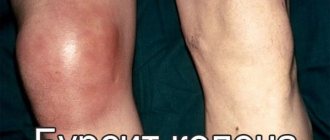
Bursitis of the knee joint
Suprapatellar bursitis of the knee joint is usually a consequence of injury or excessive stress on the joint during work or sports.
Symptoms of knee bursitis:
- localized soft tumor;
- knee pain when walking or running;
- pain that increases with palpation;
- pain at rest.
Treatment of suprapatellar and prepatellar bursitis follows the same scheme. Rest and a cold compress on the knee are recommended for the first 24–48 hours of illness. Anti-inflammatory drugs are prescribed by a doctor. Aspiration of the exudate can be performed with further rinsing of the cavity with an antibiotic solution. For purulent bursitis, opening the joint capsule and removing pus is indicated.
Treatment of purulent ulnar bursitis
In the treatment of infectious bursitis the following are prescribed:
- Broad-spectrum antibiotics to which most microorganisms are sensitive. However, it is preferable to examine the contents of the joint capsule in the laboratory. This allows you to determine the sensitivity of microflora to antibiotics and select the most effective agent.
- NSAIDs (non-steroidal anti-inflammatory drugs) reduce pain and inflammation in the joint.
- Externally, anti-inflammatory ointments and creams, compresses and dressings with medications can be recommended.
Post-traumatic bursitis, synovitis
Among soft tissue injuries that are potentially dangerous in terms of the development of purulent complications, there are:
- soft tissue bruise;
- superficial damage to the skin (abrasions, scratches, scratches);
- open damage to the skin (torn, cut, stab, bruised, chopped, bitten wounds);
- scalp wounds;
- gunshot and shrapnel wounds;
- soft tissue crushing;
- long crush syndrome
Purulent and infectious complications of soft tissue injuries include:
- infected wound with or without cellulite;
- festering hematoma;
- purulent bursitis, synovitis and arthritis;
- abscess;
- phlegmon;
- necrosis of skin and other soft tissues;
- osteomyelitis;
- giving birth;
- anaerobic clostridial and non-clostridial infection;
- post-traumatic gangrene of a limb
The severity of both the injury itself and the developing purulent complication often entails the inevitable loss of a large amount of tissue, much larger than the primary lesion.
In the treatment of purulent post-traumatic complications, a key role is played by adequate surgical treatment of the purulent focus in accordance with the principles of active surgical treatment, which implies radical surgical treatment of the purulent focus, intensive antibacterial and detoxification therapy, followed by skin grafting of the wound defect. The treatment of patients with extensive purulent processes of soft tissues is described in more detail in other sections. I would like to dwell in more detail on post-traumatic synovitis and bursitis.
Synovitis is an inflammation of the synovial membrane of a joint, limited to its limits.
Post-traumatic synovitis is most common in clinical practice. Most often, large joints are affected (elbow, knee, wrist, ankle). With synovitis, movements in the joint are sharply limited and painful. A characteristic change in the shape of the joint is caused by the appearance of effusion in the articular cavity. There is weakness, malaise, and increased body temperature.
As first aid for synovitis, joint puncture with evacuation of synovial fluid and rigid immobilization of the joint for 5-7 days are indicated using hypothermia (local cold) in the first days. Conservative treatment includes non-steroidal anti-inflammatory drugs (Nice, Movalis), in case of infection - broad-spectrum antibiotics, physiotherapeutic procedures (magnetic therapy, UHF).
Treatment of patients with traumatic synovitis should be comprehensive. The choice of treatment method in each individual case must be decided individually, depending on the severity of the injury, the nature of intra-articular changes and other reasons. After surgical treatment, it is necessary to carry out a full course of drug correction of metabolic disorders of the internal environment of the joint, as well as effective rehabilitation treatment. The result of treatment for synovitis in most cases is complete recovery (with serous and allergic synovitis), however, in some cases, stiffness or complete immobility in the joint may develop.
Bursitis is an inflammation of the synovial bursa with the accumulation of exudate in its cavity.
Most often it occurs in the shoulder joints, somewhat less frequently - in the elbows, knees, hips and in the synovial bursa between the Achilles tendon and the heel bone. The causes of bursitis, as a rule, are bruises of large joints, wound abrasions and cuts in the joint area. According to the clinical course, bursitis can be acute, subacute, chronic, recurrent; by the nature of the exudate - serous, serous-fibrinous, purulent, purulent-hemorrhagic. Characterized by swelling, hyperemia (redness), severe pain in the joint area, and increased body temperature.
For serous and serous-fibrinous bursitis, conservative treatment is indicated, including antibacterial therapy, non-steroidal anti-inflammatory drugs, physiotherapeutic procedures, and functional rest of the limb. For purulent and purulent-hemorrhagic bursitis, treatment is surgical. Adequate opening and drainage of the purulent focus with excision of the bursa (synovial bursa of the joint) is indicated.
The prognosis is usually favorable.
dr-anikin.ru
Hip replacement - choice of implant, indications, risks. Read on the website https://replaced.ru/endoprotezirovanie
Surgical treatment of elbow bursitis
Typically, elbow bursitis can be treated conservatively and does not require surgery. Surgical treatment may be required in case of frequent exacerbations of inflammation, as well as in the formation of serious purulent complications, such as an abscess or phlegmon. If surgical treatment is necessary, orthopedists often use bursa punctures to remove fluid and administer medications. If an abscess or phlegmon forms in the area of the elbow joint, the abscess is opened and drained, followed by antibacterial and anti-inflammatory therapy.
As the inflammation subsides, the doctor includes physical therapy in the complex treatment regimen: UHF, electrophoresis and thermal procedures.
- Warming up using a heating pad with hot water or a canvas bag with heated salt. Thermal effects improve blood microcirculation, thereby reducing swelling and pain. Paraffin therapy procedures are also popular. However, they are not recommended for skin damage or pustules in the elbow joint
- Electrophoresis is a painless procedure in which special electrodes are installed on the elbow joint, thanks to which microcurrents deliver medicinal substances directly to the area of inflammation.
- In recent years, shock wave therapy has been widely used. It significantly improves the condition of the joint, relieves pain and swelling, and returns the arm to its former activity and range of motion.
If the treatment is ineffective, complete removal (excision) of the ulnar bursa is possible.
Anatomy of education
The elbow joint is the joint that connects the distal part of the arm to the forearm. It is marked on the upper limb by the medial and lateral epicondyle and olecranon process. Structurally the joint is classified as a synovial joint and functionally as a ball and socket joint.
It consists of two separate articulations: the trochlear notch of the ulna and humerus, the head of the radius and the humerus.
Like all synovial joints, the elbow joint has a capsule that encloses the joint. This formation itself is strong and fibrous, strengthening the joint. The joint capsule is thickened medially and laterally, forming collateral ligaments that stabilize flexion and extension of the arm.
The bursa is a membrane sac filled with synovial fluid. It acts to cushion the moving parts of the joint, preventing degenerative damage. There are many bursae in the elbow, but only a few are of clinical importance: Intratendinous - located inside the triceps brachii tendon, Subtendinous - between the olecranon process and the triceps brachii tendon, reducing friction between the two structures when stretching and flexing the arm, Subcutaneous - between the olecranon process and the overlying connective tissue
How to treat bursitis
Treatment of bursitis of the elbow joint is mainly carried out using conservative methods. A good result is given by:
- Physiotherapeutic procedures are effective in reducing inflammation and pain, relieving muscle spasms, and have a beneficial effect on nerves and tendons. Physiotherapy is used to treat chronic bursitis and acute cases, has virtually no contraindications and perfectly complements other treatment methods. Ultrasound therapy (exposure to ultrasonic waves), diadynamic therapy (pulse currents), shock wave therapy, cryotherapy (low temperature treatment) and other procedures have shown good results in the treatment of joints.
- Therapeutic gymnastics - a special set of exercises will speed up the healing process. Exercise therapy improves blood circulation and lymph flow in the problem area, optimizes muscle function. Treatment with movement is especially important for the chronic form of the disease and prevention of relapses. At the same time, it is important not to cause harm - bursitis can be the result of heavy physical exertion, then the joint must be kept at rest during treatment. Whether to do exercises or not, and if you do, which ones, is the task for the treating orthopedic traumatologist and exercise therapy doctor, who will create a set of safe exercises and monitor the correctness of their implementation when exercising in the exercise therapy room.
- Medicines – for the medical treatment of elbow bursitis, anti-inflammatory and painkillers are used. Medicines can be in the form of tablets, injectables (including intra-articular injections), ointments and gels for topical use. For infectious forms of bursitis, antibiotics are prescribed.
Puncture of the joint capsule is a necessary measure for purulent inflammation, which does not improve with conservative treatment measures. The pus is pumped out through a puncture, the joint capsule is washed with drugs that relieve inflammation. After surgery for bursitis, a drainage hole may remain on the elbow joint (to avoid postoperative complications), and physiotherapeutic procedures will speed up healing.
When bursitis of the elbow joint occurs against the background of other diseases, the condition for recovery is their treatment. The doctor will definitely give recommendations after determining the diagnosis.
To make an appointment with a traumatologist-orthopedist or other doctor at the Kuntsevo Treatment and Rehabilitation Center, leave a request on the website or call.
Symptoms
The symptoms of bursitis of the elbow joint are:
- Severe or moderate pain (depending on the type of inflammation), feeling of heating, burning. The pain can radiate to neighboring joints - the wrist and shoulder.
- Swelling of the joint - a noticeable outward thickening (effusion) appears on the elbow. It is better visible when the arm is bent. The swollen area is soft and elastic to the touch. When pressing and bending, the pain intensifies.
- Redness of the skin in an enlarged area, locally increased temperature (local hyperemia). The temperature with bursitis of the elbow joint can reach 39-40 0C.
- Limitation of the range of motion in the joint - it is painful, and sometimes it is impossible to bend or straighten it completely.
- General intoxication of the body - increased temperature in general, weakness, headaches.
The first signs of bursitis of the elbow joint can appear within a few days from the moment of injury to the elbow; with chronic inflammation, they are quite weak, and with recurrent inflammation, they appear periodically during exacerbations.
Without proper treatment of elbow bursitis, inflammation can become chronic, leading to the formation of fistulas with purulent contents, abscesses, phlegmons - rupture of the internal cavity with pus and its spread to neighboring areas.