Pellegrini - Stied disease (m. Pellegrini - Stied), peritendinitis of the knee joint, shadow or Stied fracture, Stied - Pellegrini disease, post-traumatic paracondylar ossification of the thigh, paraosseous accompanying shadow of Pellegrini, Keller - Pellegrini - Stied disease. It was first described in 1905 by the Italian physician Pellegrini A., and in 1907 by the German surgeon Stied A. Ossification, located in the soft tissues in the area of the internal femoral condyle. What is it, what are the causes and symptoms, as well as treatment methods, we will consider further.
Features and general description
Pellegrini-Stied disease is a pathological bone growth characterized by a latent clinical picture. In scientific terms, we are talking about ossification of paraaticular tissues in the area of the epicondyle of the knee. The disease occurs most often due to injury or regular microtrauma against the background of significant loads on the joint.
The development of the pathological process begins with the formation of tendon ruptures and necrotic lesions in the muscle tissue. Progression may be complicated by reactive periarthritis. First, the tendon is involved in the pathological process, and then the synovial tissue. Periarthritis leads to tendobursitis. As a result, the soft tissues in the knee structure swell. At the same time, the patient already experiences difficulties with movement and is tormented by constant severe pain. Properly selected therapy leads to the disappearance of symptoms. Otherwise, residual manifestations of Pellegrini-Stied disease are revealed, which leads to its transformation into a chronic pathology.
Symptoms of Pellegrini-Stied disease
The onset of pathological changes is characterized by the formation of tendon ruptures and foci of necrosis in the periosteal muscle tissue. There are no external manifestations yet, so Pellegrini-Stida disease on the knee joints often remains untreated.
The progression of the disease is manifested by severe symptoms and reactive periarthritis. First, the tendon is affected, then the pathology affects the synovial tissue.
Characteristic signs of knee joint disease:
- pain in the area of ossification formation;
- irradiation of pain to the front of the leg;
- severity of torment at night;
- dysfunction of active flexion and extension of the knee;
- swelling of soft periarticular structures;
- local increase in skin temperature;
- increased or decreased sensitivity;
- atrophy of the muscular frame of the affected lower limb.
Pellegrini Stida disease may have similar symptoms and signs to other knee diseases, so see your doctor for an accurate diagnosis.
Main reasons
Men aged 25 to 45 years, whose daily work is directly related to sports or physical activity, are predisposed to the disease. Provoking factors are direct mechanical injury to the thigh and sudden abduction of the lower leg. In addition, the following factors may accompany Pellegrini-Stied disease:
- bleeding in the knee;
- necrotic processes in periarticular tissues;
- hormonal imbalances;
- the presence of varicose veins;
- arthritis;
- trophic disorders;
- prolonged swelling in the knee area.
Doctors also warn about a hereditary predisposition to the pathology. This is due to the genetic characteristics of bone growth. The presence of close relatives with its manifestations sharply increases the likelihood of a repetition of the diagnosis in the family. However, even in this case, a trigger in the form of injury will be needed.
What kind of disease is this?
Pellegrini-Stida disease is a post-traumatic ossification of paraarticular tissues in the area of the medial epicondyle of the femur. Most authors consider it a disease of traumatic origin. When the internal ligament is torn from the femoral condyle at the site of its attachment, the periosteum rises and a subperiosteal hematoma is formed, which undergoes ossification. The disease develops more often in men aged 25-45 years, mainly among those involved in physical labor or sports.
Most patients are asymptomatic or with minor pain in the medial part of the knee joint.
In cases of timely contact with specialists and the correct prescription of therapy, the prognosis in most cases is favorable and the patient’s complete recovery is observed.
- ICD-10 code: in classes M70-M79, combining “Other soft tissue diseases”, Pellegrini-Stida disease is designated by code M76.4 under the name “Tibial collateral bursitis”.
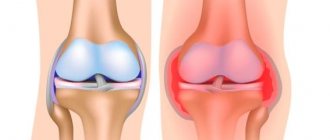
Clinical picture
For a long time, Pellegrini-Stied disease of the knee joint can be asymptomatic. At the same time, patients often complain of discomfort in this area, which only intensifies after physical activity or sports. As the disease progresses, the clinical picture is supplemented by swelling, pain, redness of the skin around the affected joint, and increased temperature in this area. In addition, difficulties with movement may occur, gait changes and lameness appears. In the case of a prolonged pathological process, the volume of motor activity is reduced. In the final stages of the disease, a person loses the ability to make full movements in the knee joint, and ankylosis occurs.
Treatment of pathology
Therapy for Pellegrini-Stida disease should be comprehensive and include therapeutic techniques that are used in the early stages of the development of the process. In severe cases, surgery is used. Traditional methods of treatment are used as an additional method before the main therapy. At the initial stages of the disease, non-steroidal anti-inflammatory drugs are used, which relieve signs of inflammation and reduce pain. Muscle relaxants, chondroprotectors and vitamin complexes are also indicated.
Herbal medicine using decoctions of anti-inflammatory herbs will be useful.
If the volume of motor activity of the limb decreases, surgery is performed. During its course, the overgrown bone is removed, and the altered cartilage is removed and replaced with its own cartilage tissue taken from other parts of the body. After surgery, the patient requires a long period of rehabilitation. For this purpose, a complex of physiotherapeutic measures is carried out, therapeutic massage and restorative gymnastics are prescribed.
Source etosustav.ru
PELLEGRINI-STIDE DISEASE
(A. Pellegrini, Italian surgeon; A. Stieda, German surgeon, 1869-1945; synonym:
Stida fracture, Stida-Pellegrini syndrome
) - post-traumatic ossification of paraarticular tissues in the area of the medial epicondyle of the femur.
Clin., rentgenol, and pathoanatomical picture of the disease with its characteristic calcification of the tibial collateral ligament of the knee joint was described in 1905 by Pellegrini. In 1908, Stida published 5 similar observations. He believed that the pericondylar shadow on the radiograph appears as a result of an avulsion fracture of the epicondyle of the femur after injury or a sharp contraction of the adductor magnus muscle of the femur, but this was not subsequently confirmed.
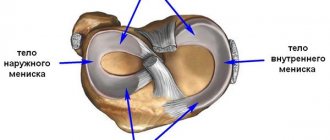
The disease is observed in people of both sexes, mainly men aged 25-45 years. It usually develops after a direct blow to the area of the medial condyle of the femur, forced abduction of the tibia, or a sharp uncoordinated contraction of the adductor muscles of the thigh. The injury is accompanied by hemorrhage into the adductor magnus tendon or tibial collateral ligament. At the site of hemorrhage over time, as a result of periosteal ossification or metaplasia of connective tissue elements, calcification or ossification may develop (see Ossification). Microscopically, the area of ossification is a bone tissue consisting of thin plates, between which there are wide bone marrow spaces.
The main symptoms of P.—Sh. b.—dysfunction of the limb, pain in the area of the medial epicondyle of the femur during movements in the knee joint and palpation, prolonged swelling of the knee joint, limitation of its mobility, and later atrophy of the thigh muscles. For diagnostic purposes, an x-ray examination is performed. After 3 weeks after an injury, radiographs of the knee joint area reveal a bone shadow in the shape of a bracket, sickle or triangle in a typical location - at the upper edge of the medial epicondyle of the femur parallel to its cortex, separated from the epicondyle by a light gap (Fig.).
Differential diagnosis is made with a marginal fracture of the femoral condyle or avulsion of the cortical plate by the tendon of the adductor magnus muscle. These injuries are detected immediately after the injury, and a defect is identified on the condyle corresponding to the site of the avulsion of the bone fragment.
The wedge, the picture, is similar to the epicon di lit of the femoral condyle, but with it there are no rentgenol, signs of the disease.
In the acute stage of the disease, immobilization of the limb with a plaster splint for 2 weeks is indicated. Diathermy, electrophoresis with novocaine, diadynamic Bernard currents, and ultrasound provide a good therapeutic effect. In advanced cases, 3-4 injections of 15-20 ml of 1% novocaine solution into the area of the epicondyle around the calcified area or hydrocortisone with novocaine are recommended with an interval between injections of 3-4 days. It is extremely rare, when long-term conservative treatment is unsuccessful, removal of ossificate with careful hemostasis is indicated.
After surgery, in some cases, a new ossification is formed at the site of the removed one.
The prognosis is favorable, treatment leads to the restoration of limb function, and sometimes the reverse development of calcification is detected by X-ray.
Prevention of the disease consists of timely and complete treatment of injuries to the knee joint.
Bibliography:
Korzh A. A. Heterotopic traumatic ossifications, p. 91, M., 1963; Pellegrini A. Ossificazione traumatica del legamento collaterale tibiale dell' articolazione del ginocchio sinistro, Clin. moderna, v. 11, p. 433, 1905; Stieda A. t)ber eine typische Verletzung am unteren Femurende, Langenbecks Arch. klin. Chir., Bd 85, S. 815, 1908.
Source xn--90aw5c.xn--c1avg
Diagnostic methods
A doctor may suspect Pellegrini-Stied disease of the knee joint after a physical examination and palpation of the affected area. To confirm the diagnosis, the patient is prescribed an X-ray examination in several projections simultaneously. In case of a pronounced pathological process, the image clearly visualizes excess bone growths in the area of the diseased knee joint. To determine the extent of the lesion, MRI and CT are required. A blood test is also required to determine the amount of calcium in the body.
Conservative therapy
Pellegrini-Stied disease can be treated in two ways. One of them is conservative, the other is operational. The first option is resorted to in the initial stages of the disease. Non-steroidal anti-inflammatory drugs are usually prescribed. In case of disease progression, exposure to novocaine blockades and hormonal agents is required. The doctor selects all medications, as well as their dosage, on an individual basis.
Simultaneously with taking medications, physiotherapeutic treatment is recommended to improve blood circulation in the affected area. The following procedures are particularly effective: electromassage, mud applications, magnetic laser procedures, ultrasound, electrophoresis.
The need for surgery
Treatment of Pellegrini-Stied disease of the knee joint by surgery is indicated when the volume of motor activity in the affected limb is reduced. During the operation, the doctor removes the overgrown bone and altered cartilage. The latter is replaced by the patient’s own similar elements taken from other parts of the body.
After surgery, a long period of rehabilitation is required to avoid relapse. The patient is prescribed hemostasis, electrophoresis with Lidaza, hydrokinesitherapy and a course of exercise therapy.
Bilateral gonarthrosis of the 3rd degree - how and with what is it treated?
Our readers successfully use Artreid to treat joints. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
The largest joint in our body is the knee. It allows the leg to move and helps in supporting body weight, and therefore it is the one that is most susceptible to various injuries and diseases. The most common cause of knee joint disease is natural aging of the body. This is why gonarthrosis most often appears in older people.
- Why do we suffer from this?
- How does the disease manifest itself at different stages?
- How is the disease diagnosed and treated?
Why do we suffer from this?
However, there are other factors that negatively affect the health of the knee joints:
- Firstly, these are any injuries that result in post-traumatic arthrosis: ligament rupture, meniscus injury, hip fracture, etc. Such injuries occur especially often in athletes.
- Secondly, the cause is diseases that cause the destruction of cartilage, such as chondromatosis or arthritis.
- Thirdly, a person may simply be genetically predisposed to this disease.
- Also, gonarthrosis often occurs in people who are overweight, have severe varicose veins, and in those who take drugs of a certain group for a long period.
Prognosis for recovery
With timely and competent treatment, as well as the patient’s compliance with therapeutic recommendations, the prognosis for recovery is favorable. After a rehabilitation period, the affected limb eventually regains its function. However, the possibility of the disease returning cannot be ruled out.
Prevention of relapse cases comes down to preventing knee injuries, eliminating intense sports and physical activity. Only with this approach can a recurrence of the disease or its transformation into a chronic stage be avoided.