Author of the article: Victoria Stoyanova, category 2 doctor, head of the laboratory at the diagnostic and treatment center (2015–2016).
Article publication date: 03/24/2014
Article updated date: 01/27/2020
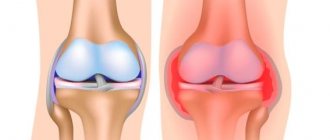
The human body is often compared to cars: the heart is the engine, the stomach is the fuel tank, and the brain sets the whole device in motion. Where are the shock absorbers in humans? Of course, in places that experience increased load: there are cartilaginous discs between the vertebrae, and in the knee joint there are two “shock absorbers” - the menisci. Lateral (external) and medial (internal). The results of degenerative changes in the menisci, although they will not stop the activity of the body as a whole, will definitely cause a lot of unpleasant sensations.
What are degenerative changes in the menisci?
Degenerative changes are anatomical damage to an organ resulting from injury, atypical joint structure or disease. Degeneration of the meniscus is most often the result of injury, sometimes not even obvious: one unsuccessful rotation of the tibia can cause damage to the cartilage disc, which is accompanied by severe pain.
Most often, due to the anatomical structure, the medial meniscus undergoes degeneration. If the outer cartilage, which cushions the movement of the knee joint, does not have rigid fixation and moves to any side if necessary, then the medial one is rigidly fixed in the joint, and its horns are in close proximity to the condyles. One sharp turn of the shin - and the meniscus does not have time to escape from the displaced process of the bone, the result is its damage or rupture.
Degenerative changes can be different:
- separation from the attachment point;
- rupture of the horns and body of the meniscus;
- excessive mobility as a result of rupture of the intermeniscal ligaments;
- cyst - the formation of cavities filled with fluid inside the cartilage;
- meniscopathies are dystrophic changes that develop under the influence of minor injuries, as well as as a complication of gout, osteoarthritis, rheumatism, tuberculosis and a number of other diseases.
Mechanism of development of degenerative joint lesions
The functioning of the joint depends on the condition of the cartilage. In the center the cartilage has a hyaline base; at the periphery it is fibrous. The thickness of the hyaline part is from 1 to 6 mm. Cartilage cells, chondrocytes, produce thin fibrils, threads that intertwine in different directions and form cartilage. The cells also synthesize chondrin, a lubricating fluid.
In a newborn, the tissue fluid of cartilage includes 75-80% water. In an adult, the normal level is 55-65%. During aging, during degenerative changes in the joints, this figure drops below 50%. Under such conditions, primary cartilage lesions develop, which, if nothing is done, spread first to the joint capsule and then further.
The main cause of degenerative changes in joints is moisture deficiency.
Characteristic symptoms
If you are haunted by aching pain in your knee, which either disappears or appears with renewed vigor, you can already assume that there are changes in the meniscus. About 90% of pathologies of the knee joint are caused by damage to the “shock absorber”.
Symptoms largely depend on the nature of the pathology. Ruptures are accompanied by severe pain, blockade of the leg in a bent state and swelling. With serious damage to the medial meniscus, hemorrhage into the joint cavity often occurs - hemarthrosis. Significant swelling and severe pain are also characterized by meniscal cystosis.
Tears and detachments from the attachment site are often chronic in nature and are manifested by periodic pain and a feeling of impediment in movement.
There is a diagnostic test: go up and down stairs or slopes. With pathology of the meniscus, the pain in the knee intensifies when moving down.
Secondary degenerative-dystrophic transformations in the medial meniscus, that is, those arising due to other pathologies of the body or diseases, are also characterized by a chronic course. Often in such cases there are clicks and rolling* of the joint during movement after a long period of rest, and sometimes there is pain in the knees. The increase in symptoms occurs gradually as the cartilage layer thins and salts or uric acid crystals accumulate in it (the latter in case of gout). In the absence of adequate treatment, the final stage of meniscopathy becomes contracture - a stable violation (limitation) of joint mobility.
* Rolling – sensations of pathological mobility, instability and displacement of the articular surfaces of bones.
The following symptoms are common to all types of meniscal degeneration:
- soreness,
- swelling,
- blockage of the joint in a bent position or sensation of a foreign body in the knee,
- clicks and crunches,
- numbness of the knees after a long period of inactivity.
Structure of the meniscus of the knee joint
The meniscus is a cartilage-like formation inside the knee joint that performs a shock-absorbing and protective function. It has a crescent shape and is located between the articular surfaces. There are two of them in each knee, namely:
- Lateral (also known as external) – is less likely to be injured, but is more mobile.
- Medial (otherwise called internal) - most susceptible to injury, less mobile compared to the external.
The structure of the knee joint. Internal and external meniscus of the knee.
The strength and elasticity of this cartilage layer is provided by collagen fibers located radially. Given the crescent shape, each of them has two horns: anterior and posterior. The inner surface has a worse blood supply than the outer surface, facing the joint capsule. This affects the healing processes at different locations and treatment tactics, respectively.
Causes of degeneration
The anatomical features of the location and structure of the menisci determine the high incidence of pathologies both among young people and among mature people. Most often, athletes, ballerinas, dancers suffer from ruptures, damage and cystosis - that is, people who are in constant motion and experience high loads.
Other possible reasons:
- dysplasia – abnormal formation of the knee joint;
- gout, syphilis, tuberculosis, rheumatism and other diseases that can affect joints;
- sprains of ligaments, as well as their incorrect formation;
- flat feet (low shock absorption of the foot is compensated by increased load on the knee);
- high physical activity;
- excess weight.
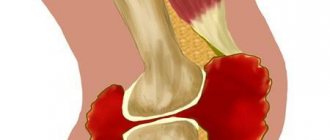
Types of meniscal tears
Types of meniscal tears of the knee joint.
The meniscus is damaged both in isolation and in combination with other anatomical formations. When exposed to an external force, the rupture is called traumatic. It is usually found in athletes. If changes occur due to arthrosis, this is a degenerative damage that is more common in people of the older age group. Moreover, both of these options are often multiple, affecting articular cartilage. They are, one way or another, interconnected and one does not exclude the other or is its consequence.
A distinction is made between complete and partial rupture. In the first case, free fragments become mobile and can cause blocking (“jamming”), namely the occurrence of impingement syndrome. A sharp immobilization occurs, which can only be eliminated by specialists and mainly by surgical means. If the part where there is active blood circulation is damaged, hemarthrosis is most likely - the accumulation of blood inside the joint. It manifests itself externally by a rapid increase in swelling.
Diagnostics
In case of acute injuries to the meniscus, there is usually no doubt - blockade of the knee in a characteristic position, pain and clicks when straightening allow a correct diagnosis to be made in 90% of cases.
It is not always possible to determine degenerative-dystrophic transformations during examination due to the absence of clear symptoms and, often, a positive reaction to special tests. In such cases, instrumental research methods are resorted to:
- MRI allows you to obtain a three-dimensional image of all tissues of the knee: the articular surfaces of the bones, the ligamentous apparatus and the joint itself.
- During arthroscopy, an endoscope is inserted into the joint cavity through a miniature incision, with the help of which the condition of the tissues and synovial fluid is monitored (on a monitor).
First aid for meniscus injury
When a meniscus ruptures, a sharp pain occurs in the first minutes, which intensifies when the leg is extended.
If pain occurs as a result of an injury, care must be taken to ensure that the victim gets to a medical facility as soon as possible. The injured leg must be immobilized. To avoid bending during transportation, it is better to apply a splint or splint. It is strictly not recommended to eliminate the blockade, if it occurs, on your own. In order to alleviate the condition and avoid the increase in swelling, cold is applied to the knee, for example, an ice pack. Aerosol coolers, used more often among athletes, are optimal. As a last resort, you can offer the victim a non-steroidal anti-inflammatory drug. The sooner the patient gets to the clinic in compliance with all transportation rules, the less complications can be expected.
Treatment methods
Therapy for degenerative changes in the menisci completely depends on the nature of the damage. Acute injuries serve as a direct indication for the use of conservative treatment methods:
- First of all, a puncture of the joint is performed, eliminating its swelling and restoring mobility. Sometimes several procedures are required, since active exudation (secretion of inflammatory fluid) in the joint lasts up to three to four days.
- Analgesics are prescribed, preference is given to narcotic drugs (Promedol and its derivatives), because other drugs in this case, as a rule, are not able to relieve the patient of pain.
- Chondroprotectors provide the body with the necessary substances to restore the damaged area of the meniscus.
- Anti-inflammatory drugs.
- At the rehabilitation stage, physiotherapeutic methods are used as an auxiliary means - ozokerite, UHF, iontophoresis, shock wave therapy.
- For 14 days, a splint is applied to the straightened leg to secure the joint in the required position.
In case of ruptures, surgical intervention is indicated: instruments are inserted into the knee joint through two miniature incisions and the damaged area is sutured. Serious injury may require the cartilage lining of the joint to be removed and replaced with an artificial one. All surgical procedures are performed only after signs of inflammation have subsided.
Chronic dystrophies, joint dysplasia and abnormal development of the ligamentous apparatus require exclusively surgical treatment.
If the cause of degeneration is chronic diseases, such as rheumatism and gout, along with surgical methods, the underlying disease is also treated (diet, immunocorrectors and other methods).
Degenerative transformations of the menisci are a fairly common pathology that requires immediate consultation with a specialist. The future functioning of the joint depends on the timeliness of treatment, and delays can cause the spread of degenerative processes to other elements of the joint. Therefore, do not delay your visit to the doctor, take care of yourself and be healthy!
Is rehabilitation necessary?
Of course, it is necessary, especially after operational activities. What is the purpose of rehabilitation:
- restoration of muscle tone of the injured limb;
- normalization of blood circulation;
- reduction of pain syndrome;
- restoration of full function of the knee joint.
A set of exercises and the frequency of their implementation are developed individually for each patient, guided by the severity of the injury or the complexity of the pathology. Moreover, after surgery, exercise therapy begins 2 months after the operation, and with conservative treatment - 15-20 days after the injury.
Damage to the posterior horn of the medial meniscus - treatment
After an objective diagnosis has been carried out, determining the location and severity of the violation of the integrity of the cartilaginous structures of the joint, the doctor prescribes a comprehensive treatment. It includes several areas of action, which include conservative therapy, surgical intervention, and subsequent rehabilitation. Mostly all activities complement each other and are assigned sequentially.
Treatment without surgery
If partial damage to the posterior horn of the medial meniscus (grade 1 or 2) has been diagnosed, conservative treatment is possible. It includes the use of drugs of various pharmacological groups (non-steroidal anti-inflammatory drugs, vitamin preparations, chondroprotectors), the performance of physiotherapeutic procedures (electrophoresis, mud baths, ozokerite). During therapeutic measures, functional rest for the knee joint must be ensured.
Meniscus arthroscopy
At the SportClinic, meniscal arthroscopy is performed by the best traumatologist-surgeons in Russia.
Surgical treatment of meniscal tears of the knee joint is carried out using arthroscopy. This is a minimally invasive and effective method for diagnosing and treating such pathologies today. It is low-traumatic in relation to surrounding tissues. The high resolution of the arthroscope camera provides a detailed image, which is displayed in an enlarged format on the screen, which ensures the accuracy of the examination during arthroscopy. Immediately after diagnosis, all surgical procedures are performed. In case of a rupture, this means resection or removal of the meniscus, and in case of minor damage, it can be sutured.
Arthroscopic suturing of the meniscus
By connecting the torn edges, mainly from a fresh injury, it is possible to achieve their fusion and restore the integrity of the damaged structure. This occurs most successfully after a rupture in the part that faces the joint capsule and is better supplied with blood. During arthroscopy, special clamps are introduced into the joint, which the doctor places on the torn edges, having previously connected them. This method is especially relevant for athletes and people who regularly expose their knee to fairly heavy loads. The effectiveness of the technique is high, success is achieved in 90%. Arthroscopy is a low-traumatic and easily tolerated operation. If you follow the recommendations of specialists during the rehabilitation period, it is possible to restore your previous shape in the shortest possible time.
Meniscus resection
If reconstruction is not possible after a rupture, then resection is performed through arthroscopy - damaged and torn elements are removed. The remaining healthy tissue is preserved and the surface and edges are sanded for best function. After which, the leg returns to active movements without significant consequences. As a rule, if most of the meniscus was preserved, then the functions of the knee do not suffer in any way in the future; after several weeks of a rehabilitation course, the patient is allowed to participate in sports training.
Complete arthroscopic removal
Complete removal or meniscectomy is a common operation and is also performed using an arthroscopic technique. The meniscus, previously affected by arthrosis, literally falls into pieces under traumatic influence. Sometimes a complex mechanism of injury leads to its loss. The decision to remove is usually made during arthroscopy. The limb after such operations functions stably, provided proper recovery and moderate loads. Further, it is recommended to be constantly monitored by a doctor to prevent the development of arthrosis.