Endoprosthetics is a surgical treatment aimed at restoring a joint damaged by degenerative-dystrophic processes. Rehabilitation measures after knee replacement are sometimes more important for the patient’s health than the operation itself. The success of surgical intervention, the usefulness of the motor abilities of the joint and the quality of future life depend on rehabilitation. To speed up the process of restoring joint mobility, it is important that the attending doctor or exercise therapy instructor has knowledge of the principles of biomechanics and ontogenesis, according to which the human body is a single mechanism, and with regular systematic influence on certain points or organs, the condition of a previously damaged and operated knee improves, the patient learning new movements.
Types of endoprosthetics
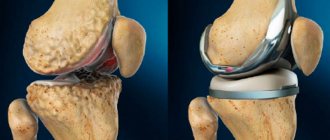
Knee replacement surgery is the main way to avoid being in a wheelchair. Surgical intervention is performed when complex pathology can no longer be eliminated. Depending on the extent of damage, the following types of endoprosthetics are distinguished:
- Total – complete replacement of the knee joint with a prosthesis. The operation is performed in case of tissue damage of 70%.
- Partial – replacement of a specific area with an implant. A gentle technique is used if the joint is less than 50% damaged.
Damage to the knee joint can be caused by a jump from a height, chronic arthrosis, arthritis, gonarthrosis, or a blow to the knee. Bone and cartilage tissue is destroyed due to impaired blood flow and trophism.
Preoperative preparation
The main complications of endoprosthetics are the development of contractures, muscle atrophy, vein thrombosis or synovitis (accumulation of excess fluid in the joint capsule). The reason for their appearance is considered to be a lack of preparation for surgery. The fact is that knee replacement surgery is most often performed on elderly people whose health has been compromised by chronic diseases.
To prevent the development of complications during the rehabilitation period, you need to prepare for surgery. The patient must undergo a course of physiotherapy, exercise therapy and massage. They will improve blood circulation in the knee joint and increase muscle tone. As a result, rehabilitation after surgery will be more successful. In addition, it is necessary to improve the performance of the hands, since they will take on the main load after the operation. The following types of physical activity are recommended:
- swimming;
- aqua gymnastics;
- Nordic walking;
- cycling or exercising on an exercise bike.
Rehabilitation after endoprosthetics
The main task of the recovery period after surgery is the gradual return to the patient’s ability to move independently. Rehabilitation after knee replacement consists of three stages: early (3 weeks), late (up to 6 months) and long-term (up to a year). Postoperative recovery is accelerated by physiotherapeutic procedures and physical therapy. The rehabilitation program is developed individually, taking into account the reason for knee replacement, the age and health of the patient.
Rehabilitation after endoprosthetics performs the following tasks:
- relieving pain and swelling;
- improvement of blood circulation and tissue trophism;
- improving the mobility of the prosthesis;
- relief of the inflammatory process;
- muscle strengthening;
- restoration of range of motion.
CPM therapy in the early postoperative period
From the first day after endoprosthetics, Artromot or Kinetec mechanotherapy devices are used for passive development of the knee joint. They allow you to control the intensity of physical activity: amplitude, speed and frequency are individually selected. The flexion angle is increased by 10° daily until 90° is reached in independent flexion. The electronic remote control allows you to easily set the speed and pauses in stretching the joint. The display shows the achieved extension and flexion value.
The design of CRM simulators is anatomically correct, based on the physiology of the functioning of the knee joint. Constant movement promotes rapid recovery of injured tissue, minimizing the likelihood of contractures and stiffness. During the session, patients note complete muscle relaxation and absence of pain. The advantage of a mechanical apparatus is the ability to work out a joint 3-4 times a day, which cannot be done through physical therapy exercises. Next, the artificial joint is developed using special installations - orthotics. They restore balance and coordination of movements. The complex allows you to assess the functional state of joints and muscles. The Biodex device has the following features:
- passive mode – a change in speed is provided to overcome the stretch reflex and further assist in movement;
- isometric mode – to increase static muscle strength in the presence of pain;
- isotonic mode – for active training of the osteoarticular system.
Using the control panel, you can control or change various parameters: speed, torque, range of motion. The Biodex rehabilitation complex allows you to combine dynamic and static muscle loads.
How can a foreign patient make an appointment for surgery for a torn meniscus?
To begin with, Gelenk Clinic specialists will need current MRI and X-ray images to assess the condition of the knee joint. Once you submit the required documents to us through our website, we will send you patient information and cost estimates within 1-2 days. .
Foreign patients can make an appointment for meniscus tear surgery in a short time. We will be happy to assist in obtaining a visa after the advance payment indicated in the estimate has been received into our account. If a visa is not issued, the amount received is returned to you in full.
Due to sometimes long flights, we try to keep the time between the first examination and surgery to a minimum. During outpatient and inpatient treatment of the knee joint, you will be able to use the services of qualified medical personnel who speak several foreign languages (eg English, Russian, Spanish, Portuguese). Payment for a translator (for example, into Arabic) is carried out separately. We also organize transfers, we can book a hotel room and tell you how to spend time in Germany for you and your relatives.
Send request
Physiotherapy
The exercise therapy program is aimed not only at developing the knee, but also at restoring neural connections. The instructor controls the duration and intensity of classes. Fitness balls, dumbbells, expanders and other sports equipment are used. Myofascial release (kinesitherapy) is performed using special rollers. Exercises are performed on slings. They combine simultaneous unloading of some muscles and targeted training of others.
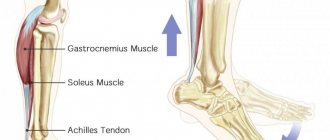
A course of physical therapy for postoperative rehabilitation should alternately affect all areas of the lower limb and include the following exercises:
- Flexion and extension of the ankle joint. First, the sock is pulled towards you, and then in the opposite direction. The exercise is repeated 10 times. It is recommended to do it every 10 minutes throughout the day.
- Taking your leg to the side while lying in bed. The limb is moved to the side, sliding along the surface, then returned to its place. In this case, the toe of the foot should be directed upward.
- Knee flexion to 90° followed by extension. The exercise is performed in a horizontal position. The leg is smoothly pulled towards you until a right angle is reached at the knee. Then the limb is returned to its original position - pulled forward, sliding along the surface. Start with a small amplitude, gradually increasing it.
- Tension of the quadriceps femoris muscle and activation of the limb. In a supine position, the leg is raised up to a level of 30 cm from the surface. She is held in this position for 5-8 seconds. Do 10 approaches with an interval of 2 minutes.
- Alternate contraction of the gluteal, posterior and anterior thigh muscles. This gymnastic technique normalizes tissue trophism and increases muscle tone.
5-6 days after the operation, they begin to master walking on parallel bars, a treadmill or a step machine. A bicycle ergometer is used, equipped with an electronic system to control the progress of the workout. The built-in computer allows you to adjust the speed, time and distance. The number of approaches is determined by the doctor. Gradually increase the time spent on your feet.
To increase the effectiveness of physical therapy, physiotherapeutic procedures are prescribed: shock wave therapy, ultrasound, electrical muscle stimulation, magnetic and laser therapy. The rehabilitation center offers water classes, massage courses, mud therapy and balneotherapy. Physiotherapy improves blood circulation, stimulates metabolic processes, and calms the nervous system. To improve regeneration, manual therapy, classic manual and lymphatic drainage massage are used.
Late period rehabilitation
After discharge, the patient uses crutches for 5-7 weeks, then begins to learn to walk independently. While lying down, you can do the following:
- bend your knees, lying on your stomach;
- lie on your back and do a plank, resting on your healthy foot and shoulder blades.
While sitting, it is recommended to do the following exercises:
- simultaneous flexion and extension of the toes;
- rotation of the feet clockwise and counterclockwise;
- raising your leg without bending your knee;
- swinging limbs in the air for several seconds.
Exercises performed while standing:
- bending the leg forward and backward, leaning on a chair;
- raises on toes;
- “sliding” along the wall;
- half squats with support;
- back lunges;
- rolling from heel to toe.
The intensity of the exercises is increased gradually. The number of repetitions is no more than 15 times. Rehabilitation doctor S. Bubnovsky, who developed a set of exercises, recommends doing everything slowly and avoiding sudden movements. The main condition is that there should be no pain or swelling. 1.5 months after joint replacement surgery, you can begin exercise therapy.
Recovery after knee meniscectomy
In the rehabilitation clinic, after removal of the meniscus, patients are prescribed the following physiotherapeutic procedures:
- electromyostimulation;
- laser treatment;
- UHF therapy;
- ion-galvanization;
- extracorporeal shock wave therapy;
- magnetic therapy;
- hot paraffin treatment (in the later stages of rehabilitation).
Exercise therapy and physiotherapy help relieve spasms from tense muscles, increase the tone of atrophied and weakened muscle fibers, and activate blood flow and microcirculation in the lower limb. Under the influence of physiotherapeutic procedures, metabolism in the joint is stimulated, swelling and pain are relieved.
For six weeks after a meniscectomy, there is still a risk of blood clots. In the early postoperative period, specialists at the rehabilitation clinic apply a bandage to the lower extremities with an elastic bandage, and in the later period they recommend that patients use compression stockings. The degree of compression of medical devices is selected by a rehabilitation specialist. It takes into account the extent of surgery and the predisposition to blood clots.
Long-term recovery period
The goal of the final stage of rehabilitation is the complete restoration of movements and preparation for a full life. At a later stage, you are allowed to visit the gym. You can engage in a sport with moderate loads: Nordic walking, swimming, cycling. Rehabilitation at the final stage includes the following daily exercises: “scissors”, “bicycle”, walking on bent legs with the help of support.
Do not lift heavy objects or subject the joint to high physical stress. It is prohibited to play football, basketball or volleyball. If the doctor's recommendations are followed, performance returns 1.5-3 months after surgery.
What type of anesthesia is used for surgical treatment of a meniscus tear?
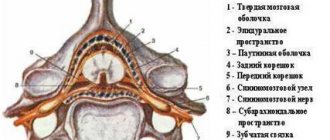
Typically, surgery for a torn meniscus is performed under general anesthesia. To avoid risk, there is the possibility of spinal anesthesia. To do this, the surgeon injects an anesthetic into the spinal canal of the lumbar spine. In this case, the patient is fully conscious. What type of anesthesia is most suitable for the patient is determined during a conversation with the anesthesiologist. Our doctors are true masters of their craft, who during your appointment will offer you the best method that meets all the indicators of previous examinations.