In our Center, we can offer a treatment method for arthrosis of the sacral iliac joints using comprehensive programs that include radiofrequency treatment , blockades , and drug therapy . This approach allows you to relieve pain for a long time, and additional recommendations will help you get rid of this disease! We will answer all your questions by phone. You can also ask a question by filling out the request form below.
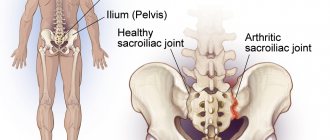
Arthrosis of the sacroiliac joints is an inflammatory change in the joint. It is formed by the articular surface of the sacrum and the iliac bone of the pelvis, and is quite strong due to short ligament bundles (the strongest).
Ligaments: Proper ligaments of the joint
- Ventral (anterior)
- Dorsal (posterior)
And additional
- The iliopsoas ligament arises from the L5 transverse process of the lumbar vertebra and attaches to the iliac crest.
- The sacrospinous ligament runs from the spine of the ischium to the sacrum.
- Sacrotuberous ligament -
Accessory ligaments do not belong to the sacroiliac joint. They fix the pelvis to the spine.
The main function of the sacroiliac joint is to soften the load transmitted from the legs to the spine.
Where is the sacroiliac joint located?
The sacroiliac joint is a large, inactive joint formed by the ear-shaped surfaces of the sacrum and ilium, covered with dense fibrous cartilage. The sacroiliac joint is the most mobile in young children. With age, due to increasing vertical loads, the joint becomes stronger - ridges and depressions form on the articular surfaces, overlapping each other. The stability of the joint is also ensured by powerful ligaments, which are stronger than the pelvic bones.
The main function of the joint is to absorb shock loads, support the spine, and rotate the belt of the lower extremities relative to the spine within 2-18 degrees. The joint is also directly involved in walking.
Symptoms of sacroiliac arthrosis
The onset of the pathological process often goes unnoticed, as it does not manifest itself with specific symptoms. The first manifestations of the disease are associated with the destruction of cartilage tissue. Over time, the patients' condition worsens, they complain of:
- painful sensations in the lumbosacral spine, in the buttocks area, which intensify during bending, sitting, walking or physical activity;
- muscle tension in the sacral region;
- stiffness of movements, decreased amplitude;
- crunching sound when turning the body or bending over
- change in gait;
- frequent urge to urinate;
Patients characterize the pain as pulling, aching, which at times radiates to the groin area, perineum, buttocks and legs.
Lack of treatment contributes to the worsening of the inflammatory process. The skin over the affected joints turns red and becomes more sensitive, the soft tissues become swollen due to impaired local circulation. Osteophytes form on the surface of the joint. In severe cases, patients completely lose the ability to move without assistance.
Diseases of the sacroiliac joint
Sacroiliitis is inflammation of the sacroiliac joint. Serves as a characteristic sign of rheumatoid arthritis and other joint pathologies, ankylosing spondylitis. Sacroiliitis is one of the diagnostic criteria for Crohn's disease and ulcerative colitis. Inflammation can also be a sign of brucellosis, degenerative-dystrophic phenomena (arthrosis, osteoarthritis). Sacroiliitis leads to pathological mobility (instability) or ankylosis (pathological fusion) of the sacroiliac joint. Dysfunction of the joint becomes a source of constant pain.
The area of the sacroiliac joint can be affected by tumors, metastases in the pelvic bones, or an infectious process (osteomyelitis).
Treatment of arthrosis of the iliosacral joint
The effectiveness of treatment largely depends on how early it was started. Along with conservative therapy, radiofrequency ablation of the joint is prescribed, in a set of measures that together help eliminate the inflammatory process and stop the destruction of the joint. It includes:
- drug therapy;
- physiotherapy;
- manual therapy;
- Exercise therapy.
In case of exacerbation of the disease, bed rest is recommended until the severity of pain decreases. In the future, patients are advised to give up heavy physical work, sports and long running. But moderate physical activity is an integral part of the fight against arthrosis of the sacroiliac joint. When working in a sedentary or standing position, it is important to take regular breaks and walk around.
A vertebrologist may recommend that the patient wear a special orthopedic corset. It will help reduce stress on the back muscles and pressure on the affected joints. The bandage is selected individually by the doctor. It should be worn for several hours during the day.
If conservative treatment is completely ineffective or advanced forms of arthrosis have led to the formation of osteophytes, patients can be helped surgically. This will protect the person from pain, preserve his ability to work and avoid disability.
Drug therapy
In order to relieve pain and eliminate the inflammatory process, patients are prescribed drugs from different groups. They, as well as the route of administration (oral, intramuscular, intravenous) and doses are selected individually, based on the stage of development of arthrosis of the sacroiliac joint. In this case, existing concomitant diseases must be taken into account.
Patients are advised to use:
- NSAIDs – used for moderate pain. In addition to the analgesic effect, they have anti-inflammatory properties. They are most often used in the form of drugs for oral use, but if they are ineffective, intramuscular injections can be prescribed. The negative side of drugs in this group is their negative effect on the condition of the mucous membranes of the gastrointestinal tract with long-term use.
- Corticosteroids - indicated for severe inflammatory processes that cannot be treated with NSAIDs. They are prescribed in short courses and have a powerful anti-inflammatory effect.
- Muscle relaxants are drugs that relieve muscle spasms. They are used to eliminate reflex spasms caused by pain. This reduces the intensity of pain and improves blood circulation in the area.
- Chondroprotectors - drugs in this group are designed to stop the destruction of cartilage tissue and improve its structure. They are intended for long-term use.
- Vitamin complexes – help increase the effectiveness of drugs from other groups and normalize metabolic processes.
- Local remedies in the form of ointments, creams or gels most often contain NSAIDs and are used to relieve mild pain.
Lidocaine or novocaine blockades can quickly relieve unbearable pain. They are performed exclusively under completely sterile conditions, i.e. in a medical facility. The essence of the procedure is to inject anesthetic solutions into precisely defined points in the sacral area. The manipulation brings relief within 2–5 minutes. It can also be carried out at the SL Clinic.
But the blockade cannot be performed during pregnancy or the presence of pustular rashes on the skin in the projection of the affected joint.
Physiotherapy
Physiotherapeutic procedures that are correctly selected in terms of duration and frequency of implementation significantly increase the effectiveness of drug therapy and can reduce the intensity of pain. Patients are recommended:
- electrophoresis with the introduction of drugs from the NSAID group - the procedure involves the introduction of drugs through a weak electric current directly into the lesion;
- laser therapy – the thermal effect of the laser activates the processes of regeneration of cartilage tissue cells;
- reflexology - influencing biologically active points helps improve blood circulation and reduce pain;
- Magnetic therapy - a method that helps reduce the intensity of pain and reduce the rate of degenerative processes.
Usually a course of procedures is prescribed, consisting of 10–12 sessions. They can only be carried out during remission. Contraindications to physiotherapeutic treatment are serious diseases of the cardiovascular system, severe renal or respiratory failure, febrile conditions, and epilepsy.
Manual therapy
Manual therapy sessions conducted by a specialist, taking into account the characteristics of the patient’s condition, can not only activate blood circulation in the area of the sacroiliac joint and thereby improve tissue nutrition, but also slow down the course of degenerative processes.
The procedures are carried out in courses. They should be started only after the acute phase of arthrosis is completed.
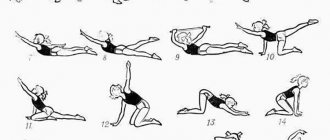
Exercise therapy
Although rest helps relieve pain, a specific set of exercises can be even more helpful. Moreover, physical therapy plays an important role in the conservative treatment of arthrosis of the sacroiliac joint. Depending on the stage and general condition of the patient, a training schedule and workload are individually developed for him. It is usually necessary to do therapeutic exercises daily for 20–30 minutes.
The first sessions of exercise therapy are recommended to be carried out under the supervision of a specialist. This will help not only to master the necessary set of exercises, but also to maintain an optimal rhythm when performing it. In most cases, patients are prescribed body turns, bends, rotations, etc. When performing any exercise, it is important to avoid sudden movements and overexertion, and if pain occurs, you should definitely consult a doctor.
Swimming and yoga have a beneficial effect on the patient's condition. But they are only permissible outside of exacerbation of arthrosis.
Surgical treatment of arthrosis of the sacroiliac joint
In some cases, the only way for patients to get rid of excruciating pain and avoid long-term back pain and joint pain is surgical treatment of arthrosis. It is indicated when attempts to cope with the disease using conservative methods are unsuccessful, as well as in severely advanced cases, i.e., stage 3 arthrosis of the sacroiliac joint.
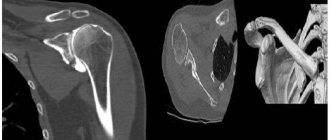
The essence of surgical intervention depends on the nature of the existing changes. Radiofrequency ablation of nerve endings can be used to eliminate pain. Its essence consists in introducing a special electrode through a pinpoint puncture of soft tissue directly to the pain-causing nerve and its destruction by the generated thermal energy.
The procedure in most cases leads to immediate pain relief. In other situations, there is a progressive decrease in their intensity over 6-8 weeks. After it is completed, the patient can almost immediately move independently and return home on the same day.
If irreversible changes have occurred in the sacroiliac joint, the surgeon may recommend arthrodesis to the patient. The operation is performed on both sides in 2 stages:
- With the patient lying on his stomach after treatment of the surgical field, an incision about 2 cm long is made and a channel is formed into the articulation cavity through the posterior portion of the sacroiliac ligament. Using special instruments, a thorough curettage is carried out, i.e., cleaning the articular surfaces. The cavity is washed with solutions of antiseptics and antibiotics and the wound is sutured. Drainage is inserted into it and an antiseptic bandage is applied.
- The patient is turned over onto his back and a cushion is placed under the lumbar curve. An incision up to 4–5 cm long is made along the iliac crest, through which a bone canal is formed in the crest using an awl. Also, 2 more channels are created at a distance of 1–2 cm from the first. 3 rods are inserted into them and the rigidity of the installation is carefully controlled. An external fixation device is mounted on them and the necessary compression parameters are set.
During the rehabilitation process, surgeons change compression modes, thereby achieving effective arthrodesis of the sacroiliac joint. Patients can get up already on the second day after surgery. In the absence of adverse events, he can stand up independently and begin learning to walk. A control x-ray is performed on day 5 and, if there are no complications, the patient can return home, receiving detailed recommendations on the specifics of recovery.
Every 2–3 days, the patient must independently or with the help of relatives carry out dressings and take prescribed medications. After 8–10 weeks, a repeat X-ray examination is performed and part of the external fixation device is removed. After this, the patient needs to walk for about an hour, leaning on crutches and without them. In the absence of pain, final dismantling is performed, which leads to normalization of range of motion.
You can undergo conservative and surgical treatment for arthrosis of the sacroiliac joint at the SL Clinic. Our highly qualified vertebrologists are able to accurately determine the causes of pain and stiffness of movement, and select the optimal treatment tactics, which are sure to give positive results.
In severe cases, you can receive professional surgical care from us and regain the ability to move calmly. We provide medical services at the level of well-known clinics in Germany, Israel and the Czech Republic, but at the same time make them accessible to a wide range of patients. The cost of all types of services, including specialist consultations, blockades, surgical treatment, is given in the price list. Entrust your health to us, and we will do everything possible so that pain does not bother you anymore.
Indications and contraindications for MRI of the sacroiliac joints
MRI of the sacroiliac joint is recommended if the patient has the following complaints:
- pain in the lower back, in the buttocks, sacrum, radiating to the thigh - a sign of sacroiliitis and instability of the SIJ;
- the pain intensifies when a person stands or sits for a long time, when turning the body, walking for a long time, when trying to change position, or get up from a chair;
- a characteristic symptom is the occurrence or intensification of pain when climbing stairs, transferring the weight of the body from one leg to the other, trying to roll over while lying in bed;
- limited mobility of the spine;
- the presence of space-occupying formations, edema, swelling, nodes and bumps, determined visually or by touch.
MRI of the sacroiliac joint is prohibited if there are contraindications:
- pacemakers, defibrillators, cochlear implants and other medical devices implanted into the patient’s body are an absolute contraindication, unless the implant is made of MRI-compatible materials;
- Magnetic resonance imaging is not performed in patients under 5 years of age and in pregnant women in the first trimester of pregnancy;
- foreign bodies made of magnetic metal are also an absolute contraindication for MRI (this especially applies to small pieces of metal in the eyes, steel clips on brain vessels, fragments and fragments of ammunition);
- patient weight more than 130 kg and/or body circumference more than 150 cm is an obstacle to research due to inconsistency of anthropometric data and the size of MRI equipment;
- severe claustrophobia.
Department of Traumatology and Orthopedics
article in PDF format
QUOTE LINK:
Chensky A.D., Slinyakov L.Yu., Cherepanov V.G., Ternovoy K.S., DIAGNOSIS AND TREATMENT OF SACRIOLIAC JOINT SYNDROME // Department of Traumatology and Orthopedics. 2015.№ 2(14). pp. 12-16 https://jkto.ru/id-3/id-2/2-14-2015-/id-3.html https://elibrary.ru/item.asp?id=24356992
A. D. CHENSKY, L. Y. SLINYAKOV, V. G. CHEREPANOV, K. S. TERNOVOY
First Moscow State Medical University named after I.M. Sechenov, Moscow
One of the causes of pain in the lumbosacral spine is pathological processes occurring in the sacroiliac joint.
Under our supervision from 2009 to 2014. There were 385 patients with sacroiliac joint syndrome.
We carried out complex conservative therapy for pain caused by pathology of the sacroiliac joint. In 80% of cases, we were able to relieve pain for a long period (from 2 to 5 years) without resorting to radiofrequency denervation. But in some patients (20%), the pain syndrome was severe and recurrent. Due to the ineffectiveness of conservative therapy for this group of patients, the tactics of radiofrequency denervation of the sacroiliac joint were chosen, which made it possible to relieve pain in the sacroiliac joint in this category of patients in 100% of cases.
Key words: sacroiliac joint, pain syndrome, radiofrequency denervation.
The problem of pain occupies one of the central places in modern medicine and is the subject of large-scale multidisciplinary research. Currently, it is experiencing a period of intensive study, characterized by the extremely rapid emergence of new data, concepts, and theories, which sometimes do not even have time to receive proper semantic assimilation, both in theoretical and practical terms.
Among the many known syndromes and symptoms of various pathological conditions, the pathophysiological substrate of pain is the most common, disabling manifestation. Approximately one in five working-age members of society suffers from pain every year. Chronic pain syndromes, more often than the underlying diseases themselves that cause them, are the most common cause of disability in the most active part of the population. According to statistics from the World Health Organization, 40-80% of the adult population suffers from vertebrogenic pain syndromes during the period of most active labor activity in 25-55 years. Back pain often affects both workers and employees, regardless of their type of activity and qualifications, and therefore those who are engaged in work with little physical exertion are almost as vulnerable as those who are engaged in heavy work. Despite a number of studies conducted over the past decades on the problem of lumbosacral pain, it still remains relevant at present. This is confirmed both by statistical data on the prevalence of lumbosacral pain syndrome and by the existence of opposing views on such key issues as the etiology and pathogenesis of vertebrogenic pain syndromes of the lumbosacral spine. At the same time, the dominant group of specialists attaches primary importance to degenerative processes occurring at the level of the lower lumbar segments of the spine, as the cause of pain syndromes in the pelvic girdle and lower extremities.
One of the causes of pain in the lumbosacral spine is pathological processes occurring in the sacroiliac joint.
Pathological processes occurring in the sacroiliac joint were given importance back in ancient times. Hippocrates was the first to draw attention to the presence of mobility in the sacroiliac joint during childbirth in women. Subsequently, Ambroise Pare confirmed the presence of mobility in these joints not only in women, but also in men. Modern ideas about the pathology of the sacroiliac joints began to take shape at the end of the last and beginning of this century.
In 1911, Meisenbach drew the attention of doctors to the fact that one of the causes of pain in the lumbosacral spine may be processes occurring in the sacroiliac joint under the influence of mechanical factors, age-related changes and dishormonal changes, which would later be called “sacroiliac joint syndrome.” .
A number of authors emphasized the complex anatomical connection between the sacrum, ilium and lumbar spine at the beginning of the last century (Goldthwait, 1905; Brooke, 1928 et al.). They note that pathological posture or dysfunction of the lumbar spine can always be based on pathology of the sacroiliac joints. Also, in their opinion, the cause of sciatica is irritation of nerve endings due to changes in the ventral surface of the sacroiliac joint.
In the 20s of the last century, the sacroiliac joint was often looked at as the cause of sciatica, but with the development of the herneological theory, the diagnosis of the disease of the sacroiliac joint was actually consigned to oblivion by official medicine. French orthopedist Piedullu (1966) noted that limited mobility of the sacroiliac joints is the starting point of dysfunction of the lumbosacral spine.
Only this, in his opinion, contributes to the occurrence of lumbargic and sciatica syndromes.
According to Tonnis (1978), the diagnosis of intervertebral disc disease from this point on began to become too frequent and hasty. The author also notes that sacroiliac joint syndrome has the right to exist like other syndromes of vertebrogenic origin: “lumbalgic”, “cervicalgic”, “thoracolgic”, etc.
V.D. Chaklin and E.A. Abalmasova (1973) drew attention to the fact that the function of the spine, especially the lumbar region, should be considered in connection with the articulations of the pelvis and hip joints. The functional complex of the sacroiliac, hip joints and lumbosacral joint constitutes a single whole, a complex biological system consisting of a number of subsystems, with a clear hierarchical structure and subordination. Many connections allow this system to function as a single whole. When the function of all three components of the triad is disrupted, very severe functional disorders of the trunk, gait and sitting occur. They are of great importance for understanding the pathology and for constructing a treatment plan for diseases of the spine and hip joints, taking into account the mobilization of one or all components of the triad, then we can talk about the diagnosis and treatment of the “functional triad” syndrome, in which the sacroiliac joint plays an important role.
PC. Anokhin et al. (1976) propose a compensation rule, according to which functional reserves are activated only in conditions of dysfunction of the basic physiological mechanisms responsible for a given function. An example is degenerative-dystrophic lesions of the motor unit. Dysfunction within one joint leads to disruption of the entire biomechanical chain, compensatory loading of neighboring articular links. Further, the impaired function of physiological movement leads to deformation of the joints, which irreversibly leads to disruption of the mechanism of movement. Regarding sacroiliac joint syndrome, an isolated disorder can be regarded as the onset of subsequent multiple lesions of the joints and tissues involved in movement. Thus, it is possible to more accurately represent the role of the sacroiliac joint in the pathology of the lumbosacral spine.
It is well known that in 13% of patients with low back pain, its source is the sacroiliac joint (Maigne et al., 1996).
DonTigny (2007) states that every patient with low back pain originating from the sacroiliac joint has a discernible anterior rotational displacement (subluxation) of the ilium, and in most the pain resolves with manual adjustment.
The range of motion in the sacroiliac joint is small: less than 4 degrees of rotation and up to 1.6 mm of displacement (Sturesson et al., 1989; Sturesson et al., 2000).
With a long-term course of degenerative-dystrophic processes in the sacroiliac joint, manual therapy is often an insufficient method of treatment. Therefore, a number of authors, and in particular we, propose the following therapeutic methods.
Interventional treatments
Intra-articular injections
Injections into the sacroiliac joint with local anesthetics or corticosteroids can eliminate the pain or provide significant relief for up to 1 year. It is assumed that intra-articular injections are more effective than periarticular infiltration. However, periarticular infiltration has shown good results in short follow-up in two double-blind studies (Manchikanti L, Singh V, Pampati V, et al., 2001; van der wur P, Buijs Ej, Groen Gj, 2006), confirming the importance extra-articular sources of sacroiliac pathology (Luukkainen R, Nissila M, Asikainen E, et al., 1999; Luukkainen RK, wennerstrand PV, Kautiainen HH, Sanila MT, Asikainen EL, 2002; Borowsky CD, Fagen G, 2008). Controlled studies suggest that both intra- and extra-articular injections may be effective. Luukkainen et al. (2002) describe a randomized trial on 24 patients. The first group (n=13) underwent periarticular infiltration with corticosteroids and local anesthetic. The second group (n=11) received local anesthetic and saline. After a month, pain according to VAS decreased significantly in the first group after periarticular infiltration compared to the control group. Maugars et al. (1996) reported the treatment of 13 sacroiliac joints. Intra-articular corticosteroids were administered to 6 joints, and saline was administered to the remaining 7 joints. After a month, in the first group, pain in 5 out of 6 joints decreased by more than 70%, while there was no effect in the placebo group. All patients in the control group and 2 patients in the first group who experienced a short period of symptom relief were given repeated intra-articular injections of corticosteroids. At 1, 3, and 6 months, pain was significantly reduced in 86%, 62%, and 58% of patients, respectively.
At the same time, despite the effectiveness of using corticosteroid drugs in orthopedic practice, this technique has a number of contraindications and complications. In this regard, we use a minimally invasive intervention method - radiofrequency denervation.
Radiofrequency treatment (denervation) of the sacroiliac joint
The effectiveness of radiofrequency neurotomy in the treatment of sacroiliac joint pain has been reported in several prospective (Burnham RS, Yasui y, 2007; Gevargez A, et al., 2002) and retrospective studies (Ferrante FM, et al., 2001; Cohen SP, Abdi S, 2003; Yin w, et al., 2003), as well as in one randomized controlled trial (Cohen SP, et al., 2008). However, selection criteria, definition of success, and radiofrequency parameters (temperature, duration, and neurotomy site) vary widely among studies. Gevargez et al. (2002) performed 3 interventions (radiofrequency energy 90 °C) in the area of the posterior sacroiliac ligament and 1 in the area of the posterior branch of the L5 nerve root. In comparison, Ferrante et al. (2001) performed complex bipolar intra-articular interventions with a temperature of 90 °C. Cohen and Abdi (2003) report isolated 80 deg. interventions at the level of the posterior branches of the L4-L5 nerve roots and the lateral branches of the posterior branches of the S1-S3(S4) nerve roots. Yin et al. (2003) followed the same technique, except for the posterior ramus of the L4 nerve root, and he performed the neurotomy more caudally. Burnham and Yasui (2007) describe bipolar radiofrequency denervation lateral to the dorsal sacral foramen as well as monopolar radiofrequency neurotomy of the posterior ramus of the L5 nerve root. Recently, Cohen et al. (2009) examined which demographic and clinical factors may influence the outcome of radiofrequency treatment for the sacroiliac joint. The paper reports that intense pain radiating below the knee and age over 65 years are a statistically significant predictor of failure of radiofrequency treatment.
One study suggests the use of pulse radiofrequency therapy for the treatment of sacroiliac pain (Vallejo R, Benyamin RM, Kramer J, Stanton G, Joseph Nj, 2006). A neurotomy is performed on the medial branches of the L4-L5 nerve roots and the lateral branches of the posterior branches of the S1-S2 roots. Good and excellent results (>50% and 80% reduction in VAS, respectively) were achieved in 73% of patients. The duration of the clinical effect of treatment ranged from 6 to 32 weeks.
Due to the varied and extensive innervation of the sacroiliac joint, difficulties sometimes arise when using classical radiofrequency methods. In two double-blind randomized and one controlled studies, Dreyfuss et al. (2008; 2009) demonstrated the superiority of multicenter denervation of the deep block of the lateral sacral branches in the area of the sacroiliac joint ligaments over single-point denervation. However, these studies also showed that lateral rami neurotomy does not sufficiently interrupt nociceptive information originating from the intra-articular part of the sacroiliac joint innervation (eg, capsular distension). To solve the problem with various options for anatomical innervation, some researchers use low temperatures (42 degrees) during denervation, which increases the area of exposure, minimizing the effect of exposure. In 2008, a randomized controlled trial (Cohen SP, Hurley Rw, Buckenmaier CC 3rd, et al., 2008) and a series of retrospective studies (Kapural L, Nageeb F, Kapural M, et al., 2008) were published regarding low-temperature radiofrequency treatment of sacral -iliac joint. In a retrospective study, from 3 to 4 months after treatment, the mean VAS pain score decreased from 7.1 to 4.2 (Kapural L, Nageeb F, Kapural M, et al., 2008). 18 patients had good or excellent effect, while 8 had minimal or no effect. Cohen et al. (2008) conducted a randomized, placebo-controlled trial in which classic radiofrequency neurotomy was performed on the dorsal rami of the L4 and L5 nerve roots, and low-temperature radiofrequency intervention on the lateral rami of the S1 to S3 nerve roots. At 1, 3, and 6 months after treatment, 79%, 64%, and 57% of patients, respectively, reported greater than 50% pain relief. In the placebo group, only 14% of patients reported significant improvement at 1 month, and no effect was observed at 3 months. It is also worth considering the cost of consumables for radiofrequency therapy, as these are not covered by funding in some countries.
Conclusion
Under our supervision from 2009 to 2014. There were 385 patients with sacroiliac joint syndrome. In 24% of cases there was a history of pelvic trauma. More than half of the patients (52%) suffered from osteochondrosis of the lumbosacral spine for a long time. In the remaining patients (26%), the cause of pain in the sacroiliac joint was provoked by Hip-Spine or Knee-spine syndrome against the background of osteoarthritis of the hip or knee joint. At the same time, coxarthrosis caused dysfunction and pain in the SIJ faster than arthrosis of the knee joint.
We carried out complex conservative therapy including manual manipulation, matrix therapy (MaRy e), therapeutic blockades, homosyniatric therapy and shock wave therapy for pain caused by pathology of the sacroiliac joint. In 80% of cases, we were able to relieve pain for a long period (from 2 to 5 years) without resorting to radiofrequency denervation. But in some patients (20%), the pain syndrome was severe and recurrent. In this group, the majority were patients with concomitant degenerative-dystrophic pathology of the lumbar spine and large joints of the lower limb. Due to the ineffectiveness of conservative therapy for this group of patients, the tactics of radiofrequency denervation of the sacroiliac joint were chosen (Fig. No. 2), which made it possible to relieve pain in the sacroiliac joint in this category of patients in 100% of cases.
Bibliography
1. Chensky A.D. Sacroiliac joint syndrome in traumatological and orthopedic pathologies of the spine and pelvis. dis. the doctors. med. sc. 1999
2. Kavalersky G.M., Bobrov D.S., Slinyakov L.Yu., Chensky A.D. Biomechanics of lumbar spine fractures in elderly and senile patients. Fundamental and applied problems of engineering and technology. 2015. No 4 (312). pp. 122-126.
3. Manchikanti L, Singh V, Pampati V, et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4:308–316.
4. Van der Wur P, Buijs EJ, Groen GJ. Intensity mapping of pain referral areas in sacroiliac joint pain patients. j Manipulative Physiol er. 2006;29:190–195.
5. Luukkainen R, Nissila M, Asikainen E, et al. Periarticular corticosteroid treatment of the sacroiliac joint in patients with seronegative spondylarthropathy. Clin Exp Rheumatol. 1999;17:88–90.
6. Luukkainen RK, Wennerstrand PV, Kautiainen hh, Sanila MT, Asikainen EL. Ef cacy of periarticular corticosteroid treatment of the sacroiliac joint in non-spondylarthropathic patients with chronic low back pain in the region of the sacroiliac joint. Clin Exp Rheumatol. 2002;20:52–54.
7. Borowsky CD, Fagen G. Sources of sacroiliac region pain: insights gained from a study comparing standard intraarticular injection with a technique combining intraand periarticular injection. Arch Phys Med Rehabil. 2008;89:2048–2056.
8. Maugars Y, Mathis C, Berthelot JM, Charlier C, Prost A. Assessment of the effect of sacroiliac corticosteroid injections in spondylarthropathies: a double-blind study. Br j Rheumatol. 1996;35:767–770.
9. Burnham RS, Yasui Y. An alternate method of radiofrequency neurotomy of the sacroiliac joint: a pilot study of the effect on pain, function, and satisfaction. Reg Anesth Pain Med. 2007;32:12–19.
10. Gevargez A, Groenemeyer D, Schirp S, Braun M. CT-guided percutaneous radiofrequency denervation of the sacroiliac joint. Eur Radiol. 2002;12:1360–1365.
11. Ferrante FM, King LF, Rochë EA, et al. Radiofrequency sacroiliac joint denervation for sacroiliac syndrome. Reg Anesth Pain Med. 2001;26:137–142.
12. Cohen SP, Abdi S. Lateral branch blocks as a treatment for sacroiliac joint pain: a pilot study. Reg Anesth Pain Med. 2003;28:113–119.
13. Yin W, Willard F, Carreiro J, Dreyfuss P. Sensory stimulation guided sacroiliac joint radiofrequency neurotomy: technique based on neuroanatomy of the dorsal sacral plexus. Spine. 2003;28:2419–2425.
14. Cohen SP, Hurley RW, Buckenmaier CC 3rd, et al. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109:279–288.
15. Cohen SP, Strassels SA, Kurihara C, et al. Outcome predictors for sacroiliac joint (lateral branch) radiofrequency denervation. Reg Anesth Pain Med. 2009;34:206–214.
16. Vallejo R, Benyamin RM, Kramer J, Stanton G, Joseph nJ. Pulsed radiofrequency denervation for the treatment of sacroiliac joint syndrome. Pain Med. 2006;7:429–434.
17. Dreyfuss P, Snyder BD, Park K, et al. e ability of single site, single depth sacral lateral branch blocks to anesthetize the sacroiliac joint complex. Pain Med. 2008;9:844–850.
18. Dreyfuss P, Henning T, Malladi n, Goldstein B, Bogduk n. e ability of multi-site, multi-depth sacral lateral branch blocks to anesthetize the sacroiliac joint complex. Pain Med. 2009;10:679–688.
19. Kapural L, Nageeb F, Kapural M, et al. Cooled radiofrequency system for the treatment of chronic pain from sacroiliitis: the rst case-series. Pain Pract. 2008;8:348–354.
Information about the authors:
Chensky Anatoly Dmitrievich – State Budgetary Educational Institution of Higher Professional Education First Moscow State Medical University named after I.M. Sechenov, Department of Traumatology, Orthopedics and Disaster Surgery. professor of the department, doctor of medical sciences, e-mail
Slinyakov Leonid Yurievich – State Budgetary Educational Institution of Higher Professional Education First Moscow State Medical University named after I.M. Sechenov, Department of Traumatology, Orthopedics and Disaster Surgery. Doctor of Medical Sciences, Professor,
Cherepanov Vadim Gannadievich – State Budgetary Educational Institution of Higher Professional Education First Moscow State Medical University named after I.M. Sechenov, Department of Traumatology, Orthopedics and Disaster Surgery. Candidate of Medical Sciences, Associate Professor, e-mail
Ternovoy Konstantin Sergeevich – State Budgetary Educational Institution of Higher Professional Education First Moscow State Medical University named after I.M. Sechenov, Department of Traumatology, Orthopedics and Disaster Surgery. Candidate of Medical Sciences, Associate Professor, e-mail
DIAGNOSIS AND TREATMENT OF THE SYNDROME OF THE SACROILIAC JOINT
A. D. CHENSKY, L. YU. SLINYAKOV, VG CHEREPANOV, K. S. TERNOVOY
Sechenov First Moscow State Medical University, Moscow
Information about the authors:
Chensky A. – Professor, PhD in Medical Science
Slinyakov Leonid Yurievich – IMSechenov First Moscow State Medical University. eDepartment of Traumatology, Orthopedics and Disaster Surgery. Doctor of Medical Sciences, Professor
Cherepanov Vadim Gannadievich – IMSechenov First Moscow State Medical University. eDepartment of Traumatology, Orthopedics and Disaster Surgery. PhD, Assistant of the Department
Ternovoy Konstantin Sergeyevich – IMSechenov First Moscow State Medical University. eDepartment of Traumatology, Orthopedics and Disaster Surgery. PhD, Assistant of the Department
One of the causes of pain in the lumbosacral spine are pathological processes that occur in the sacroiliac joints. we observed 385 patients with the syndrome of the sacroiliac joint from 2009 to 2014. we have conducted a comprehensive conservative treatment of pain caused by the pathology of the sacroiliac joint. In 80% of cases we have been able to stop pain
for long term (2 to 5 years) without resorting to radiofrequency denervation. But the proportion of patients (20%) suffered heavy and recurrent nature. In view of the ine ectiveness of conservative therapy for this group of selected patsietov tactics radiofrequency denervation of the sacroiliac joint, which allowed to stop pain in the sacroiliac joint in these patients in 100% of cases.
Key words: sacroiliac joint, pain, radiofrequency denervation.
Preparing for MRI of the sacroiliac joints
It is very important to remember that magnetic resonance scanning, despite the lack of preparation required, has a number of requirements. Before the study, patients must leave all unnecessary items in the storage room - this especially applies to jewelry, piercings, any metal objects, phones and gadgets. The powerful magnetic fields generated during an MRI can damage electronics and heat metal, causing burns.
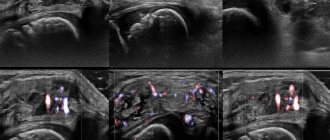
Magnetic resonance imaging of the sacroiliac joints with contrast
MR imaging of the SIJ supports the use of contrast enhancement. This technique involves the introduction of a special contrast agent into the patient’s blood, which accumulates in pathologically altered tissues due to inflammatory diseases and tumors. The use of contrast greatly facilitates the diagnosis of diseases of the sacroiliac joints and increases the information content of the study, especially in controversial cases.
MRI of the sacroiliac joint in STIR mode
Magnetic resonance imaging is not one study, but a whole complex of algorithms, modes and programs used to diagnose diseases. The STIR mode is one such algorithm, suppressing the signal from adipose tissue and detecting sacroiliitis in the early stages, when inflammation manifests itself only as bone marrow edema. Other diagnostic methods are not able to detect sacroiliitis at the very beginning, which ultimately worsens the prognosis and prevents effective prevention of complications.
How is magnetic resonance imaging of the sacroiliac joint performed?
MRI is carried out using a tomograph - a device in the form of a cylinder lying on its side, with a short and wide tunnel in the center. This tunnel is the working part of the installation; the patient is in it during the study. For this purpose, there are guides in the tunnel along which the table for the patient moves.
Before starting the study, you need to make sure that you have left all foreign objects, especially metal objects, in the storage room. Then, after going into the room with the tomograph, with the help of the medical staff, the patient is placed on the table. It is recommended to wear headphones on your ears - they muffle the rather loud sounds of the tomograph operating. To make the examination more comfortable, they also broadcast calm music and convey the operator’s instructions.
The duration of MR imaging of the SIJ is 15 minutes. If contrast enhancement is required, the procedure lasts 30 minutes. After completing the study, you need to wait no more than 30 minutes until the doctors decipher the images.
Possible complications and side effects
When done correctly, blockade is one of the safest procedures. One of the complications after it can be an allergic reaction to the drugs used. That is why CELT specialists necessarily prescribe tests to identify the patient’s allergy to the administered drugs. The phenomenon of infection is extremely rare. Its frequency does not exceed 1%. In addition, for some time there may be pain at the puncture site, which goes away after one to two days.
What will an MRI of the sacroiliac joints show?
Any patient wants to know what is visible on an MRI of the sacroiliac joints. Therefore, we provide a consultation with a radiologist to each of our patients - a specialist in the field of MRI diagnostics will show you your images, tell you what changes and signs were detected, what diseases they may correspond to. If you have had an MRI before, take the old images with you - this will allow you to compare them with the new ones and find out whether there are positive or negative dynamics in the development of the disease.
After the procedure
The patient stays in the clinic for one to two hours under the supervision of medical staff. If he does not have any non-standard reactions, he is sent home. He is prohibited from driving a car for 24 hours. The use of steroids may cause redness or paleness of the skin of the face, as well as an increase in blood pressure during the first few days after the procedure. In addition, steroids have an irritating effect on the stomach, so it is recommended to take a drug such as Omeprazole during the first three days after the blockade.
Interpretation of MRI of the sacroiliac joints
In a series of layer-by-layer photographs taken in several projections through the area of the sacrum and pelvis, it is easy to see the SIJs themselves, their articular surfaces and articular cartilages, the joint cavity, the surrounding ligaments and tendons, as well as the pelvic bones. An MRI diagnostic doctor, looking at the images, pays attention to deviations from the norm, signs of inflammatory changes, narrowing of the joint space, and the presence of effusion in the joint cavity. In STIR mode, signs of sacroiliitis in the form of bone marrow edema can be detected. When contrast is used, the dynamics of its accumulation and release from tissues are assessed. The presence of gross changes in the form of tumors, osteomyelitis, osteoporosis, etc. is excluded. The information received after decoding the images is included in the conclusion.