The joint between the foot and lower leg can withstand loads that are 7 times the human body weight. Osteoarthritis of the ankle joint (deforming osteoarthritis, arthritis, OGS) makes movement painful and difficult. The disease slowly but purposefully exposes not only cartilage to dystrophic, inflammatory changes, but also all other elements of the joint, including the capsule, membrane, and bone tissue. In addition, muscles and ligaments may be damaged. All this can lead to partial or complete disability.
According to studies, the likelihood of being sent to the emergency room due to ruptures, sprains of ligaments or tendons when diagnosed with AHS triples!
Ankle arthritis, although common in older people, can also occur in younger patients, even teenagers and young children. This happens both due to the innate characteristics of the body or wearing high-heeled shoes, and due to excessive force loads on the joints or lack of physical activity. How does arthrosis develop and what to do about it?
Deforming osteoarthritis of the ankle joint: how does it appear?
The ankle joint does not have its own vascular system, therefore, with metabolic disruptions caused by aging, intense training or other factors, the nutrition of the cartilage tissue is also disrupted. Due to the lack of “building materials” and important microelements, intracellular metabolism decreases, cartilage recovers poorly and slowly, and its basic structure gradually changes.
Chondroitin and glucosamine are synthesized less frequently and in small volumes, which are not enough to support and timely restore the joint. Hence the loss of elasticity, shock-absorbing properties and strength, and the formation of bone growths. In the future, if the disease starts and you don’t know how to treat osteochondrosis of the ankle joint, the cartilage will continue to deteriorate.
In the initial stages of the disease, symptoms of osteoarthritis of the ankle joint are rarely bothersome. Sometimes there is pain, but it goes away as quickly as it started.
Factors that can provoke OGS:
- Poor nutrition.
The body lacks protein, fatty acids and other essential substances.
- Uncomfortable shoes.
For example, high heels.
- Heredity.
- Age-related changes.
- Increased sports loads.
For example, boxing or dancing. There is also a high risk of arthrosis if you suddenly stop playing sports.
- Excess weight.
Excess weight significantly increases pressure on the joints.
- Flat feet, high stature, congenital dysplasia.
- Concomitant diseases such as diabetes, hemophilia, osteochondral disorders or vascular atherosclerosis.
It may occur due to problems with hormones or the thyroid gland. Especially at risk for women during menopause.
- Inactivity.
A lack of daily physical activity weakens muscles, which significantly increases the load on joints.
- What else potentially influences the development of ankle osteoarthritis?
- Hypothermia of the legs.
For example, your feet are cold because your shoes are not appropriate for the season.
- Carrying heavy things.
Arthrosis is especially often diagnosed among loaders.
- Injuries in the ankle area.
Any dislocations and fractures can cause cracks in the cartilage tissue. If microtrauma is not noticed and treated in time, serious consequences and diagnoses cannot be avoided.
In addition, the prerequisites include different leg lengths (due to shifting loads), damage to internal organs, and deformation of the toes. Work that requires a person to stand for a long time throughout the working day also often becomes an aggravating factor along with obesity.
Diagnostic methods
To determine the functional usefulness of the joint, a number of tests are performed. Their results make it possible to assess muscle strength, sensitivity, and the preservation of tendon reflexes. The primary diagnosis can also be made on the basis of patient complaints, medical history, and external examination. Since the symptoms of DOA of the ankle are similar to the signs of arthritis, bursitis, tenosynovitis, instrumental studies are required:
- radiography;
- magnetic resonance or computed tomography;
- ultrasonography.
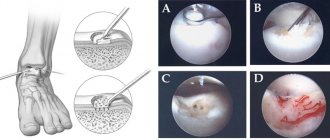
According to indications, punctate is collected for morphological study. If necessary, an arthroscopic examination of the inner surface of the ankle is prescribed, taking samples of synovial fluid and membrane, cartilage tissue.
Symptoms of ankle osteoarthritis
The main problem in identifying symptoms and treating osteoarthritis of the ankle joint is that the disease almost does not manifest itself in the initial stages. According to statistics, people tend to ignore pain after or during physical activity, which subsides and disappears at rest.
With osteoarthritis of the ankle joint, patients are concerned about:
- It's a dull pain.
In particular, the morning one, which disappears after 2-3 hours.
- Stiffness of movements.
It’s unpleasant, painful, difficult to rotate your foot or make circular movements.
- Swelling in the shin area and lower ankle.
- Dull crunching or clicking sounds.
People who have been diagnosed with deforming osteoarthritis of the ankle joint find it difficult to climb stairs and even walk. Lack of therapy after several months or years (depending on the individual clinical picture) leads to loss of ability to work.
Grade 2 osteoarthritis of the ankle joint, which can still be treated with medication:
- Grade 1 osteoarthritis of the ankle joint.
It is difficult to recognize arthrosis on X-rays. Sometimes it is almost asymptomatic - patients note only local rare pain under heavy loads and fatigue. After rest, the cramps disappear instantly. And although there are no external changes at all, inside the cartilage is destroyed, and there is no longer enough synovial fluid for lubrication. The supply of nutrients to areas of inflammation is hampered, which provokes subsequent destruction and friction of bones against each other.
- Grade 2 osteoarthritis of the ankle joint.
The pain becomes brighter and is present for a long time even in a state of rest or rest. The temperature in the ankle area increases (it feels hot to the touch), upon palpation, complaints of pain appear, and slight swelling may be noticed. X-rays clearly show the presence of osteoarthritis. This stage is characterized by lameness, stabbing pain and loud crunching, increased pain upon awakening.
If stage 1 osteoarthritis of the ankle joint can be treated relatively quickly and the accompanying symptoms can be relieved without surgery, then at the third stage, surgery is unlikely to be avoided. Grade 3 is characterized by pronounced visual curvature, joint deformation, bone displacement, very strong pain when trying to take a vertical position, the pain radiates higher, spreads to the calf, knee and entire leg, and does not go away even at night. In phase 4, complete destruction of the joint and extensive bone growths are observed.
Attention! Without the necessary treatment, deforming osteoarthritis of the ankle joint will progress, leading to impaired posture and gait. This happens especially quickly in old age, when the muscles and the body as a whole are very weakened, and it is quite difficult to normalize metabolic processes.
Possible complications
At the final stage of deforming osteoarthritis of the ankle, complete or partial immobilization of the joint is observed. If it occurs in a functionally disadvantageous position, then the person is able to move only with the help of crutches, since resting on the foot is impossible.
The course of DOA is often complicated by secondary reactive synovitis and spontaneous hemorrhages into the joint cavity.
Treatment of ankle osteoarthritis
Treatment tactics for ankle osteoarthritis will vary depending on the patient's characteristics and the stage of the disease. For example, overweight people are shown a diet that involves losing excess weight. If you are not obese, you just need to adhere to the rules of proper nutrition, add more sources of protein, sulfur and selenium, and vitamins to your diet.
The main tasks are to relieve pain, restore the functional ability of the foot, regulate metabolic processes, and remove inflammation.
In general, therapy is based on:
- Taking medications.
Drug treatment of deforming osteoarthritis of the ankle joint involves a course of non-steroidal anti-inflammatory drugs (NSAIDs), vitamins, painkillers to relieve pain, and chondroprotectors.
- Therapeutic physical education.
Minimum heavy loads. A set of safe exercises is prescribed that strengthen the muscle frame, but do not overload the ankle and other joints. Exercise therapy needs to be done daily. Class time is 15-30 minutes. They are allowed to do gymnastics in the water.
- Selection of special orthopedic shoes
good for fixing the ankle.
- Therapeutic massage
, which relaxes spasmodic muscles, improves metabolic processes in the soft tissues around the joint.
- Physiotherapy.
It is recommended to influence the joint with ultrasound, magnetic fields, therapeutic mud, electric current, as well as ultraviolet and infrared radiation. All this activates the vital forces of the body, helps eliminate swelling, reduce pain and improve the penetration of medications into the affected area.
An integrated approach speeds up the healing process and improves well-being. By themselves, such auxiliary methods as exercise therapy, massage, physiotherapeutic procedures, analgesics are aimed at alleviating the condition, superficially eliminating symptoms, but not at regenerating the cartilage itself. In the most advanced cases, when therapy does not produce results, surgery is required. For example, surgical removal of osteophytes (growths) or damaged cartilage, its replacement with artificial materials (metal or ceramic implants).
Prevention
Prevention of DOA consists of eliminating all factors that provoke damage to the cartilaginous structures of the ankle. Orthopedists recommend giving up smoking and alcohol, which worsen the condition of the blood vessels in the legs. It is necessary to replenish the diet with fresh vegetables, fruits, low-fat fermented milk products - the main sources of water- and fat-soluble vitamins and microelements. During sports training, elastic bandages should be used to protect all joint structures from microtrauma.
Classification of the disease
Osteoarthritis of the ankle can be primary or secondary.
Primary arthrosis can occur in the following forms:
| Form | Description |
| Localized | The degenerative process affects nearby joints: knee, hip |
| Generalized | The process extends to remote connections |
The secondary form occurs as a concomitant disease with other pathologies (trauma, bursitis, rheumatoid arthritis).
Classification of stages according to radiological signs:
- absence of manifestations;
- dubious signs;
- changes are minimal (single osteophytes, narrowing of the lumen of the joint space);
- pathological narrowing of the gap, multiple osteophytes;
- pronounced changes (the lumen is not visible, osteophytes are rough).
Stages of pathology
In total, three stages of the disease can be distinguished:
| First | Second | Third |
| This stage is best treated. True, the cartilage tissue is already severely damaged. The joint cannot be deformed, the appearance is the same as in its normal state. In fact, the process of destruction has already begun. Cartilage cells, which do not receive the required amount of auxiliary components, die over time. Later the process moves on to fabrics. Feels pain. | Symptoms become more noticeable and acute. All the time a person suffers from pain. Deformation is observed, the joint becomes larger, and this is visible to the naked eye. Already at this stage, one of the irreversible changes occurs - bone tissue grows outside the joint. | The main manifestation is characterized by significant deformation. The shape of the ankle has changed, it becomes many times larger and swells. The cartilage is very damaged, as are the ligaments. If measures are not taken in time, the person faces disability. It may be limited to the inability to perform certain actions or result in complete incapacity. |
Narrowing of the joint space
Attention! You need to see a doctor after the appearance of minor pain, which has some frequency. If done on time, there is a high probability of a favorable outcome after treatment. The later the patient identifies his pathology and begins therapy, the greater the chance that he will need surgery on the ankle joint of the right or left leg for arthrosis.
Degree of damage
Factors causing the disease
Main reasons:
- severe physical activity (intense sports, long walking);
- uncomfortable shoes;
- excess weight;
- frequent viral infections;
- hypothermia;
- injuries of the joint, periarticular ligaments;
- surgical operations;
- metabolic disorders (gout, diabetes);
- congenital developmental anomalies;
- the presence of a primary focus of inflammation (from arthritis to osteoarthritis);
- genetic predisposition (collagen gene defect);
- deficiency of the hormone estrogen in menopausal women.