A little anatomy
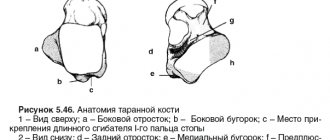
The supracalcaneal bone is formed by one of the parts of the spongy tarsus. It is formed by the head, body and connecting neck. The head meets the scaphoid bone, the body, covered 60% with articular cartilage, articulates with the lateral and posterior malleolus like a fork. The dorsal process has lateral and medial tubercles connected by a tendon. The joints are supplied with blood from the peroneal, posterior, tibial artery and its branches. Due to the unique anatomical architecture, pathological ischemia occurs after injury, peripheral arterial occlusion. The condition is accompanied by subjective symptoms of necrosis of the talus of the ankle joint.
Removal, curettage and bone marrow stimulation.
After debridement, several channels are produced that communicate the defect with the bone marrow. This procedure can be performed using reaming or microfracturing. The purpose of the manipulation is to destroy the barrier of sclerotic subchondral bone that prevents the migration of stem cells from the bone marrow. As a result, a clot is formed, saturated with growth factors and stem cells, which is subsequently rebuilt into hyaline-like cartilage tissue. Most often used for stages 3-4 of the disease. The size of the defect should not exceed 1.5 cm. In clinical studies, the effectiveness of the method was estimated from 46 to 100% (on average 85%).
Causes and symptoms
The pathology is provoked by: lupus erythematosus, arthritis, Gaucher disease, anemia, diabetes mellitus. Also leading to aseptic necrosis:
- embolism;
- thrombosis;
- use of vasoactive drugs;
- problems with lipid metabolism;
- intraosseous pressure;
- load on the tibia, sharp flexion of the soles, affecting the great vessels.;
Symptoms of necrosis due to the similarity of pain symptoms, the disease is often mistaken for arthrosis. The difference lies in the rapid progression of subjective signs and the age of the patients. Damage to the ankle joints occurs more often in active people 20-45 years old. The main symptoms of post-traumatic aseptic necrosis of the left talus:
- increasing pain in the ankle;
- limitation of motor function;
- the appearance of swelling and lameness.
With progressive symptoms, medical attention is necessary, otherwise the disease will lead to disability.
Surgical treatment of osteochondral injuries of the talus.
Surgical treatment of OPTC depends on many factors: patient characteristics such as age, activity level, comorbidities, characteristics of the lesion itself such as its location, size, depth of the lesion, lesion morphology, duration. Basically, surgical treatment is based on one of three principles: 1) removal of the loose body with or without bone marrow stimulation through microfracture, reaming 2) preservation of cartilage through retrograde reaming, fixation of the fragment or replacement of the defect with cancellous bone 3) stimulation of the formation of new hyaline cartilage by due to osteochondral block transplantation, mosaic chondroplasty, allograft.
Classification by stages
Signs of avascular necrosis of the ankle joint help determine the extent of the damage. More accurate information is provided by an x-ray, from which a specialist accurately determines the phase of the disease.
- I – initial subarachnoid compression affects 10% of the bone tissue. The disease does not limit movement; it periodically makes itself felt after exercise.
- II - partial fragmentation of a separate area, the appearance of severe pain, cracks.
- III - bone damage by 40-50%.
- IV - total destruction and necrosis of cells with cartilage separation, destructive changes in the tibia. Fragmentation leads to loss of functionality of the legs. A patient with necrosis of the talus cannot do without surgery.
Technology for the treatment of aseptic necrosis of the talus in Stoparthrosis If you have similar problems, contact the clinic. We employ traumatologists, orthopedists, and physiotherapists with 15-20 years of experience, specializing in the treatment of joint diseases. On the day of treatment, doctors relieve symptoms and provide first aid.
Causes of bone cysts.
The causes of bone cysts have not yet been studied in detail. The disease can appear as a result of previous injuries (dislocations, falls, bruises, etc.). It also affects people suffering from rheumatoid arthritis, osteoarthritis and chronic gout. Bone cysts increase the risk of developing fractures because... when they form, the volume of bone tissue decreases, and the bones can no longer withstand the previous load and break easily.
The disease can be asymptomatic for a long time and be discovered accidentally during a fracture or during an X-ray examination for another reason. Sometimes a bone cyst can cause swelling and pain.
Diagnostics
Doctors will find out the etymology of the disease, conduct an external examination, and prescribe an informative examination. These measures are necessary to draw up a clinical picture and an individual therapeutic program. Instrumental diagnostics consists of radiography, MRI, CT, and blood biochemistry. Experts detect abnormal changes in the joints within the first week. To confirm the diagnosis, microscopic tests are performed after 5 days, once again confirming local necrosis of mast cells.
| An injection into the ankle joint for necrosis of the talus |
Sign up for treatment
Classification of osteochondral injuries of the talus.
Radiological classification of osteochondral lesions of the talus by Berndt and Harty
CT classification of osteochondral lesions of the talus Ferkel and Sgaglione
MRI classification of osteochondral lesions of the talus Hepple.
What therapeutic methods are used?
Reducing the load on the hip joint with physical therapy, careful attitude when abstaining from sports, immobilization of the hip joint (for example, orthopedic prosthesis) Hyperbaric oxygen therapy (hyperbaric oxygen therapy) in the earliest stage of necrosis of the femoral head.
Surgeries on the hip with drilling holes in the hip bones (for example, pri-foramen), Surgeries on the hip with transplantation of bone cartilage Surgeries on the hip such as osteotomy (for example, varisation osteotomy according to M. Perthes) Artificial hip joint using endoprosthetics for a fractured femoral head .
Symptoms and course
Unfortunately, the disease can occur without any symptoms for a long time. The patient does not experience pain, so he consults a doctor only when the infection has penetrated deep into the bone.
Signs of jaw necrosis:
- pain in an infected tooth or in the socket of an extracted one;
- loosening of teeth;
- swelling so severe that it disrupts the symmetry of the face;
- purulent discharge from the gums;
- putrid odor from the mouth;
- pain when swallowing, chewing, talking.
The main symptom of osteonecrosis of the jaw is bone exposure
.
Retrograde reaming.
This method will require the use of x-ray control and knowledge of the exact topography of the defect location. Retrograde reaming is the method of choice in the presence of a large subchondral cyst and with intact articular cartilage, as well as in cases of deep defect location, when it is difficult to reach it using the arthroscopic method. For medial defects, the entry point of the wire becomes the tarsal sinus. In clinical studies, the effectiveness of the method was estimated from 81 to 100% (average 88%).
How does necrosis end?
A favorable outcome of the pathology will be with enzymatic melting of tissues, germination of connective tissues into the remaining dead tissue, followed by the formation of a scar. The area of necrosis can become overgrown with connective tissue, resulting in the formation of a capsule. In addition, bone can form in the dead area. This phenomenon is called ossification.
An unfavorable outcome of the pathological condition is characterized by purulent melting, as a result of which the risk of bleeding and spread of the lesion increases. This is how sepsis will develop.
With ischemic stroke, myocardial infarction, necrosis of the kidney or pancreas, that is, when vital organs are affected, there is a high probability of death.
Rehabilitation after surgery for osteochondral injuries of the talus.
Most authors adhere to the standard rehabilitation protocol, which recommends 6 weeks of immobilization after surgery using bone marrow stimulation. However, recently, work has appeared indicating that a 2-week period of immobilization is more than enough for small and medium-sized defects. Rehabilitation consists of training active and passive range of motion, muscle strength and muscle balance of the lower leg, reducing swelling and proprioceptive training.
Pain, a sensation of wedging, and swelling often persist for up to 1 year after surgery. After 6 months, it is advisable to perform an MRI control to assess the dynamics; in the presence of severe bone marrow edema, the prognosis is unfavorable. In such cases, progression of the lesion may further lead to the need for arthrodesis or ankle replacement.
What treatment can help with necrosis of the femoral head?
To make a treatment decision, classification in ARCO is mandatory. In this case, the age of the patient, the degree and localization of necrosis are very important. In adults, unlike children diagnosed with necrosis of the femoral head (M. Perthes), self-healing is impossible. The condition of the hip joint, the general condition of the patient, additional diseases, and life expectancy are also taken into account in the decision-making process about treatment.
The earlier the stage of the disease with necrosis of the femoral head, the higher the chances of mitigating symptoms and even a complete recovery.
What is the diagnosis using x-rays?
Digital X-rays are a modern low-emission examination method, but they are not very suitable for diagnosis in the early stages of the disease, because X-rays show only changes in bone structure.
Bone beams begin to break down only weeks after necrosis (death of bone cells due to lack of blood circulation) has occurred. Therefore, necrosis of the femoral head cannot be detected using x-rays in the early stages of the disease.
6.6. lupus erythematosus
Hebra (1854) described lupus erythematosus, which was mainly located on the face, cheeks and nose in a butterfly pattern. Cazenave (1851) proposed to call this disease lupus erythematosus, perhaps it was discoid lupus erythematosus. Kaposi (1872) used this name to distinguish only manifestations of skin damage, but not damage to internal organs. Osler (1895-1904), calling this disease exudative erythema, described various manifestations of systemic lupus erythematosus in the internal organs. Libman and Sack (1924) called this disease non-rheumatic warty endocarditis. Baehr (1935) presented autopsy materials on 23 patients, putting forward the idea of the dangers of solar radiation in this disease, and also described glomerulonephritis, which had the appearance of “golden turns of threads.”
Haggare (1948) was the first to prove the cellular nature of lupus using bone marrow extraction. Miescher and Fauconnet (1956), observing growth factors of lupus erythematosus cells that were absorbed by blood serum when they came into contact with isolated cell nuclei, suggested that lupus cell factors were antinuclear antibodies. Friou (1958) reported the use of fluorescent anti-human globulins for the detection of antinuclear antibodies. Klemperer (1942), having studied systemic lupus erythematosus and dermatosclerosis, proposed calling them diffuse colloid disease. Despite the fact that there is still debate in scientific circles about the nature of these diseases, the concept of “colloid disease” was accepted by everyone very quickly. In 1952, Ehrlich proposed the term “connective tissue diseases,” which gradually replaced the previous name.
Systemic lupus erythematosus is a multiple autogenous autoimmune disease affecting many systems and organs. The mechanism of this disease mainly consists of the deposition of immune complexes in all internal organs, but the exact causes of the disease have not yet been fully explained.
Systemic lupus erythematosus causes ANFH due to the deposition of immune complexes. It activates complements and generates active mediators that penetrate bone tissue (trabeculae, mesh structures of bone marrow, microcapillaries inside the bone) and destroys them, changing the viscosity and rheology of the blood, forming blood clots. As a result of this, osteolytic necrosis occurs in the head of the femur, also affecting the acetabulum and branches of the ischium.
The main pathological changes in lupus erythematosus are the occurrence of mucus-like edema and fibrinoid degeneration of connective tissue, as well as necrotizing vasculitis. It should be especially noted that when patients with lupus erythematosus take steroid hormones, the incidence of ANFH increases sharply after such treatment.
Systemic lupus erythematosus in combination with necrosis of the femoral head occurs, firstly, due to the fact that it directly causes this necrosis; secondly, because after taking steroid hormones, degeneration occurs in the structure of the femoral head, the mesh structure of the trabeculae, bone marrow and microcapillaries inside the bone are damaged, fat cells inside the bone hypertrophy, intraosseous microcapillaries are compressed in the area of greatest load of the femoral head, and the flow stops supply into the bone, and eventually the femoral head collapses.
Generalization
Necrosis of the femoral head is a serious disease of the bones of the hip joint. In this case, local destruction of the bone of the femoral head occurs, as bone tissue dies in certain areas. Necrosis of the femoral head in adults is a typical disease of civilization. As with a heart attack, the main risk factors are smoking, high blood fat levels and alcohol abuse. Every year, many thousands of people suffer from necrosis of the femoral head in Germany alone!
By age, these patients are usually from 35 to 45 years old.
Men are more often affected than women. The disease necrosis of the femoral head significantly reduces the quality of life of people. In 30-70% of cases, bilateral necrosis of the femoral head is observed. Arrival arrangements
Fixation.
Fixation of the fragment is performed only in cases of fresh extensive damage. The torn osteochondral fragment is lifted, the underlying bed is subjected to microfracture or reaming, and then the fragment is fixed using submersible absorbable screws or fibrin glue. The method is technically complex and its indications are quite narrow, but when it was used according to indications, a good result was observed in 89% of cases.
Thus, the most effective and technically simple method of treating the vast majority of osteochondral injuries of the talus at the moment is removal, curettage and bone marrow stimulation. Depending on the equipment of the operating room and the skills of the operating surgeon, this intervention can be performed either openly or arthroscopically.
How is necrosis of the femoral head recognized?
During the appointment, we review the patient’s complaints about the hip and analyze possible risk factors for necrosis of the femoral head.
An accurate history of hip pain and a thorough clinical examination are then performed.
The examination criteria are:
- hip mobility
- sensation of hip mobility
- pain areas in the hip
- positions that can cause pain
- Muscle mass and strength of the gluteal hip muscles
- gait
Thanks to our many years of experience, we can correctly assess the symptoms and begin treatment.
In orthopedics, a number of different hardware diagnostic methods are used. X-rays and magnetic resonance imaging (MRT) confirm the diagnosis of the hip.
Types and stages of disease development
The stages of development of aseptic necrosis of the head of the hip joint do not have a clear distinction between each other. The first stage lasts about six months, when pain occurs during exercise or during bad weather, after the disappearance of the provoking factor it goes away. The second stage also lasts about six months. During this period, thinning of the muscles of the buttock and thigh appears.
The third stage takes a longer time - up to 2.5 years, during which the tissue surrounding the necrosis zone resolves. Patients are already beginning to move exclusively with a cane. In the fourth stage, which develops over about 6 months, patients cannot move on their own. However, the duration of development of the disease is individual for each person, depending on concomitant diseases, timely treatment and other factors.
Doctors distinguish four types of necrosis of the hip joint:
- Segmental (observed in 48% of patients with this diagnosis). A small area of necrosis appears as a cone on the upper part of the femoral head.
- Complete necrosis (diagnosed in 42% of patients). The entire head is affected.
- Peripheral (occurs in 8% of patients). The pathology affects the outer part of the head, located under the articular cartilage.
Central (observed in 2% of cases). A zone of necrosis forms in the center of the head of the femur.
POLYTRAUMA / POLYTRAUMA
Bondarenko A.V., Batrak Y.Yu., Plotnikov I.A.
Federal State Budgetary Educational Institution of Higher Education "Altai State Medical University" of the Ministry of Health of the Russian Federation, Regional State Budgetary Institution of Health Care "Regional Clinical Hospital of Emergency Medical Care", Barnaul, Russia
TREATMENT OF DAMAGES TO THE ASTRAL BONE DURING POLYTRAUMA
Fractures and dislocations of the talus are a rare and complex pathology. Being a consequence of high-energy impacts, they often occur in polytrauma (PT) [1-3]. Due to its unique anatomy, blood supply, and numerous complex articulations, treatment of injuries to the talus presents significant challenges. Their course is often accompanied by the development of infectious complications, degenerative arthrosis, hindfoot deformities, avascular necrosis, unsatisfactory outcomes and a high level of disability [4-6]. Since almost all talar fractures are intra-articular, they require precision reduction, stable fixation and early function [4, 7]. The presence of several severe injuries in patients complicates the use of conventional surgical methods for treating injuries of the talus or postpones their implementation to a later date, which leads to the development of complications - edema, epidermal blisters, fibrous changes in soft tissues, and avascular necrosis [8-10]. In the late period, it is often not possible to satisfactorily compare fragments and hold them using traditional methods. Taking this into account, it is necessary to search for simple, minimally invasive methods of surgical treatment of injuries to the talus in patients with PT, both in the early and late periods. Purpose of the study
– to find out the frequency and nature of injuries to the talus during polytrauma, treatment features, including the use of modern minimally invasive methods of osteosynthesis.
MATERIAL AND METHODS
The study was carried out in accordance with the ethical principles of the Declaration of Helsinki (World Medical Assosiation Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects, 2013) and the “Rules of Clinical Practice in the Russian Federation” (Order of the Ministry of Health of the Russian Federation dated June 19, 2003 No. 266) with patient consent to participate and approved by the local ethics committee. Patients were included in the study in a continuous manner from a limited area over a limited period of time. From 2000 to 2021, 175 patients with 182 injuries of the talus, aged from 14 to 80 years (median - 32 years, interquartile range - from 27 to 42 years) were treated at the Regional Clinical Hospital of Emergency Medical Care in Barnaul. . Men - 145 (82.9%), women - 30 (17.1%), workers - 91 (52%), non-working people of working age - 69 (39.4%), students and pupils - 9 (5.1%) ), pensioners – 6 (3.4%). 145 (82.8%) patients were injured as a result of high-energy impacts: in road traffic accidents - 97 (55.4%), in falls from great heights - 48 (27.4%), as a result of low-energy impacts : in case of accidents at home - 21 (12%), in case of sports injuries - 9 (5.1%). In 117 (66.9%) patients, injuries to the talus were one of the components of PT. Its severity according to the ISS scale [11] in 75 (64.1%) patients ranged from 17 to 25 points, in 26 (22.2%) – from 25 to 40 points, in 16 (13.7%) – over 41 points. Traumatic brain injuries were detected in 24, of which 15 had cerebral concussions, 9 of them had brain contusions, 2 of them had intracranial hemorrhages, 1 of them had fractures of the base of the skull. Injuries to the internal organs of the chest and abdomen - 21 of them, of which pneumothorax - in 2, hemothorax - in 2, kidney bruises - in 9, liver ruptures - in 3, spleen - in 3, intestines - in 1, omentum - in 1. Injuries to the musculoskeletal system of other localizations - in 83 (shoulder fractures – in 8, forearms – in 5, hips – in 18, shins – in 49, calcaneus – in 21, spine – in 21, ribs – in 14, pelvis – in 13). In 58 (33.1%) patients, the injury to the talus was isolated. Closed injuries to the talus were observed in 160 (87.9%) cases, open - in 22 (12.1%). The work used Coltart's classification (1952) [9], which allows the damage to be most accurately detailed. The following were identified: 1. Fractures of the body of the talus without and with displacement (Fig. 1a). 2. Fractures of the neck of the talus of three types: type I – fractures of the neck of the talus without displacement of bone fragments (Fig. 1b); Type II – fractures of the neck of the talus with displacement of bone fragments and subluxation in the subtalar joint (Fig. 1c); Type III – fractures of the neck of the talus with dislocation of the body (Fig. 1d). 3. Subluxations and dislocations in the subtalar joint (Fig. 1e). 4. Complete dislocations of the talus (Fig. 1f).
Figure 1.
Types of injuries to the talus: a) fractures of the body of the talus are located posterior to the lateral process and involve both the ankle and subtalar joints; b) Type I – fractures of the neck of the talus without displacement; c) Type II – fractures of the neck of the talus with displacement and subluxation in the subtalar joint; d) Type III – fractures of the neck of the talus with dislocation of its body; e) subluxations and dislocations in the subtalar joint; f) complete dislocation of the talus
Fractures of the body of the talus were noted in 78 (42.9%) cases, without displacement - in 61 (33.5%), with displacement - in 17 (9.3%). Fractures of the neck of the talus of all three types – 54 (29.7%), I – 15 (8.2%), II – 26 (14.3%), III – 13 (7.1%). Dislocations and subluxations in the subtalar joint – 41 (22.5%). Complete dislocations of the talus – 9 (4.9%). Upon admission, patients with hindfoot injuries underwent radiographs of the ankle and foot in 2 standard views. To detail the damage, multislice computed tomography (MSCT) was performed. Indications for surgical treatment of injuries of the talus were: fractures of the body within the articular cartilage with a displacement of more than 2 mm, fractures of the neck of the talus with displacement, dislocations of the talus that could not be conservatively reduced and subtalar dislocations of the foot, open injuries. In case of isolated injuries, elimination of dislocations, reposition and fixation, including surgical fixation, were performed immediately until swelling and epidermal blisters appeared. Patients with PT were guided by the “Damage control” concept [12]. According to the recommendations of V.A. Sokolov, in the process of inpatient treatment of patients with PT, resuscitation and specialized clinical stages were distinguished [2]. In case of closed injuries and the absence of the possibility of surgical intervention, gross displacements were eliminated in full with immobilization with plaster, an external fixation device (AF) (Fig. 2) or temporary percutaneous fixation of the subtalar and ankle joints with K-wires (Fig. 3). Final osteosynthesis was carried out after stabilization of the condition and when the quality of the skin was satisfactory. In case of open injuries and extremely serious condition of patients after primary surgical treatment (PST), as a rule, temporary percutaneous fixation of the subtalar and ankle joints with K-wires was used, which provided the opportunity to perform further diagnostic and therapeutic procedures, and also reduced the severity of edema. Once the condition was stabilized, final osteosynthesis was also performed.
Figure 2.
Extrafocal osteosynthesis of an open fracture-dislocation of the talus with displacement of fragments
Figure 3.
Transarticular fixation with Kirschner wires of subtalar dislocation and dislocation in the Chopar joint
1. Fractures of the body of the talus.
There were 71 closed and 7 open fractures. Upon admission, all patients with closed fractures underwent plaster immobilization; in 57 patients it was the final method of treatment; 14 subsequently underwent osteosynthesis, of which 8 had open reduction and internal osteosynthesis with 3.5-mm cortical screws (Fig. 4). in 6 – closed reduction and transcutaneous minimally invasive osteosynthesis (MIO) with screws with a 4.0 mm channel (Fig. 5).
Figure 4. X-ray after open reduction of the talus body fracture and osteosynthesis with cortical screws with a diameter of 3.5 mm
Figure 5. Closed minimally invasive osteosynthesis of a fracture of the body of the talus using cannulated screws with a diameter of 4.0 mm with dorsal installation
All patients with open fractures underwent PSO with ANF osteosynthesis upon admission. In 3 patients this was the final method of treatment; in 4 patients, after the wound healed, open reduction was performed with osteosynthesis of the body of the talus with 3.5 mm cortical screws. 2. Fractures of the neck of the talus.
There were 47 closed and 7 open fractures.
All 15 type I talar neck fractures were closed. Upon admission, patients underwent plaster immobilization; in 9 patients it was the final method of treatment; in 6 patients, MIO of the talus was subsequently performed with 4.0-mm screws with a channel. There were 25 closed fractures of the neck of the talus type II, and 1 open. Upon admission, 15 patients with closed fractures underwent closed reduction with plaster immobilization, 6 underwent closed reduction with transarticular fixation with K-wires, and 4 underwent ANF osteosynthesis. Subsequently, at the profile-clinical stage, 15 patients with plaster immobilization underwent closed reduction and MIO with 4.0-mm screws with a channel. In 5 patients, after transarticular fixation, in 3 patients, after transosseous osteosynthesis, the ANF underwent open reduction with fixation with 3.5-mm cortical screws. In 2 patients, transarticular fixation and osteosynthesis of the ANF were the final treatment methods. On admission, a patient with an open fracture of the neck of the talus type II underwent PSO with ANF osteosynthesis. Based on wound healing, external fixation was changed to MIO with 4.0 mm channel screws. There were 9 closed type III fractures of the neck of the talus, 4 open ones. At the resuscitation stage, 3 patients with closed fractures underwent closed reduction of dislocations of the body of the talus with plaster immobilization, 4 patients underwent closed reduction with transarticular fixation with K-wires, and 2 patients underwent closed reduction. reduction with ANF osteosynthesis. At the profile clinical stage, 3 patients with plaster immobilization, 3 with transarticular fixation with K-wires, and 1 with ANF underwent open reduction and osteosynthesis with 3.5-mm cortical screws. In 2 patients, transarticular fixation with K-wires and ANF were the definitive treatment methods. Upon admission, all 4 patients with open fractures of the neck of the talus type III underwent PSO with reduction of the dislocated body of the talus and osteosynthesis of the ANF. Based on wound healing, external fixation of the ANF was changed to internal fixation with 3.5-mm cortical screws. 3. Subluxations or dislocations in the subtalar joint.
There were 36 closed injuries of this type, 5 open ones. For closed injuries, 5 patients underwent closed reduction of the dislocation with plaster immobilization, 27 patients underwent closed reduction with transarticular fixation with K-wires, and 4 patients underwent closed reduction with ANF osteosynthesis. Subsequently, at the profile-clinical stage, 4 patients with transarticular fixation and 2 patients with ANF underwent closed arthrodesis of the subtalar joint with 7.3-mm cannulated screws (Fig. 6). In 5 patients, plaster immobilization, in 23 – transarticular fixation with K-wires, in 2 – ANF were the final methods of treatment.
Figure 6. Radiographs of the foot after arthrodesis of the subtalar joint with osteosynthesis with cannulated screws with a diameter of 7.3 mm
For open injuries, transarticular fixation with K-wires was performed after PSO and reduction in 2 patients, and ANF osteosynthesis was performed in 3 patients. Subsequently, at the profile-clinical stage, in a patient with transarticular fixation, arthrodesis of the hindfoot joints was performed using a lockable Expert HAN nail (Switzerland) (Fig. 7), and in a patient with ANF, arthrodesis of the subtalar joint was performed with 7.3-mm screws with a channel. For 2 patients, ANF osteosynthesis was the final treatment method.
Figure 7. Radiographs of the foot after arthrodesis of the subtalar and ankle joints with a locking pin
4. Complete dislocation of the talus.
Closed complete dislocations of the talus were observed in 5 patients, open ones - in 4. In all patients with closed dislocations of the talus, upon admission, it was possible to close the prolapsed bone into place; after which, in 4 of them, transarticular fixation was performed with K-wires through the ankle and subtalar joints; in 1, ANF was used for fixation. These treatment methods were definitive. In case of open complete dislocations of the talus, 2 patients underwent PSO of open dislocation with reduction of the talus and transarticular fixation with K-wires; in 2 patients, PSO of open dislocation with reduction and osteosynthesis of the ANF was performed. At the profile-clinical stage, one patient with transarticular fixation underwent arthrodesis of the subtalar joints of the hindfoot using a lockable Expert HAN nail. For the rest, the osteosynthesis methods used upon admission became final. Thus, the final method of treatment was plaster immobilization in 71 cases, transarticular fixation with K-wires – in 30, osteosynthesis with 3.5 mm cortical screws after open reposition – in 31, MIO 4.0 mm screws with a channel – in 28, osteosynthesis of the ANF - in 12, arthrodesis of the subtalar joint with screws with a channel - in 8, arthrodesis of the hindfoot joints with locked Expert HAN nails - in 2. When studying the results, hospital mortality, the nature and number of complications, and the outcomes of the treatment were assessed. Long-term anatomical and functional results were monitored in 50 (38.6% of the primary cohort) patients with 51 injuries of the talus over a period of one to three years. To assess the results, the AO FAS [13] and Matthies-Luboschitz-Schwarzberg scales [14] were used. Data analysis began with the construction of a frequency polygon. When studying the statistical significance of differences, we used the calculation of the χ2 test with the Yates correction and the Bonferroni method for multiple comparisons. The critical level of significance of differences was taken to be less than 0.05 [15].
RESULTS AND DISCUSSION
Throughout the entire observation period, 117 (66.9%) patients with injuries to the talus, which were one of the components of PT, were delivered from Barnaul to the hospital, while during the same time period, isolated injuries to the talus were noted in 58 (33 ,1 %). Thus, injuries to the talus during PT occurred 2 times more often than isolated ones; the differences are statistically significant (p <
0.001). Table 1 shows the number of patients with isolated injuries of the talus and with PT, depending on the type of injury. All injuries to the talus under PT conditions occurred as a result of high-energy impacts - road accidents and catatraumas, while most of its isolated injuries were obtained as a result of low-energy impacts - household and sports injuries (Table 1).
Table 1.
Number of patients with isolated injuries of the talus and with PT depending on the type of injury
| Nature of damage | Type of injury | Total | |||
| Road accident | Catatrauma | Household | Sports | ||
| Isolated injury to the talus | 22 | 6 | 21 | 9 | 58 |
| Damage to the talus during PT | 75 | 42 | — | — | 117 |
| Total | 97 | 48 | 21 | 9 | 175 |
Table 2 shows the distribution of talar injuries according to Coltart's classification for isolated trauma and PT. Isolated injuries to the talus were represented in most cases by fractures of the body and neck of the talus without displacement, while the majority of injuries to the talus in PT were fractures of the body and neck with displacement, dislocations of the foot in the subtalar joint and complete dislocations of the foot (Table 2) .
Table 2.
Distribution of talus injuries according to Coltart's classification in isolated injuries and PT
| Nature of damage | Type of damage | Total | ||||||
| Body fracture | Cervical fractures | Subtalar foot dislocations | Complete dislocations of the ram | |||||
| no offset | with offset | Type I | Type II | III type | ||||
| Isolated injury to the talus | 28 | 4 | 14 | 3 | — | 9 | — | 58 |
| Damage to the talus during PT | 33 | 13 | 1 | 23 | 13 | 32 | 9 | 124 |
| Total | 61 | 17 | 15 | 26 | 13 | 41 | 9 | 182 |
Of 124 injuries to the talus during PT, open injuries were noted in 21 cases, while out of 58 cases of isolated injury - only in one, the differences are statistically significant (p <
0.01).
2 patients died, both with PT. The overall mortality rate for injuries to the talus was 1.1%, in patients with PT – 1.7%. In one deceased, the cause of death was edema and swelling of the brain due to an open craniocerebral injury, in another – acute massive blood loss, hemorrhagic shock due to blunt abdominal trauma with rupture of internal organs. Both deaths were not associated with damage to the talus. 51 somatic complications were noted in 34 (19.4%) patients. With isolated injuries of the talus, 5 complications were identified in 3 (1.7%) victims (deep vein thrombosis of the lower extremities in 3 cases, bronchopulmonary complications in 2 cases). In PT – 46 complications in 31 (17.7%) patients (in 19 cases – deep vein thrombosis of the lower extremities, in 15 – bronchopulmonary complications, in 9 – bedsores, in 2 – sepsis, in 1 – thromboembolism of the branches of the pulmonary artery ). In patients with PT, all somatic complications developed when the severity on the ISS scale was over 30 points, but their connection with the severity of injuries to the talus was not traced. The differences in the frequency of somatic complications in patients with isolated trauma of the talus and PT are statistically significant (p < 0.05). 22 local complications were noted in 20 (11.4%) patients: with closed injuries – 11 complications (6.9% of the total number of closed ones), with open ones – 11 (50% of the total number of open ones). Of the complications, 5 cases of instability in the ANF were noted, which led to secondary displacements, 5 suppuration of postoperative wounds, 5 ischemic necrosis of the wound skin edges, 6 soft tissue inflammations in the circumference of the transosseous elements of the ANF, 1 fracture of K-wires during transarticular fixation at the level of the joint space of the ankle joint The most common local complications were observed when using transosseous osteosynthesis of the ANF (10 cases), transarticular fixation of the ankle joint with K-wires (9 cases), open reduction and internal fixation with 3.5 mm cortical screws (2 cases), arthrodesis of the subtalar joint with screws with channel 7 .3 mm (1 case). There were no local complications with transcutaneous MIO using screws with a 4.0 mm channel. 1. Fractures of the body of the talus.
There were no complications with closed injuries; with open injuries, 4 local complications were noted: in 2 cases, inflammation in the wound area and in 2 cases, instability of transosseous elements.
All complications were observed during the treatment of ANF. The incidence of local complications in fractures of the body of the talus is 5.1%. 2. Fractures of the neck of the talus.
7 local complications were noted.
No complications were identified in type I neck fractures. In type II, 1 local complication was noted - instability of the transosseous elements of the ANF in a closed fracture. The frequency of local complications in type II is 3.8%. In type III - 6 local complications (for closed fractures - 5, for open fractures - 1). In closed fractures, local tissue inflammation in the area of transosseous elements of the ANF - 1, inflammation in the wound after open reduction and osteosynthesis with 3.5 mm cortical screws - 2, ischemic necrosis of the wound edges during open reduction and transarticular fixation with K-wires - 2. In open in fractures, inflammation in the wound area after PSO and osteosynthesis with 3.5 mm cortical screws – 1. The frequency of local complications in type III is 46.1%. 3. Subluxations or dislocations in the subtalar joint.
8 local complications were noted (for closed injuries – 5, for open ones – 3).
In case of closed injuries, inflammation of the soft tissues around the transosseous elements of the ANF - 1, ischemic necrosis of the wound edges during transarticular fixation with K-wires - 1, instability of the transosseous elements of the ANF - 1, relaxation during transarticular fixation with K-wires - 1, fracture of the K-wires in conditions of transarticular fixation – 1. In case of open injuries, inflammation in the wound area under conditions of ANF osteosynthesis – 2, with arthrodesis of the subtalar joint with screws with a 7.3 mm channel – 1. The frequency of local complications with subluxations and dislocations in the subtalar joint – 19.5%. 4. Complete dislocations of the talus.
Three local complications were noted, all with open injuries. Inflammation in the area of the postoperative wound during osteosynthesis of the ANF - 1, ischemic necrosis of the wound edges under conditions of transarticular fixation with K-wires - 1, inflammation in the area of the transosseous elements of the ANF - 1. The frequency of local complications in complete dislocations of the talus is 33.3%. Thus, the highest frequency of local complications was observed in type III fractures of the neck of the talus (46.1%), complete dislocations of the talus (33.3%), and subtalar dislocations of the foot (19.5%). Long-term treatment results were studied in 50 (38.6% of the initial population) victims from 3 to 6 years after the injury. The assessment was carried out using the AO FAS [16] and Matthies-Luboschitz-Schwarzberg scales [17]. Table 3 shows clinical outcome data according to the AO FAS scale. There were no excellent results; good results were observed in victims with fractures of the body and neck of the talus of types I and II. For type III talar neck fractures, subluxations and dislocations in the subtalar joint, the treatment results are satisfactory. No unsatisfactory results were noted (Table 3).
Table 3.
Long-term results of treatment of injuries of the talus according to AO FAS
| Nature of damage | Number of cases (n) | Average of the total AOFAS scores (M ± δ) | Result |
| Body fracture | 28 | 82 ± 3.7 | Good |
| Cervical fracture | 9 | 79 ± 3.9 | Good Good |
| Type I | 5 | 81 ± 2.9 | Good |
| Type II | 3 | 78 ± 2.6 | Good |
| Type III | 1 | 72 ± 0 | Satisfactory |
| Subluxations in the subtalar joint | 12 | 59 ± 6.9 | Satisfactory |
| Dislocations | 2 | 61 ± 9.9 | Satisfactory |
Table 4 shows clinical outcome data according to the Matthies-Luboschitz-Schwarzberg scale. Good results were observed in patients with fractures of the body and all types of fractures of the neck of the talus; satisfactory results prevailed in cases of subluxations and dislocations in the subtalar joint. No unsatisfactory results were noted (Table 4).
Table 4. Long-term results of treatment of injuries of the talus according to the Matthies-Luboschitz-Schwarzberg scale
| Nature of damage | Number of cases (n) | Average of the sum of points on the scale (M ± δ) | Result |
| Body fracture | 28 | 3.6 ± 0.4 | Good |
| Cervical fracture | 9 | 3.77 ± 0.2 | Good |
| Type I | 5 | 3.8 ± 0.2 | Good |
| Type II | 3 | 3.8 ± 0.16 | Good |
| Type III | 1 | 3.6 ± 0 | Good |
| Subluxations in the subtalar joint | 12 | 3.4 ± 0.3 | Satisfactory |
| Dislocations | 2 | 3.4 ± 0.3 | Satisfactory |
Satisfactory results were due to the presence of pain syndrome in patients, partial disability, the presence of signs of the formation of avascular necrosis of the talus, degenerative arthrosis of the ankle and subtalar joints.
CONCLUSIONS:
1. Damage to the talus during PT occurs from high-energy impacts and occurs 2 times more often than isolated ones. The largest share among them is occupied by dislocations and displaced fractures, open injuries, characterized by a more severe nature of the course. 2. Somatic complications with injuries to the talus in patients with PT are an order of magnitude more common (17.7%) than with isolated injury (1.7%). 3. The most common local complications of injuries to the talus were observed with open fractures (up to 50%), fractures of the neck of the talus type III (46.1%), complete dislocations of the talus (33.3%), subtalar dislocations of the foot (19.5 %) obtained from high-energy impacts in patients with PT. 4. In cases of severe general condition of patients with PT, as a temporary measure, patients are shown transarticular fixation with K-wires of the ankle and subtalar joints, which, unlike a plaster cast, provides more rigid fixation, free access to the injured limb, is simpler and more quickly performed, than ANF fixation. 5. Despite the fact that the majority of local complications were noted when using ANF osteosynthesis, it is almost impossible to use any other method of definitive treatment due to the nature of soft tissue damage in patients with severe open injuries of the talus during PT. 6. The results of using transcutaneous minimally invasive osteosynthesis with 4.0-mm screws with a channel for fractures of the body and neck of the talus allow us to recommend the method for wider use in patients with PT.
Funding and conflict of interest information
The study had no sponsorship.
The authors declare that there are no obvious or potential conflicts of interest related to the publication of this article.
LITERATURE:
1. Agadzhanyan VV, Pronskikh AA, Ustyantseva IM, Agalaryan AKh, Kravtsov SA, Krylov YuM, et al. Polytrauma. Novosibirsk: Nauka Publ., 2003. 494 p. Russian (Agajanyan V.V., Pronskikh A.A., Ustyantseva I.M., Agalaryan A.Kh., Kravtsov S.A., Krylov Yu.M. et al. Polytrauma. Novosibirsk: Nauka, 2003. 494 p. .)
2. Sokolov VA. Multiple and concomitant injuries. M.: GEOTAR-Media, 2006. 512 p. Russian (Sokolov V.A. Multiple and combined injuries. M.: GEOTAR-Media, 2006. 512 p.)
3. Bondarenko AV et al. Treatment of injuries to posterior part of the foot in polytrauma. Barnaul, 2021. 88 p. Russian (Bondarenko A.V. et al. Treatment of injuries to the hindfoot due to polytrauma. Barnaul, 2021. 88 p.)
4. Ruedi TP, Buckley RE, Moran CG. AO Principles of fracture management. New York: Thieme, 2007. Vol. 1-2. 947 p.
5. Nikitin NV. Diagnosis and treatment of foot injuries. K.: Phenix, 2005; 192 p. Nikitin N.V. Diagnosis and treatment of foot cysts. K.: Phoenix, 2005. 192 p. Russian (Nikitin N.V. Diagnosis and treatment of injuries to the bones of the foot. K.: Phoenix, 2005. 192 p.)
6. Foot surgery. Edited by Ardashev IP. Kemerovo: Siberian publishing group, 2021. 215 p. Russian (Foot surgery /edited by I.P. Ardashev. Kemerovo: Siberian Publishing Group, 2021. 215 p.)
7. Muller ME, Allgover M, Schneider R, Willinegger H. The manual for internal fixation: the technique recommended by AO group (Switzerland): translated into Russian, 3rd edition, revised and corrected. M.: Ad Merginem, 1996. 750 p. Russian (Müller M.E., Allgover M., Schneider R., Willinegger H. Manual on internal osteosynthesis: technique recommended by the AO group (Switzerland): translation into Russian. 3rd ed., additional and revised. M.: Ad Marginem, 1996. 750 pp.)
8. Talus fractures. Materials of the book by Schatzker J., Tile M. The rational of operative fracture care. Margo Anterior
. 1999; 5:3-7. Russian (Fractures of the talus. Based on materials from the book Schatzker J., Tile M. The rational of operative fracture care //Margo Anterior. 1999. No. 5. P. 3-7)
9. Talus fractures. Materials of the book Schatzker J., Tile M. The rational of operative fracture care. Margo Anterior
. 1999; 6:1-15. Russian (Fractures of the talus. Based on materials from the book Schatzker J., Tile M. The rational of operative fracture care //Margo Anterior. 1999. No. 6. P. 1-15)
10. Campbell's operative orthopedics. 11th ed. Edited by ST Canale, JH Beaty. Mosby Elsevier Philadelphia, Pennsylvania, 2008, pp. 4851-4870
11. Baker SP, O'Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J. Trauma
. 1974; 14(3): 187-196
12. Sokolov VA. Damage control – the modern concept for treatment of patients with critical polytrauma. Priorov Herald of Traumatology and Orthopedics
. 2005; 1: 81-84. Russian (Sokolov V.A. “Damage control” - a modern concept for the treatment of victims with critical polytrauma // Bulletin of Traumatology and Orthopedics named after N.N. Priorov. 2005. No. 1. P. 81-84)
13. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle hind-foot, mid-foot, hallux and lesser toes . Foot and Ankle Boarding
. 1994; 15(7): 349-353
14. Mattis ER. Estimation of outcomes of fractures of locomotor system bones and their consequences: the guidelines. M., 1983. 11 p. Russian (Mattis E.R. Assessment of the outcomes of fractures of the musculoskeletal system and their consequences: methodological recommendations. M., 1983. 11 p.)
15. Glants S. Medicobiological statistics: translated from English. M.: Practice, 1998. 459 p. Russian (Glantz S. Medical and biological statistics: translated from English. M.: Praktika, 1998. 459 p.)
View statistics
Loading metrics...
Links
- There are currently no links.
What treatment methods are used for necrosis of the femoral head?
When choosing a treatment method, the disease must be classified according to the so-called international ARCO classification:
- ARCO 0 necrosis of the femoral head: All images are negative in all examinations
- ARCO I necrosis of the femoral head: MRI and bone scintigraphy shows necrosis
- ARCO II necrosis of the femoral head: X-rays and CT scans show minor decalcification, MRI examination shows a typical area of necrosis.
- ARCO III necrosis of the femoral head: X-rays and CT scans show a break under the cartilage, later deformation of the femoral head occurs.
- ARCO IV necrosis of the femoral head: signs of joint wear (secondary arthrosis of the hip joint)
Osteochondral transplantation.
For osteochondral transplantation, cartilage tissue from the ipsilateral knee joint is most often used. Indications for transplantation are large and deep defects, often with the formation of a cyst, as well as the lack of effect from the surgical treatment methods proposed above. The possibility of using the calcaneal bone site at the Achilles-calcaneal joint as a source of tissue for osteochondral transplantation is currently being studied, with good early results.
The objective of the method is to restore the structural and biomechanical characteristics of damaged hyaline cartilage. This method is characterized by a long and difficult rehabilitation period. Morbidity of the donor site (pain in the knee joint after removal of columns of osteochondral blocks) is observed in 12% of cases. The technique itself is technically complex and time-consuming.
In clinical studies, the effectiveness of the method was estimated from 74 to 100% (average 87%).
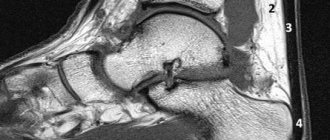
What are the benefits of using MRI?
MRI can make a diagnosis in the early stages. Making a diagnosis in the early stages is also the only way to restore or at least preserve the hip joint.
Computed tomography, like X-rays, only determines changes in bone structure and is therefore effective only in the later stages of the disease.
All three methods have been successfully used to determine the nature and extent of femoral head necrosis and to establish an accurate analysis and treatment plan.