Fracture of the talus is a rare and complex pathology. Accounts for less than 1% of skeletal bone fractures, less than 20% of foot bone fractures.
Fractures of the talus can be divided into fractures of the neck, body, head and processes.
Fractures of the neck of the talus are the most common (50%). They are a consequence of high-energy trauma (road accident, fall from height). The mechanism of injury is forced dorsiflexion of the foot and simultaneous axial load. Often accompanied by other fractures in both the lower leg and hip on the same side.
Fractures of the body of the talus account for 13-23%, most often the result of high-energy trauma, axial load in the position of pronation and supination of the foot.
Fractures of the head of the talus almost never occur in an isolated form.
Fractures of the external process of the talus account for 10-11% of fractures. Occur under the influence of axial load in the position of dorsiflexion of the foot, inversion and external rotation. Often found among snowboarders.
Fractures of the posterior process of the talus are the result of avulsion of a bone fragment by the posterior tibiotalar ligament, or the posterior portion of the deltoid ligament. The second mechanism of injury is often found in athletes, especially football players.
The talus has a complex anatomy and a small number of blood supply sources, which largely determines the difficulties in treating its injuries and often unsatisfactory functional results.
The Hawkins classification of talar neck fractures is based on the degree and direction of displacement, which in turn determines the degree of disruption of the blood supply and the risk of avascular necrosis.
| Hawkins 1 | undisplaced | 0-13% risk of avascular necrosis | |
| Hawkins 2 | Subluxation of the subtalar joint | 20-50% risk of avascular necrosis | |
| Hawkins 3 | Subluxation of the subtalar and tibiotalar joints | 20-100% risk of avascular necrosis | |
| Hawkins 4 | Complete dislocation of the talus | 70-100% risk of avascular necrosis |
Diagnosis of a fracture of the neck of the talus.
In addition to the clinical picture, radiographs are required for a complete diagnosis. In addition to the frontal and lateral projections, the Canale projection is used, which is optimal for visualizing the neck of the talus.
Canale projection in maximum equinus, pronation 15°, photograph taken at an angle of 75°.
In difficult cases, CT scanning is indicated.
In the case of an acute displaced fracture, closed removal of the displacement is indicated in all cases. If the position of the fragments is satisfactory (displacement less than 2 mm), conservative treatment is possible, plaster immobilization for 8-12 weeks, 6 weeks without putting weight on the leg.
In all cases of displaced fractures, open reduction and osteosynthesis are indicated.
For adequate visualization of the entire neck of the talus and quality control of reposition, it is recommended to use 2 approaches, anteromedial and anterolateral.
For the convenience of performing the operation, it is desirable to have a distractor, joysticks (Schanz screw + universal handle), and a headlamp for better lighting. If reduction is difficult, an extended approach through the medial malleolus is recommended.
After achieving reposition, preliminary fixation with knitting needles is performed. Often a zone of bone tissue compression is determined along the anterior-internal and anterior-outer surfaces. In this situation, the use of a bone graft or synthetic bone replacement material is indicated.
After X-ray control, final fixation of the fracture is performed with compression screws and/or plates and screws.
After open reduction and osteosynthesis, a 3-month period without load follows. It is necessary, if possible, to place the limbs in an elevated position and use local cooling. Development of active and passive movements from the first day after surgery.
Unfortunately, fractures of the neck of the talus are accompanied by a large number of complications. In 50% of cases, subtalar arthrosis develops, in 33% tibiotalar arthrosis. Depending on the degree of displacement, the risk of avascular necrosis increases. It can be identified by radiographs at 6-8 weeks after surgery, in the form of foci of sclerosis, against the background of a decrease in bone density in the area of the dome of the talus.
They are more rare than fractures of the neck of the talus. The principles of treatment remain the same - conservative treatment if the displacement is less than 2 mm and surgical treatment if more than 2 mm. Adequate visualization of the body of the talus will require an ankle osteotomy (usually the internal one).
After adequate reposition, preliminary fixation with knitting needles is performed.
For final fixation of the fracture, compression screws with a diameter of 3.5 and 4 mm are used, and, if necessary, plates.
Fractures of the body of the talus are characterized by the same complications as fractures of the neck.
This fracture is often confused with a common ankle sprain. The mechanism of injury is forced eversion with axial load on the hindfoot. This fracture is also often called a snowboarder's fracture.
It is not always possible to detect a fracture on conventional direct radiographs. In this situation, CT comes to the rescue.
For fractures of the lateral process of the talus, the Hawkins classification is used.
Fractures of the lateral process are always intra-articular, since the lateral process participates in articulation with both the calcaneus and the fibula. For this reason, if the fracture is displaced, surgical treatment is recommended. If the fracture is type B, then it is possible to perform open reduction and osteosynthesis; for type C fractures, resection of the lateral process is performed. In cases of symptomatic nonunion in chronic lesions, resection is also performed.
For surgical treatment, direct external access is used, directly under the apex of the outer malleolus. In cases where it is possible to perform osteosynthesis, the external process of the talus is fixed with one or two screws, 2.4 or 3.5 mm, depending on the size of the fragment. When the fragment is too small or fragmented, its resection is performed.
A fracture of the posterior process of the talus is characterized by several different mechanisms of occurrence. Depending on the mechanism, the morphology of the fracture differs.
The first mechanism is sharp dorsiflexion at the ankle joint. More often it occurs in athletes, either as a result of a sudden transition to a squatting position, or due to an unsuccessful landing after a jump.
The second mechanism is sharp dorsiflexion with simultaneous pressure on the area of the heel tubercle.
And the third mechanism is often found in football players and dancers, excessive dorsiflexion. To implement this mechanism, it is necessary to have an anatomically sufficiently large posterior process of the talus.
The diagnosis of a fracture of the posterior process of the talus is very often made untimely or not made at all. This is due to both a blurred clinical picture and visualization difficulties. During the clinical examination, a posterior impingement test is performed - the thumb and index finger of one hand are placed paraachillary and apply pressure towards the posterior process of the talus, while the other hand is plantarflexed. If the test causes pain, jamming, or crunching, all this indicates damage to the posterior process of the talus. Radiographs often reveal a triangular bone, which differs from a fracture of the posterior process by its smooth contours and rounded shape. It can also often cause pain along the back surface of the ankle joint, especially if its synchondrosis with the posterior process is damaged. In such cases, its removal is indicated.
For non-displaced fractures, conservative treatment is possible, consisting of plaster immobilization for a period of 6 weeks. If there is significant displacement or a large fragment, surgical treatment, open reduction and fixation with 1 or 2 screws are recommended. For comminuted or chronic fractures accompanied by severe pain, resection of the posterior process is recommended. In general, treatment is carried out according to the same principles as for the external process.
Classification of fractures
Based on the location of injury, they are divided into:
- Fracture of the neck of the talus.
This injury is the most common and is often combined with an ankle injury and ligament rupture. The reason is the dorsiflexion of the foot and the simultaneous load on it.
- Fracture of the body of the bone.
Accounts for 13% of all element injuries. The mechanism of occurrence is pressure during pronation or supination of the foot.
- Fracture of the lateral process of the talus.
Occurs under the influence of load on the arch of the foot during external rotation, often found in athletes involved in winter sports.
- Fracture of the posterior process of the talus.
This injury occurs after a fragment of bone tissue is torn off along with a ligament. People playing football can be injured.
What is osteochondritis of the talus?
Osteochondral injuries of the talus, sometimes also called osteochondritis, osteochondritis dissecans, or osteochondral fractures, are injuries to the cartilage and underlying structures of the dome of the talus. Osteochondritis of the talus is one of the causes of pain in the ankle joint, with which the patient turns to an orthopedic traumatologist. Osteochondritis of the talus often goes unrecognized and can lead to serious consequences if left untreated. For example, osteochondral lesions of the talus occur in 40% of ankle fractures.
Symptomatic osteochondral lesions of the talus often require surgical intervention. These injuries usually result from one or more traumatic events, resulting in partial or complete avulsion of a section of cartilage from the underlying bone. Such defects cause deep pain in the ankle joint with axial load, limited range of motion, impaired walking function, stiffness, a feeling of jamming of the joint, and swelling. These symptoms can cause limitations in physical activity and disability.
Treatment of ostiophytes
The preferred treatment for isolated symptomatic osteophytes is arthroscopic resection. In patients with clinical and/or radiological signs of significant degenerative changes, the indication for resection should be assessed with particular care. It is possible that osteophytes may re-form within a few months after surgery; the likelihood of recurrence depends on the patient's level of physical activity.
Removal of osteophytes is often performed as an additional intervention (when eliminating an osteochondral defect of the talus).
The purpose of treatment must be explained to the patient before surgery. In patients complaining of intense pain, the main goal of treatment is pain relief or elimination. The goal of treating patients with limited movement is to increase range of motion. The patient should be advised of the possibility of re-formation of osteophytes.
Osteophytes of the posterior surface of the tibia rarely cause limitation of movement, so they should be removed only if certain clinical symptoms are present. Resection of osteophytes on the posterior surface of the tibia is also technically challenging.
History of the study of osteochondritis of the talus.
The term "osteochondritis dissecans" was first published by Konig in 1888, which described the formation of a loose body in the knee joint as a consequence of fracture of the articular cartilage and underlying bone.
In 1922 Kappis described this phenomenon in the ankle joint. In 1959, the code Berndt and Harty proposed a radiological classification of these lesions, and although it has changed significantly since then, it is still widely used. Currently, the community of orthopedic traumatologists uses the term osteochondral injury of the talus (abbreviated OPTK) as the most accurately reflecting the essence of the problem, which is rarely reduced to a single injury (fracture), avascular necrosis (osteochondritis dissecans) or permanent microtrauma, but includes a combination of all of the above factors.
Anatomical studies conducted using cadaver material showed that the main mechanism leading to osteochondral fractures of the outer part of the dome of the talus is its forced inversion. Indication of injury occurs in approximately 85% of cases of OTC (Osteochondral Injury of the Talus), but in 15% of cases patients cannot associate the onset of pain with a traumatic event. Most often this occurs in cases where the source of damage is located on the posterior - inner surface of the talus. There are also cases of bilateral damage and identical damage observed in families or in identical twins, which indicates a possible genetic predisposition to avascular necrosis in some patients.
Treatment strategies for OPTK have undergone significant changes over the past 10 years. Conservative treatment for minor injuries includes functional offloading or plaster immobilization. Surgical treatment is intended for more serious injuries and includes excision, excision and curettage, excision + curettage + microfracture or reaming, installation of an auto- or allograft, antegrade and retrograde reaming, fixation of the fragment using bioabsorbable screws, autologous implantation of chondrocytes and some others. Below we will compare their effectiveness.
The goal of treatment for osteochondral lesions in all cases is to reduce pain, swelling, increase range of motion, and restore function. In many cases, several of the above techniques may be used, depending on the surgeon's preference.
Osteochondral injuries of the talus are a rare disease, but they are much more common in patients with a history of ankle fractures or ankle instability.
First aid
If an injury occurs, the patient should be given all possible assistance until the doctors arrive:
- Remove the load, lay or sit the victim.
- Remove tight shoes and clothing.
- In case of bleeding, stop the bleeding with a tourniquet until the pulsation stops, placing a note under it with the time of application. For arterial bleeding, a pressure bandage is applied above the injury site, for venous bleeding, below.
- Secure the leg using a splint or improvised objects.
- Apply cold to the foot for two hours, taking a break every 10-15 minutes.
- Offer a pain reliever after first finding out whether the person has an allergic reaction to the drug.
- Deliver the victim yourself to the nearest medical facility or wait for the ambulance to arrive.
You cannot set bone fragments or parts of tissue yourself, especially if the posterior process of the bone is fractured!
Pathophysiology of osteochondral injuries of the talus.
Anterior-external OPTCs are a consequence of inversion and dorsiflexion of the foot, they are characterized by a large area and are rarely deep. This is most likely due to the longitudinal direction of the injury force vector.
OPTK along the posterior-medial surface, on the contrary, are more often deep, cup-shaped, or accompanied by the formation of a cyst with a cap of cartilage on top. Apparently this is due to the vertical concentrated direction of the trauma force vector.
Thus, it becomes clear that osteochondral injuries of the talus are often combined with instability of the ankle joint, damage to the ligamentous apparatus of the ankle joint, and ankle fractures.
Anatomical studies have shown that the cartilage of the talus is 18-35% softer than the cartilage of the corresponding areas of the tibia. The thickness of the cartilage is inversely proportional to the load it experiences, which can also affect the location of the damage zone.
As studies have shown, the distribution of load in the ankle joint is disrupted when the defect size is more than 7.5\15 mm, which can be used to predict delayed results.
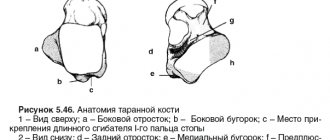
Anatomy
The talus is not injured as often as other elements of the human osteoarticular system. It is located between the heel and tibia bones, is small in size, but despite this it can withstand the weight and load of the body.
Despite the fact that there are no muscles attached to the process, it is necessary for the normal functioning of the foot.
Features of the structure:
- The surface of the bone part is covered with cartilage, the fracture of which leads to problems with the mobility of the foot.
- Poor blood circulation, so often the consequences of damage can result in prolonged fusion of fragments and lead to necrosis.
The composition of the bone in question:
- rear end,
- head,
- block.
The anterior part is connected to the navicular process, and the ankles are attached to the trochlea of the talus on both sides.
Classification of osteochondral injuries of the talus.
Radiological classification of osteochondral lesions of the talus by Berndt and Harty
CT classification of osteochondral lesions of the talus Ferkel and Sgaglione
MRI classification of osteochondral lesions of the talus Hepple.
Diagnostic measures
The following examinations will help to find out the reasons why the elements of the talus hurt:
- Collection of complaints and circumstances of illness.
- Visual inspection and palpation of the injury site.
- X-ray in several projections. The image must capture the entire foot to assess the severity of the injury.
- CT is a modern study that allows you to obtain information about the degree of displacement of bone fragments and determine the tactics of subsequent therapy.
- MRI - determines the presence of avascular necrotization.
Surgical treatment of osteochondral injuries of the talus.
Surgical treatment of OPTC depends on many factors: patient characteristics such as age, activity level, comorbidities, characteristics of the lesion itself such as its location, size, depth of the lesion, lesion morphology, duration. Basically, surgical treatment is based on one of three principles: 1) removal of the loose body with or without bone marrow stimulation through microfracture, reaming 2) preservation of cartilage through retrograde reaming, fixation of the fragment or replacement of the defect with cancellous bone 3) stimulation of the formation of new hyaline cartilage by due to osteochondral block transplantation, mosaic chondroplasty, allograft.
Rehabilitation
Recovery from injury takes a long time, since due to insufficient blood supply the bone takes a long time to regenerate.
Wearing the cast takes from 3 weeks to two months. At this time, you cannot lean on your foot. You need to move with the help of a cane or crutch.
Rehabilitation after fractures of the talus elements involves the use of several healing techniques.
Physiotherapy
Physiotherapy has an analgesic effect, increases muscle tone, preventing muscle atrophy, and reduces swelling of soft tissues.
Basic methods:
- magnet,
- electrophoresis with medicinal solutions,
- UHF,
- paraffin applications,
- ultraviolet irradiation.
Rehabilitation measures are carried out from the first days after injury and continue after removal of the plaster cast.
Medicines
Along with mechanical effects on the bone, painkillers, NSAIDs, a short course of diuretics, calcium, and vitamin and mineral complexes are additionally prescribed.
All medications must be prescribed by a doctor after determining allergic reactions and concomitant diseases.
Exercise therapy
Gymnastics is an integral component of rehabilitation activities. With forced immobility, the muscles and ligaments weaken, and elements of physical therapy are necessary to restore their functions.
Strengthening muscle tissue should begin before the cast is removed after consultation with a doctor. During the day, you can move your fingers, squeeze and unclench them, tense and relax the muscles on your sore leg.
Open surgery for osteochondral injuries of the talus.
When accessing the anterior-outer part of the ankle joint, it is necessary to remember the branches of the superficial peroneal nerve located in this area.
To access the posteromedial sections, it will be necessary to perform an osteotomy of the medial malleolus, while it is necessary to exclude damage to the tibial plateau, which bears the main axial load. Before performing an osteotomy, it is necessary to pre-drill for subsequent installation of screws fixing the osteotomized fragment.
Injury to the anterior and posterior tibial tendons, flexor pollicis longus tendon, great saphenous vein, posterior tibial artery and nerve should also be avoided. An alternative is to use two approaches at once - anteromedial and posteromedial, which allow visualization of up to 80% of the dome of the talus and avoid osteotomy of the medial malleolus.
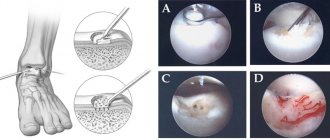
Currently, ankle arthroscopy has become widespread. Arthroscopic approaches are much less traumatic, which avoids the formation of rough postoperative scars and greatly facilitates rehabilitation. 2.7 mm arthroscopes allow visualization of the entire dome of the talus.
Removal, curettage and bone marrow stimulation.
After debridement, several channels are produced that communicate the defect with the bone marrow. This procedure can be performed using reaming or microfracturing. The purpose of the manipulation is to destroy the barrier of sclerotic subchondral bone that prevents the migration of stem cells from the bone marrow. As a result, a clot is formed, saturated with growth factors and stem cells, which is subsequently rebuilt into hyaline-like cartilage tissue. Most often used for stages 3-4 of the disease. The size of the defect should not exceed 1.5 cm. In clinical studies, the effectiveness of the method was estimated from 46 to 100% (on average 85%).
Osteochondral transplantation.
For osteochondral transplantation, cartilage tissue from the ipsilateral knee joint is most often used. Indications for transplantation are large and deep defects, often with the formation of a cyst, as well as the lack of effect from the surgical treatment methods proposed above. The possibility of using the calcaneal bone site at the Achilles-calcaneal joint as a source of tissue for osteochondral transplantation is currently being studied, with good early results.
The objective of the method is to restore the structural and biomechanical characteristics of damaged hyaline cartilage. This method is characterized by a long and difficult rehabilitation period. Morbidity of the donor site (pain in the knee joint after removal of columns of osteochondral blocks) is observed in 12% of cases. The technique itself is technically complex and time-consuming.
In clinical studies, the effectiveness of the method was estimated from 74 to 100% (average 87%).
Retrograde reaming.
This method will require the use of x-ray control and knowledge of the exact topography of the defect location. Retrograde reaming is the method of choice in the presence of a large subchondral cyst and with intact articular cartilage, as well as in cases of deep defect location, when it is difficult to reach it using the arthroscopic method. For medial defects, the entry point of the wire becomes the tarsal sinus. In clinical studies, the effectiveness of the method was estimated from 81 to 100% (average 88%).
Fixation.
Fixation of the fragment is performed only in cases of fresh extensive damage. The torn osteochondral fragment is lifted, the underlying bed is subjected to microfracture or reaming, and then the fragment is fixed using submersible absorbable screws or fibrin glue. The method is technically complex and its indications are quite narrow, but when it was used according to indications, a good result was observed in 89% of cases.
Thus, the most effective and technically simple method of treating the vast majority of osteochondral injuries of the talus at the moment is removal, curettage and bone marrow stimulation. Depending on the equipment of the operating room and the skills of the operating surgeon, this intervention can be performed either openly or arthroscopically.
Rehabilitation after surgery for osteochondral injuries of the talus.
Most authors adhere to the standard rehabilitation protocol, which recommends 6 weeks of immobilization after surgery using bone marrow stimulation. However, recently, work has appeared indicating that a 2-week period of immobilization is more than enough for small and medium-sized defects. Rehabilitation consists of training active and passive range of motion, muscle strength and muscle balance of the lower leg, reducing swelling and proprioceptive training.
Pain, a sensation of wedging, and swelling often persist for up to 1 year after surgery. After 6 months, it is advisable to perform an MRI control to assess the dynamics; in the presence of severe bone marrow edema, the prognosis is unfavorable. In such cases, progression of the lesion may further lead to the need for arthrodesis or ankle replacement.