Anatomical features of the lumbosacral spine
The spine is a complex motor system, without which normal human life is impossible.
While walking or sitting, there is a significant load on the sacral area, which increases the risk of various diseases of the musculoskeletal system. If a person does not engage in prevention, the first problems associated with the unfavorable state of the body begin in adulthood. They cause overload of the vertebrae - prolonged standing or bending, sitting and lifting heavy objects. What anatomical features are there in the lumbar region:
- The vertebrae follow each other, and an empty space forms between them. The spinal canal passes through this segment. In the area of the second lumbar segment is the end of the spinal cord.
- There are 5 spinal motion segments in the lumbar region. The last segment is formed from the 5th lumbar and 1st sacral vertebrae.
- The lumbar region contains the most massive processes of the vertebrae.
- There is a natural curve in the lumbar region called lumbar lordosis. In the sacral region there is a section directed backwards, and it is called kyphosis.
Depending on the individual case, the number of segments, their thickness or the presence of certain vertebrae may differ. This phenomenon is not dangerous to health and belongs to the category of tropism anomaly. Persons with anomalies need to more closely monitor the health of the musculoskeletal system.
Sacral spine - functions
The majority of a person's weight is distributed in this zone. It is this section that distributes the load to the lower parts of the body - the legs and pelvis. The main functions of the lower back include:
- Protecting the spinal cord and nerve roots from possible damage.
- Participation in the birth process.
- Cushioning effect during running, jumping and during heavy physical labor.
- Protection of the pelvic organs.
- Helps maintain balance.
- Redistribution of a person's weight to other areas.
- Mobility of the human body.
If there is a violation of the mobility and functionality of the lumbar or sacral areas, the patient experiences severe pain, a feeling of stiffness does not allow full movement. In complicated cases, paralysis, paresis and other pathological processes occur.
What internal organs is the sacral spine connected to?
- Pelvic bones and legs.
- Appendix, large intestine.
- Genital organs.
- Bladder.
- Sciatic nerve.
- Buttocks and thigh bones.
- Toes, feet, calf muscles.
- Rectum and anus.
If injury or mobility impairment occurs in any of the lumbar segments, problems may also arise in any of the internal organs that are located in the lower torso area. The patient may develop hemorrhoids, problems with blood circulation, a tumor process, swelling of the lower extremities, sciatica, cystitis, and problems in the genitourinary area.
Symptoms
At first, the disease may not manifest itself. Later, symptoms of lumbosacral osteochondrosis appear:
- pain of varying nature and intensity (from periodic aching painful sensations to acute attacks when a person cannot move or take a step), with frequent irradiation to the legs, groin area and lower abdomen;
- sensitivity disorders of varying severity (numbness, “crawling”, and so on);
- abnormal functioning of the pelvic organs (bladder, reproductive system, rectum and others);
- vegetative-trophic changes;
- muscle weakness, movement disorders, up to paresis and paralysis of the lower extremities.
In advanced cases of osteochondrosis of the lumbosacral region in men and women, infertility and serious diseases of the internal organs are diagnosed.
Causes of spinal diseases
There are some risk factors that predispose to the development of musculoskeletal diseases, including spinal injuries:
- Maintaining a sedentary lifestyle. In modern times, there is a special term for this phenomenon – physical inactivity. In the age of technological progress, when a person began to move to his place of work using transport, daily energy consumption decreased significantly, which led to a noticeable deterioration in the quality of health. Individuals with physical inactivity often experience poor circulation, weakness, obesity and muscle atrophy. The last point is directly related to back pain with the slightest exertion, including walking and sitting.
- Excessive physical labor. If a person works in hazardous work and is forced to lift heavy weights without proper training, over time he risks developing spinal injuries. This leads to the early course of osteochondrosis, sciatica, radiculitis, and hernias. Builders, loaders, and factory workers are at risk.
- Having flat feet or scoliosis. If the spine is curved, the load on the muscles is distributed incorrectly, which leads to serious deterioration, including imbalance and functional impairment. Against the background of flat feet, there is an incorrect distribution of the load along the foot, which also negatively affects the health of the spine.
- Pregnancy. During this position, a rapid and stressful restructuring of the mother’s body occurs. The heart, blood vessels, and internal organs are severely affected, and the functional indicators of many body systems deteriorate. The spine and connective tissues also suffer, because the ligaments and tendons become very soft. The lumbar vertebrae are most at risk from disorders. Rapidly growing body weight creates additional burden, so the back muscles are heavily overloaded. The stomach protrudes forward strongly to a large size, which changes the center of gravity forward, creating additional stress on the lower back. The result is severe pain. For this reason, many women experienced severe discomfort in the vertebrae during gestation. The use of support bandages partially alleviates the condition of the pregnant woman.
- Previous spinal injuries. If a person has had falls or injuries, then injuries lead to deterioration of the back condition over time. The risks of spinal hernias after physical injury increase significantly.
- There is no proper nutrition, there is excess body weight. Overweight people have an increased risk of problems with the lumbosacral region, since it bears a significant load. Also, obese people lack a strong muscular frame, so the back cannot cope with chronic overloads, which leads to damage to the vertebrae. An unhealthy diet is poor in minerals and vitamins, which negatively affects the health of the body.
- The presence of congenital pathologies. Some intrauterine deformities contribute to the appearance of deterioration in the musculoskeletal system and vertebral bodies already in adulthood.
- Age factor. It is important to take into account that as the body ages, disorders of the musculoskeletal system arise that are associated with degenerative processes in the body.
If you experience discomfort in the spine, it is important to consult a doctor promptly. Health problems are indicated by persistent lumbar pain, a feeling of stiffness, lumbago in the feet, and numbness in the limbs. During the diagnosis, the specialist questions the patient and prescribes an MRI or X-ray. The results of such a study ensure the correct diagnosis in most cases. Then appropriate treatment is prescribed.
What types of diseases occur
Most often, during the examination, the following pathological conditions of the spine can be detected in the lower back:
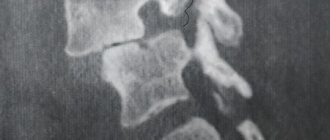
- Osteochondrosis of the lumbosacral spine. This is a degenerative change in the joints of the spine, causing damage to cartilage and bone tissue. Very often, osteochondrosis occurs as we age, since with age the intervertebral discs wear out, leading to discomfort and pain. Signs of spinal disease are stiffness, pain and burning at the site of the spinal lesion. In advanced cases, urinary incontinence and lumbago in the lower extremities occur. Over the years, pathology greatly worsens the quality of life, so treatment is necessary, requiring a comprehensive solution to the problem.
- Spondylosis. If there is too intense stress on the tailbone and lower back, then over time the height of the intervertebral discs changes downward. Spine-shaped articular processes appear on the sides of the vertebrae, which injure the cartilaginous plates and can compress areas of the spinal canal. As a result, the disease can lead to serious neurological disorders and pain. A patient with spondylosis usually complains of pain, stiffness and numbness in the lower back.
- Protrusion of the lumbar vertebrae is one of the stages of development of an intervertebral hernia. Before a true intervertebral hernia occurs, unfavorable pathological changes appear in the fibrous ring located in the intervertebral disc. When the fibrous ring is stretched with gradual leakage of the nucleus pulposus outward, protrusion is diagnosed. At this stage, you can still get rid of the protrusion non-surgically. There are techniques that allow you to correct the protrusion. Not all cases of protrusion cause symptoms, so they may not exist. Signs of the disease include pain and stiffness.
- A hernia is a more advanced form of protrusion. When a lumbar hernia occurs, serious health problems arise due to the complete protrusion of the contents of the fibrous ring into the cavity of the intervertebral disc. The condition is associated with severe discomfort and pain, often causing lumbago and a feeling of stiffness in the lower extremities. If treatment is not started in a timely manner, the patient will lose his limbs and lose sensation in his toes.
- Sciatica. This is a form of radiculitis, manifested by an inflammatory process in the sciatic nerve. A patient with sciatica cannot move normally, stand or walk for a long time, and even lie down with discomfort. The patient constantly feels lumbago and pain.
Also, some patients experience arthrosis, arthritis and the consequences of lordosis. Most diseases have one common symptom - lower back pain. If discomfort persists for a long time, you should definitely visit a doctor.
Causes of lumbosacral osteochondrosis
The etiology of the disease is not fully understood. Osteochondrosis of the lumbosacral spine develops under the influence of the following reasons:
- burdened heredity;
- injuries (bruises, fractures, etc.);
- natural aging and “wear and tear” of the elements of the lumbosacral zone;
- sedentary lifestyle, prolonged static loads on the spine;
- poor nutrition, with insufficient intake of microelements, vitamins and fluids;
- increased load on the lumbosacral region (professions associated with physical labor or sports, walking in high heels, and so on);
- obesity;
- "metabolic diseases";
- autoimmune diseases, in which aggression is directed at the cells of the connective system;
- infections and intoxications;
- any factors causing a lack of innervation and blood supply to the lumbosacral spine;
- bad ecology;
- emotional overstrain (stress);
- pathology of the musculoskeletal frame (flat feet, osteoporosis, rickets, etc.).
The lumbosacral area experiences enormous stress in women during pregnancy and childbirth. Osteochondrosis often develops in professional athletes who abruptly stop training.
Drug treatment of lumbar vertebrae
Spinal diseases have periods of exacerbation, which manifest themselves in the form of acute and crippling pain in the lower back. To alleviate the condition, symptomatic drug therapy is usually prescribed, aimed at alleviating the patient's condition. What means are used:
- NSAIDs or analgesics. Nonsteroidal anti-inflammatory drugs help relieve inflammation and severe lower back pain. Usually, injectable forms are prescribed for use for 2-3 days, after which they switch to tablets. These drugs are not suitable for long-term use, as they have a relatively high degree of gastrotoxicity (harmful to the stomach), so people suffering from stomach ulcers or gastritis should use them with caution, using the most gentle means. Examples of trade names are Diclofenac, Movalis, Nimesil.
- Muscle relaxants. Often, back pain is associated with a pathological and painful muscle spasm that causes severe discomfort. To eliminate severe pain, you need a course of muscle relaxants. In severe situations, short-term use of tablets is ineffective, so they must be taken for at least 3-4 weeks. Examples of trade names are Baclofen, Sirdalud, Mydocalm.
- Neurotropic B vitamins. These drugs are prescribed for sciatica or lumbago, when the pain syndrome is associated with pinching of the sciatic nerve or nerve roots in the spine. B vitamins in combination, namely thiamine (B1), pyridoxine (B6), cyanocobalamin (B12), which in large doses have an analgesic effect. Medicines are used in courses - injection solutions are administered over 1-2 weeks, and then switched to tablets. Oral forms of release are taken for two months to consolidate the result. Examples of drugs are Milgamma, Neurobin, Neuromax.
- Corticosteroids. This group of drugs belongs to hormonal drugs and has a large list of side effects, so they are prescribed in difficult situations. If the patient suffers from severe pain that cannot be relieved by using NSAIDs, then a corticosteroid is administered through an intra-articular injection. An example of an effective remedy is Diprospan. Under the supervision of an ultrasound sensor, an injection solution is injected into the interarticular cavity, which has a long-lasting effect. Usually, one injection is enough to relieve symptoms of pain for a long time. If for some reason it is impossible for a patient to receive a Diprospan injection, it is recommended to carry out a novocaine blockade. This is a non-hormonal agent with a powerful anesthetic effect.
Medicines to maintain the health of the lumbar back
When the period of exacerbation has passed, doctors recommend using medications that support the patient’s health condition in order to minimize the risks of a recurrent attack. These medications include:
- Chondroprotectors. These are medications aimed at maintaining the health of cartilage tissue, successfully used in the treatment of degenerative processes associated with age-related deterioration. Most often, the use of chondroprotectors is recommended in the presence of joint diseases and the progressive development of osteochondrosis. These drugs are used as a long-term course of treatment for several months or more. First, injectable forms of release are prescribed, used for several months. Then they switch to tablets, which need to be taken for 3-6 months without a break. After which they take a short rest and then use chondroprotectors again. It is important to understand that these drugs do not reduce the risk of degenerative destruction of the vertebrae. They nourish cartilage tissue, and therefore slow down the rate of progression of osteochondrosis. The active ingredients are glucosamine and chondroitin. Examples of medicines are Dona, Chondrogard, Mukosat.
- D3 supplements, calcium. There are specific supplements with a strong evidence base used to support bone tissue at any age. In particular, such supplements are needed by people who are at risk for diseases of the musculoskeletal system - postmenopausal women, people suffering from osteoporosis and children during a period of intensive growth and development of the body. Calcium and vitamin D3 support healthy bone tissue. The first component will not be able to be absorbed normally in the intestines if the patient has cholecalciferol deficiency, so it is recommended to use combined supplements. Examples - Calcium D3 Nycomed, Calcium Citrate with D3, Calcemin Advance. It is advisable to prescribe such drugs for prevention to vulnerable segments of the population or after testing.
- Multivitamin and mineral complexes. Serve as an addition to the daily diet and are not mandatory for use. If the patient’s diet is depleted in vitamins and minerals, then the doctor may prescribe appropriate supplements in periodic courses to prevent hypovitaminosis.
Less commonly prescribed are homeopathy and antispasmodics. External agents in the form of ointments and gels are also often used.
Methods of treating lumbosacral osteochondrosis
Therapy always begins with a set of conservative measures. Treatment of osteochondrosis of the lumbosacral spine is based on 4 areas:
- local impact;
- systemic drug therapy;
- vertebroneurological techniques;
- reflex methods.
Therapeutic tactics for osteochondrosis of the lumbosacral region are always based on the individual characteristics of the patient. It usually includes therapeutic exercises, water exercises, massage, spinal traction, physiotherapy and pharmaceuticals. In case of severe intractable pain, blockades are indicated. In severe cases, surgical intervention is resorted to.
Drug treatment
The medicinal treatment procedure is prescribed by a doctor. Thus, treatment of osteochondrosis of the lumbosacral region may include several types of local and systemic drugs. In the acute period, the most important is spinal immobilization and pain relief. They always begin to relieve a pain attack with non-steroidal anti-inflammatory drugs and analgesics. Additionally, muscle relaxants, antispasmodics, B vitamins, diuretics and other groups of drugs can be used.
During remission of osteochondrosis of the lumbosacral region, chondroprotectors, agents that improve tissue trophism, vitamin and mineral complexes, etc. are used. Preventive courses help prevent exacerbations.
Surgical treatment
If lumbosacral osteochondrosis does not respond to conservative therapy and continues to progress, surgical intervention is recommended for the patient. The extent of the operation will depend on the severity of the existing changes and the presence of complications. In advanced cases, the affected areas of the spine are replaced with implants.
Folk remedies
Osteochondrosis of the sacrolumbar spine in the early stages can be treated not only with traditional methods, but also with the use of folk recipes. At home they often use:
- compresses;
- wraps;
- rubbing;
- baths;
- teas with medicinal herbs.
Compresses with sea salt, honey, radish, horseradish, red pepper and natural healing mud have proven themselves well.
But still, for osteochondrosis of the sacro-lumbar spine, the best option would be if a person makes an appointment with a doctor.
Diet and exercise therapy
Almost always (with the exception of complicated osteochondrosis), treatment of the sacral spine includes physical exercise and proper nutrition. With concomitant obesity, the diet will be aimed at weight loss. And with food, a person should receive in sufficient quantities all the necessary vitamins, microelements and nutrients. The role of vitamin D, phosphorus and calcium is especially important. In order to have a positive effect on cartilage cells, meat broths, fish dishes, and jellied meat are recommended.
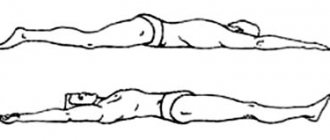
A set of exercise therapy exercises is developed by a specialist for each specific patient. Its main tasks are:
- strengthening the muscles around the affected segments of the lumbosacral area;
- spinal traction.
After training, a therapeutic massage will be useful.
Non-drug treatment
When a patient experiences an attack of acute pain in the vertebral area, supportive conservative treatment is recommended. What methods of preventing exacerbation of the disease help:
- Massage. Using special techniques, the massage therapist warms up the muscles and relieves tension. Local blood flow also improves, so after a course of massage the patient temporarily stops feeling pain in the lumbar vertebrae.
- Physiotherapeutic treatment. With the help of hardware technology and the use of medications, the inflammatory process is eliminated and chronic discomfort in the lower back goes away. Recommended hardware techniques are magnetic therapy, electrophoresis, shock wave therapy.
- Manual practice. This is a branch of alternative medicine that allows you to “straighten” the vertebrae to their natural position. The concept of the teaching is that if the vertebrae are in the wrong position, misalignment occurs throughout the body, which leads to back problems. Manual therapy cannot be performed if there is a large hernia.
- Physiotherapy. With the help of sports activities, it is possible to tone the muscles, which removes most of the stress from the vertebrae. As a result, the discomfort goes away almost completely. It is important to do the exercises daily. The exercise therapy complex is selected individually with an instructor, taking into account the diagnosis.
- Wearing orthopedic shoes and elastic corsets. Properly selected bandages and shoes will help relieve stress on target muscles that are not strong enough to compensate for discomfort in the vertebrae. The duration and timing of wearing should be recommended by the attending physician. Clothing models and sizes are also chosen based on recommendations.
If the situation is advanced and conservative methods of therapy do not help, surgery is required.