Arthrosis of the knee joint, along with arthrosis of the hip joint, is one of the most widespread degenerative diseases of the musculoskeletal system. At the age of 50, arthrosis of the knee joint already occurs in 40% of the population, and this figure gradually increases with age.
Considering the high prevalence of osteoarthritis of the knee joint, a progressive treatment algorithm has been developed, including: modification of physical activity, physical therapy, physiotherapy, intra-articular and periarticular injections of glucocorticosteroids, hyaluronic acid preparations, platelet-rich plasma, and in the absence of effect from these conservative measures - surgical treatment.
Surgical treatment of primary arthrosis of the knee joint includes two main groups of operations – endoprosthetics and corrective osteotomies. Arthroscopy for primary gonarthrosis is characterized by low effectiveness and often does not provide even temporary relief.
In the presence of deformity in the knee joint and predominant damage to one compartment (half) of the knee joint, corrective osteotomies allow you to get rid of pain while preserving your own joint.
Below we will consider the indications and contraindications for this operation, the correct selection of patients, surgical technique, fixation methods and possible complications.
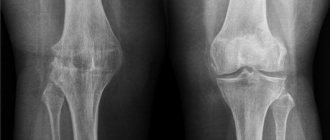
Disruption of the mechanical axis in the knee joint causes uneven load distribution and asymmetric wear of the articular cartilage. Arthrosis with varus deformity of the knee joint (legs with a “wheel”) is more common; with this form of arthrosis, wear occurs in the internal part of the knee joint.
Contraindications to high valgus osteotomy of the tibia:
- body mass index over 35
- knee instability
- extension contracture more than 15 degrees
- flexion contracture (more than 60 degrees)
- severe arthrosis of the patellofemoral joint
With proper patient selection, the effectiveness of high valgus osteotomy of the tibia is extremely high. The 10 year survival rate is 92%. Corrective osteotomy may be complemented by procedures aimed at restoring articular cartilage in the medial compartment of the knee joint.
According to a study by Schallberger in 2010, which retrospectively analyzed the long-term results of treatment of medial knee arthrosis using high valgus osteotomy, the 5-year survival rate was 98%, 10-year 92%, 15-year 71%. In total, total arthroplasty was required in the long term in 24% of cases. Patient satisfaction was 80%, the average VAS score was 0, and radiologically there was an almost complete absence of arthrosis progression.
Knee Surg Sports Traumatol Arthrosc. 2011 Jan;19(1):122-7. doi:10.1007/s00167-010-1256-4. Epub 2010 Sep 7.
High tibial valgus osteotomy in unicompartmental medial osteoarthritis of the knee: a retrospective follow-up study over 13-21 years.
Schallberger A1, Jacobi M, Wahl P, Maestretti G, Jakob RP.
So, if your knees are not aligned and your legs are shaped like a wheel, you are physically active, and your knee pain is associated with primary medial arthrosis, a high valgus tibial osteotomy is your choice.
Possible complications
Some complications arise already during osteotomy, others during the rehabilitation period.
- Incorrect fusion of bones. Occurs due to improper fixation of bone tissue fragments during surgery. With such a complication, repeated intervention is necessary.
- Non-union of bones. It may occur due to severe concomitant pathologies, smoking, impaired blood supply to the operated area, or osteoporosis. For treatment, a repeat operation is performed and special rehabilitation is prescribed.
- Compartment syndrome. Occurs if, during surgical manipulation, the muscles were strongly compressed by a tourniquet. For treatment, certain drugs are prescribed; if the case is severe, a fasciotomy is performed.
- Improper functioning of the joints located next to the surgical field. This complication is typical for the absence or violation of rehabilitation rules. Exercise therapy is prescribed.
- Infections. They can be introduced during surgery or due to improper wound care. An antibiotic is prescribed for treatment; in severe cases, revision surgery will be required.
- Nerve damage is a surgeon’s mistake or a peculiarity in the location of the patient’s nerve endings. The function of a damaged nerve cannot be restored.
- Thromboembolism. Occurs when anticoagulants are prescribed incorrectly, getting out of bed late, or the inability to wear compression stockings. To eliminate this complication, high doses of antiplatelet agents and anticoagulants are needed.
Recovery period
Consolidation of the osteotomized area occurs no earlier than after 4 months, so the rehabilitation regimen prescribed by the doctor must be carefully followed during this entire time. Complete healing of the fracture, since the physiology of each individual organism is unique, is observed in patients at different times. But on average, the bone heals within 4-6 months.
Throughout the entire postoperative period, you should strictly adhere to the orthopedic regimen: dosed bed rest, walking on crutches without relying on the problematic leg, a ban on certain types of movements and body positions, exercise therapy, etc. Let us emphasize that an integral measure for successful recovery is physiotherapy. Without it, it is impossible to fully restore the balance of the muscles responsible for the functioning of the musculoskeletal system. Physiotherapy and massage procedures are also prescribed for a speedy recovery.
To relieve postoperative pain and inflammation, the patient is prescribed medications from the NSAID series. A specially selected course of antibiotic treatment is required to prevent infection. Among the medications, calcium and vitamin D preparations, stimulants of repair processes, B vitamins, and antiplatelet agents are also recommended.
Only after complete consolidation has been confirmed by x-ray is it possible to walk, fully relying on the limb. Premature axial loading leads to complications, which are often eliminated solely by reoperation.
Derotational method
The essence of the method is to eliminate the pathological rotation of the bone relative to the joint, which causes problems with walking. Abnormal rotation is medically called rotational dysplasia. The pathology is characterized by excessive antetorsion, accompanied by decentration of the femoral head in relation to the acetabulum. The clinical situation is reflected mainly in the gait: since the leg is internally rotated, the gait acquires typical signs of clubfoot. Such a disorder can also predispose to hip joint dislocation and pain. Femoral derotation surgery is designed to reduce the antetorsion angle to normal levels. The effect is achieved by performing a subtrochanteric transverse osteotomy with fixation of the restored area (with knitting needles, screws, etc.) for its successful fusion in an intact position.
Preparatory stage
In the preoperative period, a thorough examination of the patient is carried out. Preparation includes passing:
- X-rays of the problematic joint (if necessary, send for CT, MRI);
- electromyography;
- ichnometry, podography;
- electrocardiograms;
- general, biochemical blood test;
- clinical urine analysis;
- coagulograms;
- rheumatoid factor test;
- studies of calcium-phosphorus metabolism;
- test for the rate of remodeling, formation of new bone tissue;
- fluorography;
- examination by an anesthesiologist and individual doctors of narrow specialization (cardiologist, endocrinologist, etc.).
The day before the intervention, you should stop eating for about 8-12 hours. At night and immediately before the procedure, the patient is given an enema to cleanse the intestines.
Operation process
Surgical treatment begins with the administration of anesthesia. The specific type of anesthesia to use is determined by the anesthesiologist at the stage of preoperative preparation. As a rule, this is general anesthesia. A separate category of patients may be prescribed spinal or epidural anesthesia. The surgical process takes place under X-ray control.
- During the intraoperative session, the surgeon makes a long, deep soft tissue incision layer by layer in the projection of the affected joint.
- The cut skin and muscle structures are pulled apart and fixed with a retractor, which will additionally protect them and the neurovascular bundles from iatrogenic damage during the manipulations performed.
- After a wide exposure of the bone fragment in need of correction, the specialist begins osteotomy. The dissection of the bone plate is performed with an osteotome or chisel.
- First, on the line of the intended cut on the bone, notches (approximate marks with a preliminary deepening) are made with the blade of the working tool. Then they move on to the main osteotomy.
- To create a cutting effect, a gentle impact of a surgical hammer is used on the anvil of the handle of an osteotome or chisel. To ensure that the mechanical force is concentrated correctly, a special base in the form of a roller is placed under the dissection area.
- After the osteotomy has been performed, the bone fragments are juxtaposed in the correct position and sequentially secured with osteosynthesis devices.
- At the end of the operation, the surgical field is cleaned and the expander is removed from the wound. This is followed by disinfection and layer-by-layer suturing of the wound with installation of drainage. If fixation is adequate, plaster immobilization is not required.
Treatment by the best specialists
will do everything to make your treatment as effective as possible. We cooperate with leading German clinics and can recommend a doctor who specializes in your problem. One of the unique German doctors whose specialization is osteotomy is Doctor of Medical Sciences, orthopedic traumatologist Sven Scheffler. His assets include:
- cooperation with the Olympic Sports Center;
- creation of a unique new concept “Return to Sports!”;
- treatment and rehabilitation of players of professional football clubs in Germany, Russia, Ukraine, Belarus, etc.;
- treatment and rehabilitation of professional handball players, volleyball players, gymnasts, boxers, etc.;
- annual performance of about 800 surgical interventions;
- active scientific activity (author of more than 50 scientific papers).
Dr. Scheffler is a worthy representative of world-famous German medicine. He treats both professional athletes and ordinary people. Our specialists will help you get treatment from the best doctors in Germany!
Why is it worth coming to Germany for treatment?
In addition to the general reasons and advantages of treatment in Germany, which we described in this section of the site, in Germany doctors never refuse to treat patients who have already come to their clinic for treatment. If the doctors agreed to accept you for treatment, then they will not send anyone home, but will fight until they defeat the disease. When deciding on the need to use a particular technique, German doctors proceed from the patient’s condition and the appropriateness of treatment, but never refuse further treatment only because of the patient’s age or condition, as is often the case in post-Soviet countries. If it becomes obvious that it is no longer possible to stop the progression of the disease, the patient is offered a well-thought-out program to alleviate suffering and remove pain as much as possible.
Types of intervention
Surgery can be closed or open. Closed osteotomy involves manipulation of an osteotome from a minimal approach (skin incision is 2-3 cm) without exposing the bone. The open technique is based on the use of a wide approach (incision length 8-12 cm) with exposure of the bone segment, which will be intersected using an osteotome.
- Closed tactics.
It is used in isolated cases, mainly using the cross-sectional method. Despite being minimally invasive, the procedure is associated with an increased risk of damage to nerve trunks and large vessels due to poor visualization of the surgical field. With a closed approach, muscle dissection, skeletonization (separation of the periosteum) and bone intersection, roughly speaking, occur blindly. - Open osteotomy
. This surgical tactic is more in demand in orthopedics. The overview of the operated area is quite sufficient to work with cutting instruments with high precision, without contacting important neurovascular formations. Experts note that with more extensive invasion in relation to the musculocutaneous structures, open technology in some cases turns out to be more productive and much safer.
Surgery using the osteotomy method is widely practiced both in Russia and abroad. The price in Moscow for it is from 40 thousand rubles. In Germany, the simplest intervention is performed for 15,000 euros. In Israel, prices are approximately as follows: procedure 1 tbsp. complexity costs about 20 thousand dollars, and, for example, for lengthening one leg - from 55 thousand. e. and higher.
Based on the purpose, interventions are classified into 4 main types:
- corrective surgery to correct deformity;
- intervention to lengthen/shorten the bone;
- derotational procedure – correction of pathological rotation of a bone element;
- to improve support functions.
Specifically, the process of osteotomy itself, depending on the purpose, can be implemented according to one or several technical methods. The techniques are characterized by the geometric features of the bone fracture line. Initially, there are 2 options for performing an artificial fracture - linear and figured. They include the following subtypes:
- transverse
- the guide line is straight and runs horizontally; - oblique
- an inclined cut is made in different planes at a certain angle; - z-shaped
– the strip cutting the bone segment resembles the letter “Z”; - staircase -
the dissection of the bone has a stepped shape; - spherical
- the fracture site is a smooth arcuate curve; - angular -
the intersecting line consists of two rays forming an angle, the apex of which is directed downwards; - wedge-shaped
- a combination of two oblique incisions or a combination of oblique and transverse views with the release of a bone wedge.
Osteotomy is not an operation that solves the problem of coxarthrosis once and for all! It only helps to slightly improve the patient’s quality of life and help reduce the progression of degeneration. Destruction of the cartilage of the articular surfaces in the final stages (stages 3-4) is an absolute indication for prosthetics.