Patellofemoral arthrosis is an extremely common pathological condition characterized by damage to the cartilaginous part of the articulation of the patella and femoral bone. This diagnosis is made when signs of disruption of the structure of cartilage tissue appear against the background of any physical activity.
At this stage of arthrosis development, the appearance of acute symptoms that could negatively affect the patient’s quality of life has not yet been observed. Most often, this pathological condition manifests itself in young patients between 25 and 35 years old. The occurrence of signs of arthrosis cannot be ignored, because progression of the disease can cause impaired joint mobility and disability.
What is it and why does it occur?
The kneecap, i.e., the patella, is adjacent to the cartilaginous surface of the femur, forming the patellofemoral articulation. The development of arthrosis of the patellofemoral joint is diagnosed when an inflammatory process begins in this area. Normally, the patella, which is connected to the joint by tendons and ligaments, does not come into contact with the femur when the joint moves.
However, under the influence of various unfavorable factors, destruction of the patellar cartilage and damage to the cruciate ligaments occurs. Because of this, pathological friction of the cup and femur is observed. This leads to the appearance of an inflammatory process. In the future, this violation becomes the cause of critical damage to the cartilaginous surface of the patella and the development of patellofemoral arthrosis of the knee joint.
Most often, the appearance of this pathology is the result of systematic physical overload of the knee joint during active sports, prolonged standing, carrying heavy loads, etc. Other factors that increase the risk of developing this pathology include:
- age-related decrease in the elasticity of connective tissue;
- endocrine disorders;
- wearing uncomfortable shoes;
- knee injuries;
- congenital pathologies of the structure of the joint elements and muscles of the thigh;
- infections;
- excess weight;
- rheumatoid arthritis;
- muscular dystrophy.
In fact, any load that can cause the kneecap to move relative to its axis can trigger the appearance of patellofemoral syndrome.
If treatment is not started in a timely manner, the disease progresses to osteoarthritis, accompanied by damage not only to the cartilaginous surfaces, but also to the head of the femur.
Patellofemoral arthrosis of the knee joint: Conservative treatment
Most injuries to the posterior surface of the patella are treated with conservative methods. For example, such a temporary pathology as “runner's knee” occurs in younger patients and is treated by selecting the right loads and physical therapy. When diagnosing this injury, you should avoid unnecessary training loads, as pain on the front side of the knee may occur again.
Physiotherapy and lifestyle adaptations
The symptoms of patellofemoral arthrosis are stabilized by strengthening the thigh muscles, as well as losing excess weight. Patellar pain can be reduced by avoiding activities such as squatting and climbing stairs. Muscle stretching exercises improve the lateral (side) mobility and movement of the patella in the patella surface of the femur.
Orthopedic prostheses
For severe pain in the patella, orthopedic prostheses (orthoses) help, which temporarily limit the mobility of the patella and relieve it of stress. The specialists of our clinic will provide you with qualified assistance when choosing this type of treatment for pain syndrome.
Pain therapy and medications
The progress of the disease is controlled with the help of painkillers and anti-inflammatory medications (non-steroidal anti-inflammatory drugs).
Injection treatment
For complex inflammations, a cortisone injection helps. However, this method is not recommended to be used constantly. Injections of intra-articular lubricant (hyaluronic acid) improve the gliding ability of the knee joint, but are not used as a form of etiotropic therapy for retropatellar arthrosis. This form of treatment can be successful only if there is a certain amount of articular surface, as well as with a long-term positive result.
Limits of conservative treatment
When there is no cartilaginous surface and bones rub against each other, conservative treatment is almost powerless. Highly qualified orthopedic surgeons at the Gelenk-Klinik will consider each case individually and try to help the patient using conservative methods. If the doctor determines that conservative treatment will not bring the desired result, the patient will be offered other forms of treatment for patellofemoral pathology.
Classification by degree
The main classification of this pathological condition is based on the severity of damage to the elements of the articulation:
- With grade 1 patellofemoral arthrosis, even X-rays do not reveal any signs of disruption of the integrity of the cartilaginous surfaces. At the first stage of the disease, there is already an inflammatory process, which is accompanied by the appearance of minor symptoms.
- With stage 2 of the pathological process, X-rays reveal signs of an increasing degenerative process that spreads to large areas of cartilaginous tissue. At this stage of the pathology, the appearance of severe symptoms is already observed.
- In grade 3, x-rays show extensive degenerative changes in the cartilaginous surfaces of the patella and femur. In addition, there are pronounced signs of damage to the head of the bone. In the third stage, the disease is accompanied by acute symptoms and limited joint mobility.
Transplantation of autologous cartilage cells
Autologous cartilage cell transplantation involves transplanting the patient's autogenous articular cartilage into the damaged area behind the patella. This method makes sense only when only one articular surface is damaged. If both articular surfaces are damaged, this method of surgical treatment is not performed.
With minor damage to the cartilage, it is possible to grow it again. During arthroscopic surgery, a small portion the size of a grain of rice is separated from the less congested retropatellar cartilage. Using the resulting cartilage mass, a large number of cartilage cells are formed in a special laboratory. After 6-8 weeks, these cells are transplanted to the affected areas behind the patella. After about 3 months, strong cartilage tissue with stable hydraulic permeability is formed from cartilage cells. Transplantation of autologous cartilage cells is suitable for younger patients. Regeneration of the cartilage surface prevents arthrosis diseases, as well as the implantation of a patellofemoral prosthesis.
Patellofemoral Partial Prosthesis: A metal implant on the hip between the two femoral condyles covers the patellofemoral surface of the femur. The connection of the polyethylene and titanium implant on the back of the patella forms a sliding surface. Our specialists prefer HemiCAP designs to cemented implants. © 2med
Medical request
Symptoms that appear
At the initial stage of development of this disease, clinical manifestations are mild, which makes diagnosis difficult. First, the appearance of pain is observed after physical exertion. Unpleasant sensations quickly disappear after a short rest. In addition, the presence of pathology at an early stage of its development may be indicated by a crunch in the knee when it is bent. After a short period, all clinical manifestations of patellofemoral arthrosis may disappear.
In the later stages of disease development, the acute phases become longer. In addition to intense pain, signs of swelling of the joint appear. The leg at the knee increases greatly in size. With any movement, the discomfort intensifies. In addition, patients gradually develop gait disturbances, expressed by lameness. With intense damage to the cartilage tissue of the joint, crunching and clicking sounds in the knee appear with any movement.
Subsequently, the clinical manifestations of the disease become intense. The patient loses the ability to move normally without taking painkillers. At the last stage of the pathological process, complete blocking of the joint is observed.
- Femoropatellar arthrosis - symptoms and treatment
Brief information
Patellofemoral arthrosis (lat. Patella - patella) is characterized by damage to the cartilage tissue of the patella and femur.
Usually the diagnosis is made against the background of disruption of the normal structure of cartilage with the slightest physical activity. At the initial diagnosis, no severe signs of pathology are observed. With further progression, this type of arthrosis may manifest unpleasant symptoms. Most often, the disease is detected in young patients leading an active lifestyle, aged 20-40 years. Usually one kneecap is affected, less often – two. There are unfavorable complicating markers that include luxation of the human kneecap (patella), which often occurs in individuals with this type of arthrosis.
Patellofemoral arthrosis - signs
If patellofemoral syndrome is detected, you should not self-medicate. It is necessary to visit a traumatologist to prescribe corrective therapy to slow down the development of pathology. Otherwise, arthrosis will cause a lot of inconvenience in the future. The terminal stage of development of patellofemoral arthrosis often leads to disability.
Diagnostics
If signs of patellofemoral arthrosis appear, the patient should seek advice from such highly specialized specialists as an orthopedist and traumatologist. The specialist first collects anamnesis and assesses the patient’s complaints. During the examination, the doctor assesses the possibility of normal flexion and extension of the joint in a sitting and standing position. In addition, careful palpation of the kneecap is performed with the joint flexed and extended.
Be sure to ask the patient to tense the thigh muscles. In this case, the location of the patella is assessed when attempting to hold it with the fingers. In addition to the location of the cup, during the examination the doctor can preliminarily assess the condition and functionality of the ligaments and muscles. To clarify the nature of the damage, the following instrumental and laboratory tests are prescribed:
- X-ray;
- CT;
- arthroscopy;
- general and biochemical blood tests.
In severe cases, magnetic resonance imaging is often prescribed. MRI can detect even minor disturbances in the structure of the cartilaginous elements of the articulation. After a comprehensive assessment of the condition is completed, the doctor can determine how to treat this pathological condition.
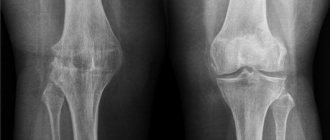
X-ray of the patellofemoral joint
Patellofemoral arthrosis causes a discrepancy between the shape of the patella in relation to the patellar surface of the femur. By examining the pattern of movement of the patella during flexion and extension of the leg, a specialist can narrow down the possible causes of the disease. © Prof. Dr. Sven Ostermeier X-ray of the knee joint in a frontal projection is one of the most important methods for diagnosing joint space in the patellofemoral joint. During this examination, the patient's legs are flexed. Thus, a more accurate distance of the patella to the patellar surface of the femur can be determined. In addition, specialists at the Gelenk-Klinik in Freiburg in Germany perform an X-ray of the knee in a lateral projection: If the image shows a narrowing of the joint space, this indicates gradual wear of the cartilage due to the inflammatory process.
How to treat the disease?
Depending on the degree of neglect of patellofemoral syndrome, therapy can be carried out using both conservative and surgical methods. With a conservative approach to the treatment of this disease, medications are first selected for the patient to suppress inflammation, eliminate symptoms and prevent further destruction of the articular surfaces.
Among other things, the conservative treatment regimen includes physiotherapeutic procedures, exercise therapy, wearing orthoses and special orthopedic shoes, etc. You can use folk remedies to a limited extent.
Medications
To stabilize the condition of the joint with arthrosis, first of all, the patient is selected drugs from among non-steroidal anti-inflammatory drugs. Medicines in this group include:
- Ibuprofen.
- Diclofenac.
- Ketorolac.
- Indomethacin.
- Ketoprofen.
In addition to anti-inflammatory drugs in the form of tablets, patients are prescribed ointments and gels that help eliminate the inflammatory process, improve local blood circulation and help restore the elasticity of damaged ligaments and muscles. Such medications include:
- Diclak gel.
- Voltaren.
- Viprosal.
- Nicoflex.
- Apisatron.
- Finalgel.
For compresses and rubbing of the affected joint, it is recommended to use Dimexide. In the presence of severe pain, intra-articular administration of anesthetics, chondroprotectors and glucocorticosteroids may be indicated. Often, patients with progressive patellofemoral arthrosis are prescribed long courses of tablet forms of chondroprotectors. Such medications include:
- Chondroitin.
- Teraflex.
- Structum.
- Don, etc.
Among other things, multivitamins are often included in the treatment regimen. They help eliminate the deficiency of nutrients in the body and launch regeneration processes.
- Treatment of deforming arthrosis of the knee joint grades 1, 2, 3, its causes and symptoms
Physiotherapy
In the complex conservative treatment of patellofemoral arthrosis, a number of physiotherapeutic procedures are used. Laser therapy is often used for this disease. This procedure involves exposing the affected area of the joint to a special beam of ultraviolet and infrared light. The course of treatment is 5–7 procedures. This physiotherapeutic method of treatment is especially effective in stages 1 and 2 of the pathological process.
In addition, magnetic therapy is often used in the treatment of arthrosis. This physiotherapeutic method can achieve significant improvement in approximately 50% of patients. Dry and liquid cryotherapy is often prescribed for this pathological condition. The liquid version of the procedure is more effective.
To eliminate the discomfort in the knee observed with this disease, paraffin wraps, mud treatment and ozokerite baths are often prescribed. In this case, the therapeutic effect is achieved to a greater extent through dosed exposure to heat.
Also, in the treatment of this pathological condition, electrophoresis with Dimexide, sulfur, zinc, lithium and other substances is often used.
Therapeutic exercises
There are special gymnastics to strengthen the muscles and tendons that support the knee. In the early stages of patellofemoral arthrosis, such exercises can achieve a positive effect even without other conservative methods of therapy. With this knee disease, static exercises give the best effect.
Slowly performed half-squats help develop the knee joints. The pace of the exercise should be as slow as possible. You should do 10–15 squats in one approach. If the patient leads a sedentary lifestyle, he is recommended to perform this exercise every hour.
In addition, gentle stretching may be recommended. To carry it out, you need to stand up straight and lunge forward and backward with each leg in turn. In one approach you should do 20-30 such movements with each leg.
Another effective exercise for developing the knee joint is performed while lying on your back. In this position, you should bend your left leg at the knee, and with your right toe extended, raise it above the surface by 15–20 cm. You should stay in this position for 20–30 seconds, and then change the position of your legs. In one approach you need to do 5 such exercises on each leg. If your condition allows, you need to do 2 approaches with an interval of 5–7 minutes.
Folk remedies
Various folk remedies for the treatment of patellofemoral arthrosis can only be used as auxiliary methods of therapy.
- Osteoarthritis of the knee joint treatment at home
It is advisable to consult a doctor before using various formulations based on herbs and natural ingredients.
A positive effect in this disease can be achieved with daily use of compresses based on iodine, medical bile, ammonia, honey and glycerin. All components must be taken in equal proportions. These ingredients should be mixed thoroughly and placed in a dark place for 2 weeks. Before application, the composition should be slightly warmed up. The compress is applied to the affected joint for 20–30 minutes.
In addition, in the treatment of patellofemoral arthrosis, celandine-based compresses can be used. To prepare the product, you need to take approximately 50–70 g of the succulent leaves and flowers of this plant and grind it to a pulp. The paste should be applied to the knee and covered with gauze. The compress should be kept for 30 minutes. This remedy should be treated for 7 days.
Carrying out the operation
If conservative treatment does not achieve significant improvement, the patient may be prescribed surgical treatment. Arthroscopy is most often prescribed. This procedure involves making a small incision through which a laparoscope equipped with a camera and light source is inserted. This procedure allows you to evaluate the condition of the joint from the inside and, if necessary, replace the affected areas of cartilage with artificial tissue.
Often a lateral incision is made, which involves cutting the ligament in the area of the kneecap. This allows you to normalize the physiological location of the joint. After this, comprehensive rehabilitation is required to restore normal functioning of the joint.
Anatomy of the disorder
The knee joint is what is called a rotating joint. This means that it can bend and turn. The joint consists of three bones, the femur, tibia and patella. Osteoarthritis of the patellofemoral joint of the knee is one of the most common causes of knee pain in middle-aged patients and is often associated with pallotemopherol deficiency.
The patella is a bone that protects the knee, but sometimes stops functioning due to injury or another problem.
The correct diagnosis is made by reviewing the patient's history and physical and radiographic examination of the knee.
Possible causes of the disease
Possible causes of the disease
Patellofemoral arthrosis, or patellofemoral pain syndrome, is a typical disease of the patellar joint (patellofemoral joint). The causes of the disease may also be in the muscles of the back, hip joint or legs.
One of the most common causes is a fracture of the knee joint, which can lead to bone damage. In addition, the cause may be imbalances in the position of the spine and hip joint, which lead to incorrect alignment, which results in overload of the tendon or increased pressure in the knee. The result is a characteristic burning or throbbing pain. There may also be changes in the anatomy of the knee joint itself.
The cause of pain may be retropatellar osteoarthritis (changes in the cartilage in the kneecap), caused by excessive stress that the cartilage cannot withstand. These include, for example, any type of combination of constant overload (especially in knee flexion), misalignment of the leg axes, persistent patellar dislocations or damage to the joint (for example, falling on the knee).
Osteoarthrosis and femoropatellar arthrosis
Osteoarthritis is the chronic degeneration of articular cartilage and the accompanying imbalance between bone accumulation and breakdown. Osteoarthritis is a complex phenomenon involving both physical and metabolic factors.
In a joint, cartilage covers the bone ends and contributes to low joint mobility. Cartilage cells are renewed to the same extent as they are degraded. The joint retains its unrestricted ability to move.
If cell renewal is slower than deterioration and/or physical stress (impact, repeated friction) is too severe, the metabolic balance of the joint is disrupted. Cartilage wear begins with cracks that gradually become deeper until regular craters (ulceration) appear.
Patellofemoral syndrome as a manifestation of patellofemoral osteoarthritis of the knee joint is a disease characteristic of older people, requiring much more serious and long-term treatment. Initially, the first set of drugs is used that improve blood microcirculation, regulate metabolism, reduce blood flow, and slow down cartilage degeneration. The next step is the appointment of physical therapy, including:
- electrophoresis;
- ultrasonic radiation;
- radon and turpentine baths, as well as mud therapy.
Based on the results of the X-ray examination and laboratory tests, the doctor prescribes a set of medications and procedures that may be required for the operation.
Another disease related to patellofemoral syndrome is femoropatellar arthrosis, which most often occurs in athletes. This condition is popularly called “runner's knee”, as athletes’ legs are subject to great stress and injury. It should be noted that female athletes suffer from this type of arthrosis more often than men.
Treatment of femoropatellar arthrosis of the knee joint initially consists of relieving pain symptoms. To do this, apply cold compresses and rub the knee with anti-inflammatory ointments.
It is imperative to stop physical activity and ensure rest. Massaging a sore knee helps a lot.
But we must remember that this disease will never go away on its own. It is necessary to contact an orthopedist, traumatologist, arthrologist. The doctor will examine the knee and prescribe treatment. Diagnosis of this disorder is carried out using x-rays.
Symptoms of patellofemoral syndrome
The cardinal symptom of patellofemoral pain syndrome is pain. The pain may be unilateral, bilateral, or alternating. In the initial stages, the pain may be less and over time it will increase to a large extent as the movement of the knee is not smooth and the muscles become tense during movement. Other pain symptoms:
- Pain in the kneecap area.
- Temporary pain after prolonged strain on the knee joint.
- The pain intensifies after exercise, when climbing stairs, while squatting.
Patients often complain of limited mobility or a typical stretching sensation caused by swelling in the area of the patella.
Partial patellofemoral knee prosthesis
Reasons for implanting a prosthesis
- Isolated arthrosis of the patellofemoral joint.
- Failed conservative treatment.
- Unsuccessful surgical treatment of ligaments.
- Pain and restrictions in daily life.
- Good condition of the meniscus
- Good condition of cruciate ligaments
- Joint stability and range of motion are normal.
The progress of medical technologies in the manufacture of prostheses, as well as modern understanding of how the patellomoral joint is structured, contribute to improved treatment results.
The results of surgery for implantation of a partial patellofemoral prosthesis depend entirely on the quality of the examination, medical indications, as well as on the exact placement of the components. The key to success in this case is experience.
The patient's weight plays an important role in the preservation of the prosthesis: The more a person weighs, the less the retropatellar prosthesis is preserved.
When is a patellofemoral partial denture implanted?
If the articular cartilage and patella are in the stage of destruction or are completely worn out, it no longer makes sense to carry out joint-preserving treatment. However, if the other part of the knee joint—the inner and outer tibiofemoral joints between the femur and the tibia bone—is not damaged, partial patellar replacement is a very good alternative.
Advantages of partial patellofemoral prosthetics
To prevent patellofemoral arthrosis from affecting the main components of the knee joint, timely surgery is necessary. With this intervention, our specialists preserve the natural structure of the knee joint and replace only the damaged area. A timely operation for partial patellofemoral prosthetics prevents complete endoprosthetics for many years.
When is partial patellofemoral prosthetics prohibited?
Contraindications
- Rheumatic inflammations
- Osteoporosis in an advanced stage
- Bacterial infections
- Soft tissue and tendon instability
If arthrosis also affects other parts of the knee joint, an isolated operation to replace the patella no longer makes sense.
In order for the patellofemoral prosthesis to last for many years, there should be no surgery on the knee joint to correct its instability and shape. The longitudinal axis of the knee joint should be straightened. Valgus or varus deformity is undesirable. However, if patients present with such leg pathology, doctors perform an accompanying intervention such as tibial osteotomy to straighten the axis.
For a more precise explanation of the reasons and contraindications for partial patellofemoral prosthetics, the patient should contact experienced specialists.
Total arthroplasty is a good treatment for arthrosis of the knee joint. However, unipolar/partial prosthetics allows you to preserve ligaments and parts of the cartilaginous bone tissue in healthy parts of the knee, and also helps to improve flexion functions.
HEMICAP® Patellofemoral Prosthesis
Over the past years of development of endoprosthetics, the HEMICAP® patellofemoral prosthesis has proven itself well. Implantation of this type of prosthesis is carried out without the use of cement. The back of the prosthesis has a bone-preserving rough structure. A screw is inserted into the tibial spine through a small incision under arthroscope control. Thanks to a special structure similar to the real one, local damage to the cartilage is compensated and the original position of the joint is restored. The strong connection between the surface of the prosthesis and the bones allows patients to exercise without pain.
Lateral x-ray after implantation of a patellofemoral prosthesis.
Implantation of other prostheses involves the use of cement, but the bone anchorage with the HemiCAP® prosthesis ensures long-term stability of the implant without cement mass. Unlike other cemented patellofemoral joint prostheses, implantation of the HemiCAP® prosthesis does not involve separation of the bone substance. Modern medicine offers various types of such prostheses in order to restore the shape of any patella surface of the femur.
The posterior surface of the kneecap is not always covered with a polyethylene implant: If the cartilaginous surface is still intact, it is preserved and used to slide the prosthesis.
If the cartilage structure behind the patella is severely damaged, a polyethylene implant is used to achieve maximum glide. A sliding plastic “liner” made of durable, highly cross-linked polyethylene is inserted on both sides of the patella.
Local arthrosis can be controlled with the HEMICAP patellofemoral prosthesis without the use of cement or the need to separate the femoropatellar joint bone.
This knee replacement allows the original functions of the knee to be preserved. Experienced specialists at our clinic respect the anatomical shape of the knee joint and thus maintain the sliding of the articular surfaces without pain. Often this operation is performed in a minimally invasive form, which shortens the postoperative period and is much easier for patients to tolerate.
Implantation of a cemented patellofemoral prosthesis
During this intervention, the articular surface is freed from the remaining cartilage and then leveled. To strengthen the sliding surfaces, a small particle is carefully separated from the cartilaginous surface. When implanting a patellofemoral prosthesis, the back of the kneecap is covered with a suitable shaped polyethylene “liner”. When replacing a worn-out joint, part of the tibia and femur bone is removed and replaced with a metal component. The components of the patellofemoral prosthesis are fixed with durable bone cement.
Medical request
Diagnosis and treatment
Diagnosis of this disorder is quite simple; it does not require any laboratory tests or hardware diagnostics. The patient lies on his back and completely relaxes his knees, the doctor palpates the kneecap, shifting it alternately in one direction, then in the other direction, identifying the painful point. Pain will also occur when the muscles of the hip joint contract.
Regardless of what the source of pain is, a thorough physical examination should be performed. Additional imaging is necessary to avoid rushed surgical procedures. In particular, before starting any treatment, it is necessary to investigate the possible causes of cartilage damage in order to then begin targeted therapy.
If the pain does not go away after a certain amount of time, grade 2 patellofemoral arthrosis of the knee joint can be diagnosed, which is characterized by the following symptoms:
- Localization of pain. Sharp or nagging pain, which can radiate to the upper thigh, appears in the front of the knee.
- Pain appears after exertion during physical exercise, running, going up or down stairs, squats, lifting weights, and so on. At rest, all pain goes away.
Second-degree patellofemoral arthrosis of the knee can cause the development of the chronic stage of the disease.
Conservative therapy
Special and multi-stage methods of treating this type of disease do not require expensive and rare drugs. Initial therapy should always be conservative. With the help of special relief programs, this disease is in many cases manageable, even if treatment may take a long time. Conservative treatment includes:
- anti-inflammatory drugs.
- exercises to strengthen the quadriceps.
- physical therapy.
- activity modification.
Special bandages can have a positive effect on the condition of the patella. At the beginning of treatment in severe cases, analgesic injections are used.
These measures are complemented by adjustments to daily activities (excluding deep knee flexion), anti-inflammatory medications, strict weight control, and physical therapy.
Prevention and home treatments
The best method for preventing and treating osteoarthritis, as well as for the initial treatment of patellofemoral syndrome, is:
- baths with sea salt and powdered mustard;
- tinctures for rubbing based on chamomile, clover, flaxseed;
- herbal infusions (elderberry, chamomile, hawthorn, celandine, sea buckthorn, arnica);
- a balanced diet, including foods such as vegetables, fruits (especially plums), dairy products, and cereals.
It is recommended to avoid excessive consumption of salt and sugar. And most importantly, the appearance of painful symptoms in the knee should not be ignored by the doctor. Any disease, if it is promptly and correctly diagnosed, can be cured.
Basketball players, dancers, runners - this is an incomplete list of those athletes who are at risk for patellofemoral arthrosis of the knee
The patient may suspect this diagnosis if he has the following symptoms: crunching, clicking in the knee, limping for no apparent reason, swelling in the upper part of the knee, redness, pain. It is pain that is considered a clear sign that a person has patellar arthrosis.
Depending on the intensity of this condition, the following stages of the disease can be distinguished:
- 1st degree. Clinical manifestations are still very small. There is almost no pain. With patellofemoral arthrosis of the 1st degree, a person may experience a feeling of tired legs, especially in the knee area, and a decrease in activity does not give a feeling of restoration of joint tissue.
- 2nd degree. Stage 2 patellofemoral arthrosis of the knee joint is characterized by increased pain. It appears after training, long walking or other stress on the legs. At rest, these sensations disappear.
- 3rd degree. Periodic pain, which now appears much more often, is caused by degenerative changes occurring inside the joint. This can also be seen on an x-ray (narrowing of the space between the bones). Stable motor function with grade 3 patellofemoral arthrosis becomes unavailable.
Patients who have aggravated clinical picture are referred for computed tomography and magnetic resonance imaging. In case of related diseases (psoriasis in the knee area), it would also be useful to refer the patient for a full examination of this area
Treatment of patellofemoral arthrosis of the knee joint is only comprehensive. It should include the following activities.
The patient is prescribed anti-inflammatory drugs (orally and externally) to relieve inflammation and reduce pain syndromes (Diclofenac, Ibuprofen). To stimulate regenerative processes, drugs are prescribed that contain components similar to the soft structures of the joint (Chondroitin, Theraflex). Regular vitamin complexes to strengthen the whole body will also be useful.
They are considered more effective than tablets and ointments. Depending on the desired effect, both anti-inflammatory drugs and chondroprotectors can be used. Hyaluronic acid injections are considered very popular and beneficial for joints. They promote the synthesis of collagen, which is responsible for the elasticity of cartilage.
We are talking about mud therapy, ultraviolet light, electrophoresis, magnetotherapy, balneotherapy and paraffin therapy. They increase local immunity, which is so necessary for recovery. It is necessary to complete a course completely prescribed by a specialist in order to achieve the desired effect.
It should not restrict the foot, and should also be anatomically correct (have a slight rise on the inside - an instep support). Previously, orthopedic shoes could only be purchased in specialized stores. Today, even mass-market manufacturers try to think not only about the beauty of their consumers’ feet, but also about their health, and therefore produce special lines for those who spend a long time on their feet.
For patellofemoral arthrosis of the second degree and higher, surgical intervention may be required
Using the arthroscopy method, you can not only examine the knee area, but also carry out the necessary manipulations to remove areas that have been damaged, and in extreme cases, replace the deformed area. A lateral incision may be required if the patellar ligament needs to be cut. In this way, she is given a normal physiological position.
The knee joint is one of the most mobile in the entire body. A huge amount of bones, ligaments, cartilage and muscles are concentrated here. Impaired functioning of just one area negatively affects the functioning of the entire apparatus - the knee. Treatment of patellofemoral arthrosis of the knee joint must be carried out together with a doctor.
Treatment
You should consult a podiatrist if the following conditions exist:
- History of patellar displacement.
- Direct blow to the knee and suspected patellar fracture or osteochondritis dissecans (long-term pain and/or swelling).
- Repeated subluxation of the patella that is not amenable to physical therapy (one can assume dysplasia of the PF joint).
If central sensitization is present, you should consult a pain management specialist.
Physical therapy
The most common treatments for PFPS are listed below:
- Manual therapy.
- Open and closed kinetic chain exercises.
- Strengthening the quadriceps.
- Patella taping.
- Knee joint orthosis.
- Strengthening the proximal muscles.
- Education.
McConelli knee taping
Which treatment methods are not supported by modern evidence?
- There was no significant difference between open and closed chain exercises based on exercise type.
- More evidence is needed to study the long-term effects of patellar taping, mechanism of action and direction of force (medial, neutral, lateral).
- There is no strong evidence regarding massage, thermotherapy, transcutaneous electrical stimulation, electrical stimulation, or biofeedback training.
What treatments are supported by the best available evidence?
- Tyler et al. noted the significant role of thigh muscle function in the treatment of PFPS. In 93% of cases, treatment was successful in improving hip flexor strength and normalizing the Ober (iliotibial tract/tensor fascia lata) and Thomas (hip flexor) tests.
- Mascal's report documented weakness of the hip abductors, extensors, and external rotators when testing 2 patients with PFPS. Treatment consisted of training the muscles of the thigh, pelvis and trunk, which led to a significant reduction in pain, improvement in the kinematics of the PF joint during dynamic testing; it also had a positive effect on the rate of return to baseline levels of function.
- Whittingham examined the effectiveness of daily patellar taping and exercise on pain and function in individuals with PFPS. The results of his work showed that patellar taping may be useful in combination with strengthening exercises to increase the rate of recovery.
Two articles were reviewed regarding the effect of foot orthoses on PFPS. Both studies show that the use of orthotics in patients with overpronation resulted in decreased pain/stiffness (although these studies used multiple interventions, including orthotics). Patients with patellofemoral pain may benefit from foot orthoses if they have excessive pronation of the foot and/or excessive internal rotation of the lower extremity on weight bearing and an increased Q angle. However, more research is needed to evaluate the effectiveness of such treatment in patients with PFBS.
Quadriceps strengthening
Pain-free exercise is very important in the treatment of PFPS. Isometric exercises with the knee in full extension (the patella not touching the femoral condyles) can be used early in therapy because they minimize stress on the patellofemoral joint while strengthening the quadriceps femoris muscle. Below are two exercises as an example.
Exercise with straight leg.
- The patient is positioned in a supine position, one knee is bent at an angle of 90 degrees (if it is a sore leg, then the exercise should be performed in the absence of pain), the foot is on the support plane; the other leg is fully extended. The patient raises the straightened leg and holds it for 10 seconds. Make sure that the patient maintains normal lumbar lordosis and does not compensate for it with his pelvis.
Pillow compression exercise.
- The patient sits comfortably with back support. Both legs are straight. Place a pillow or rolled-up towel under one knee (this knee may be slightly bent). The patient tries to press the pillow/towel into the table while straightening the knee (quadriceps muscle works).
Open and Closed Kinetic Chain Exercises
Exercises performed in a closed kinetic chain are more functional than exercises in an open kinetic chain. They are characterized by lower load on the PF joint, especially in the terminal ranges of full extension (from 0 to 40 degrees of knee flexion). Therefore, exercises should be performed in this range. Take squats as an example. Make sure that the patient's knees do not extend beyond the line of the toes - as soon as this happens, the load on the PF joint will become too high, which can cause pain.
If the patient cannot tolerate closed chain exercises, then open chain exercises may be a good alternative as it is easier to control the load (as long as the exercises are painless). When using closed chain exercises, the patient should remain within a pain-free range of motion (40 to 90 degrees of knee flexion).
Vastus medialis muscle
Copenhagen ghosts
MSB training is appropriate for some patients with PFPS, but not all. The MSMB assessment should include assessment of engagement, muscle cross-section, endurance, and ability to engage at different angles of knee flexion and be used functionally. Focusing too much on the selective activation of MSMB should be avoided, as there is no evidence that it can be isolated. However, it is extremely important for centering the patella, and therefore, although this muscle is active throughout its entire range of motion, its primary role is flexion from 0 to 30 degrees. The need to improve the function of the intercondylar fossa increases with dysplasia of the intercondylar fossa, high patellar alignment, damage to the medial patellofemoral ligament, or if there is a large gap between the tibial tuberosity and the intercondylar fossa.
Swelling and/or pain are particularly detrimental to MFSB. 10 ml of fluid will inhibit the MFS, but 40 ml will inhibit the vastus lateralis muscle. Similarly, pain causes a delay in the activation of the MFSB, and the greater the pain, the greater the delay. This helps explain why patients following trauma and/or surgery who often have joint effusion develop PFPS. This also explains why resolution of effusion is a primary goal (along with pain reduction).
MFS training should range from 0-30 degrees, include endurance maintenance, and be administered with a tonic component to maintain postural function of the muscle.
A recent study (Benjafield, 2014) shows that exercises targeting the MFSP cause a change in the angle of the MFSB fibers (relative to the femoral axis). The fiber angle can vary from 40 to 70 degrees).
Thigh muscle training
A rehabilitation program for PFPS should also include strengthening exercises for the hip abductors and external rotators. One study found that there was less pain during daily activities and better function when knee exercises were combined with hip exercises.
Another study found that patients with PFPS had worse eccentric hip abduction performance compared with healthy controls. Therefore, it is recommended to use eccentric exercises to strengthen the hip abductors.
Proprioceptive training
View this post on Instagram
Publication from Seminars for doctors and trainers (@physiosapiens.ru)
It has been proven that the quality of proprioception in the knee in patients with PFPS is reduced. Even with unilateral PFPS (i.e., proprioception is reduced in both knees). Therefore, proprioceptive training (in the absence of pain) of the knee joint should be part of the rehabilitation program.
Electrotherapy
Some patients may suffer from PFPS due to a (neuromuscular) imbalance between the vastus medialis and vastus lateralis muscles. The main cause is muscle atrophy of the MFSP and excessive/abnormal lateral displacement of the patella due to a relative increase in the strength of the vastus lateralis muscle. In case of neuromuscular imbalance between the vastus medialis and vastus lateralis muscles, electrical stimulation of the MFJ should be considered as an addition to conservative (physical) therapy, since it is selective and does not lead to an increase in tension on the PF joint.
Foot orthotics
There are several clinical predictors that can determine whether a patient will benefit from a foot orthotic or not.
- Individuals with PFPS who wear less supportive shoes.
- Those who do report lower levels of pain.
- They demonstrate a smaller amplitude of dorsiflexion of the ankle joint.
- Patients who report immediate pain relief with a foot orthosis when performing single-leg squats.
Which orthoses to choose? The studies used prefabricated orthotics made from medium-density ethylene vinyl acetate. They significantly improved functional outcomes in individuals with PFPS after 12 weeks, and these improvements were greater than those observed immediately after orthoses. These improvements may be important for the long-term prevention of knee osteoarthritis in some individuals with PFPS (however, further research is needed).
Video on the topic:
The phrase arthrosis of the patellofemoral joint is used only by traumatologists or surgeons. In the world classification of diseases ICD-10, this disease is called patellofemoral syndrome of the knee joint.
According to WHO, about 13% of all patients who complain of knee pain have pathological changes at the patellofemoral junction.
Usually the disease occurs against the background of other inflammatory processes, but there are cases when the cause may be injury or improper exercise. One of the factors in the development of the disease is old age.
Content
Differential diagnosis
Various diseases can provoke pain in the anterior knee joint without being PFPS:
- Hoff's disease.
- Iliotibial tract syndrome.
- Tendonitis of the patellar tendon.
- Osteoarthritis of the knee joint.
- Damage to articular cartilage.
- Damage to the medial meniscus.
- Baker's cyst.
- Damage to the anterior and posterior cruciate ligaments.
- Referred pain from the hip joint (eg, femoroacetabular impingement, hip osteoarthritis).
- Referred pain from the lumbar region.
Causes of the disease
The onset of patellofemoral arthrosis of the knee joint is provoked by the thinning of the articular cartilage of the patella. Once the function of the cartilage tissue is impaired, disturbances in the motor functions of the knee joint occur. The friction of bones increases, degenerative-dystrophic processes begin. The main link in the pathogenesis of the disease is a violation of the trophic and regenerative capabilities of cartilage.
The cause of this condition may be the following factors:
- genetic abnormalities of connective tissue,
- metabolic diseases,
- hormonal diseases,
- dysplasia and damage to cartilage tissue,
- increased load on the joint,
- obesity stages 3 and 4,
- permanent knee injuries
- inflammatory and autoimmune processes,
- aging and decreased tissue regeneration,
- lack of nutrients and vitamins,
- inflammatory diseases of the skin above the knee.
Sometimes the exact cause cannot be detected, in which case idiopathic arthrosis is diagnosed.
Exercise and Diet
Diet and physical therapy exercises at any stage of arthrosis pathology are an integral part of the treatment program. A severely deformed knee, in order not to provoke increased pain, must be unloaded by reducing body weight. Of course, losing weight applies exclusively to people whose weight exceeds normal values. The patient is recommended nutritional therapy for body weight correction, specially developed by the attending physician. The diet is developed in such a way that the amount of microelements and vitamins received from food satisfies the body's needs, while the extra pounds go away.
Excess weight is unacceptable.
Doctors prohibit the consumption of alcohol, dishes made from fatty meats, various kinds of canned food, fast foods, spicy and smoked foods, sweet carbonated drinks and unhealthy sweets, white baked goods, baked goods, fatty sauces and creams, fried foods. Preference should be given to dishes made from lean meat, cereal products (except rice and semolina), fresh vegetables and fruits, beans, freshly squeezed orange and pomegranate juices, and fermented milk products. The diet should be fractional: you should eat food five times a day in small portions.
Eat a healthy diet.
You must be aware that the diet must be combined with special physical activity. It is important to perform a set of exercises compiled by a specialist under his supervision. The joint, of course, will not recover through exercise therapy at an advanced stage, but you can reduce the effects of degenerative-dystrophic disease on the leg muscles and the musculoskeletal system as a whole. Specifically, the problematic knee joint should not be strained now, since it can be easily injured, which will further aggravate the already difficult quality of life. Therefore, an unskilled approach is not even considered here!
Important! At the third stage, weight loss and therapeutic exercises are mainly necessary as preparation for the upcoming operation. Such preoperative measures, by strengthening the muscular system, will make it easier to endure the rehabilitation period, more quickly restore the lost motor functionality of the operated limb, and achieve better postoperative results.
Symptoms
The clinical picture of arthrosis of the patellofemoral joint of the knee develops very slowly; there are cases of asymptomatic disease.
The disease is latent (hidden) for a long time, and only during the period of exacerbation can the patient develop specific complaints. The first thing the patient notices is a feeling of discomfort when walking or when moving the knee. After a short period of time, increasing pain, clicking and crunching occurs. A characteristic symptom of all arthrosis is morning stiffness, which goes away after half an hour or an hour.
Typically, patellofemoral arthrosis occurs without signs of inflammation, which means that the disease does not lead to an increase in temperature and the development of general intoxication.
The pain is often sharp, intense, localized in the front of the knee, sometimes radiating to the sides, the pain intensifies when the leg is bent at the knee joint.
In advanced stages of the disease, pain can be constant.
Damage to the hamstrings (hamstring syndrome)
Hamstrings are the muscles of the back of the thigh. Sudden movements and changes in direction quite often lead to injury and sprain. It is important to choose the right load so as not to completely tear them, stretching and gradual strengthening with running, sudden stops and changing directions.
Prevention and treatment:
— Strengthening the posterior muscle groups of the thigh in combination with stretching
— Physiotherapy
— Drug treatment
— Manual techniques
Classification
Patellofemoral arthrosis has three stages of the disease. Each degree is characterized by its own clinical features and radiological changes. You need to understand that for each degree, the doctor prescribes different treatment and selects appropriate rehabilitation measures.
As the degree of the disease increases, dystrophic changes in the joint and its fixing apparatus increase.
1st degree
The first or early degree is characterized by the fact that the patient has no specific complaints. Sometimes, while working or standing in one place for a long time, minor discomfort may occur, which goes away after the load stops. Unnoticed by the patient, a gradual decrease in the amplitude of movements occurs. Sometimes in the morning after waking up you may feel a little stiff.
The X-ray picture is practically unchanged; there may be slight thinning of the cartilage and reaction of the periosteum.
2nd degree
Patellofemoral arthrosis of the knee joint of the 2nd degree has severe symptoms with specific radiological and clinical signs. At the beginning of the second stage, frequent discomfort occurs in the knee joint, patella and lateral parts of the patellofemoral joint. There is morning discomfort that lasts more than an hour; when walking or putting pressure on the knees, there is a sharp pain that does not allow you to continue moving. Pain reduces the functionality of the knee joint. The x-ray clearly shows a narrowing of the space between the patella and the femur, thinning of the cartilage and the appearance of a small number of osteophytes.
3rd degree
The third or terminal degree is characterized by the fact that cartilage tissue almost disappears and bone friction occurs. The patient cannot walk normally, the pain occurs even at rest and does not go away after stopping the load. Severe pain is localized near the patella and on its lateral surfaces. Morning stiffness can last for about several hours. The X-ray shows a complete absence of space between the patella and the thigh. The images show a large number of osteophytes. There is a complete change in the patellofemoral articulation. Treatment is usually symptomatic and surgical.
Runner's knee (patellofemoral pain syndrome)
This often happens when the patella becomes dislocated from where it is centered. In this case, very often the cartilage wears out, which causes pain around the patella. Especially when you go up and down stairs, squat, or sit for long periods of time with your knees bent.
Prevention and treatment:
⁃ Properly selected physical activity (exercises)
⁃ Taping with patellar centering
⁃ Correctly selected shoes
⁃ PRP therapy and hyaluronic acid preparations (only as prescribed by a doctor!)
Diagnostics
Before prescribing radiation methods, the doctor must conduct an objective examination of the patient, examine the skin near the affected joint, and check the functions of flexion and extension.
It is also necessary to collect anamnesis and ask the patient about the possible reasons why arthrosis could develop. After the examination, it is necessary to analyze the patient’s complaints and assume the stage of the disease. Sometimes at the initial stage many diagnostic errors occur, since the symptoms may be sluggish, or the patient does not attach due importance to some little things.
After examination and questioning, the doctor chooses a radiological diagnostic method, usually:
- radiography in standard projections,
- computed tomography (CT),
- magnetic resonance imaging (MRI).
To complete the picture, paraclinical studies are prescribed, which include:
- general blood analysis,
- general urine analysis,
- blood biochemistry,
- COE,
- C-reactive protein.
After analyzing all the data, you can establish an accurate diagnosis and prescribe the correct treatment.
Diagnosis of pathology
If a patient experiences alarming signs that may suggest the development of a dystrophic-degenerative condition, it is necessary to seek help from an orthopedic traumatologist as soon as possible. The doctor must conduct an initial examination and refer the patient for tests and x-rays. If during X-rays a questionable picture is observed in the diagnosis of the disease, you can send the patient for further examination, for example the following types of instrumental studies:
- MRI or ultrasound if there are signs of soft tissue damage or suspicion of arthritis. According to indications, a study of the sacral joint may be prescribed for the differential detection of ankylosing spondylitis in the initial stages.
- CT. This method allows you to see pathological changes in joints and cartilage until they become visible on an x-ray. Computed tomography allows you to identify adverse pathological changes in the joints before the onset of the clinical picture of the disease.
- Arthroscopy is the most accurate diagnostic method. With the help of the study, you can detect all possible pathological changes in the joints at any stage of the disease.
X-rays allow us to examine the signs of the disease at stages 2 and 3 of development, when discomfort, a feeling of stiffness and crunching in the knees have already occurred. There is a narrowing of the joint space, signs of inflammation and deformation in the cartilage plate.
To differentiate the pathology from other similar conditions (various types of arthritis), a number of laboratory tests are required, including:
- Biochemical blood test with kidney samples.
- Rheumatoid factor.
- Complete blood count with determination of ESR.
- C-reactive protein.
- General urine analysis.
Carrying out these tests allows us to exclude other serious pathologies, such as reactive or rheumatoid arthritis, gout.
Treatment methods
In the treatment of patellofemoral arthrosis of the knee joint, new combinations of therapeutic drugs from various pharmacological groups should be used. To achieve the maximum therapeutic effect, it is necessary to eliminate the causes that may provoke an exacerbation of the disease.
Therapy is of the following types:
- conservative,
- surgical,
- physiotherapeutic,
- Exercise therapy exercises to restore the patellofemoral joint.
Drug treatment of the patellofemoral joint of the knee joint includes taking the following drugs:
- NSAIDs (in injections and tablets),
- chondroprotectors,
- painkillers,
- vitamin preparations,
- hormonal drugs (if urgently needed).
Before starting treatment for a pathology, first consult with your doctor.
For advanced second or third stages of the disease, surgical treatment is used.
The following intervention options are used:
- Arthroscopy using special endoscopes. A good way to diagnose and remove dystrophic changes. Also, using this technique, you can inject medicinal drugs into the joint cavity and pump out joint fluid.
- Side release. This method is aimed at correcting the position of the kneecap. Using surgical instruments, the external ligaments are cut and the position of the patella is restored.
Physiotherapeutic treatment methods are aimed at eliminating pathology in the patellofemoral joint. During the procedures, the processes of blood circulation and metabolism in cartilage tissue improve.
The most common methods:
- mud baths,
- magnetotherapy measures,
- electrophoresis with anti-inflammatory ointments,
- paraffin therapy,
- acupuncture,
- water procedures.
Physiotherapy is an additional treatment method and is prescribed only after a complete examination.