Orthopedic traumatologist > Articles > Mosaic chondroplasty of the knee joint
Articular cartilage of any joint, including the knee, has an extremely low self-healing potential. Deep cartilage defects are highly likely to lead to osteoarthritis. The frequency of such defects is about 5% in the overall structure of injuries to the knee joint.
Local traumatic injury of the knee joint, view through an arthroscope.
Treatment of local chondral defects still remains a complex and controversial problem in orthopedics. Many years of efforts by doctors and researchers are aimed at finding an optimal solution that would allow the restoration of “worn out” hyaline cartilage in the area of maximum load.
In the early 60s, the technology of drilling subchondral holes was proposed to stimulate the growth of stem cells, which, it seemed, would ensure cartilage regeneration. This technique became quite widespread in the 90s and was called “microfracture.” It has found its use in a fairly limited group of patients - young people with small and “fresh” cartilage damage.
In 1983, M. Brittberg and L. Peterson began using autologous cultured chondrocytes to treat cartilage damage. The essence of this method is to obtain and cultivate the patient's chondrocytes, and then transplant them onto a periosteal flap. The results of this technology are quite satisfactory, but the method itself is technically quite complex. Currently, matrix implantation of autologous chondrocytes using the arthroscopic method is more often used.
In the 90s of the last century, various techniques of osteochondral transpallantations were also proposed and actively used. This term refers to the transplantation of osteochondral fragments from one area of the joint to another, where there is an area of destroyed cartilage.
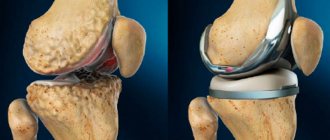
Schematic representation of mosaic plastic.
Historical aspects of mosaic plastic surgery of the knee joint
First, procedures were developed for transplanting large osteochondral grafts obtained from the patella, the medial and lateral surfaces of the condyles, and the intercondylar groove. These methods were too invasive and did not allow obtaining sufficiently congruent grafts, and also often led to disruption of the biomechanics of the joint.
Therefore, it has been proposed to use multiple cylindrical osteochondral grafts. Successful surgery using this technique was demonstrated by Matsusue et al. in 1993. During the operation, a 15 mm defect in the femoral condyle, caused by a rupture of the anterior cruciate ligament, was successfully closed. This technique is called mosaic cartilage plastic surgery (“Mosaicplasy”).
Mosaic plastic surgery - questions on biomechanics and histology
There are several questions regarding mosaic plastic surgery of the knee joint:
What is the minimum size of a cartilage defect that can be closed with mosaicplasty?
Studies on cadavers show that the maximum pressure at the periphery of the defect is observed when its size is more than 10 mm. Therefore, this threshold value is used to determine indications for surgery.
Does mosaicplasty reduce the load on cartilage?
It was found that destruction of cartilage over an area of 16 mm (about 2 cm2) leads to an increase in peripheral tension by 92%, which further increases the destruction of cartilage and contributes to increased pain. When three 8-mm grafts are transplanted, peripheral tension increases by only 35%
Where is the best place to get transplants?
The optimal location for the fence is the areas with the least load, sufficient thickness and curvature of the surface similar to the recipient area.
Studies have shown that the lateral and lateral surfaces of the femoral condyles experience the least load in the knee joint. It is from these areas that transplants are taken.
Does the curvature of the grafts matter?
Restoring the curvature of the joint as close as possible to the original one is very important for even distribution of the load. Therefore, it is very important to select the curvature of the grafts.
Is the thickness of the cartilage on the donor fragment important?
The thickness of cartilage directly depends on the load and varies in different parts of the joint. Naturally, in donor areas the cartilage is somewhat thinner (on average 1.8 mm), and in areas requiring restoration it is thicker - up to 2.5 mm. However, this difference does not cause big problems.
Arthroscopy or arthrotomy - which is better when harvesting a transplant?
In a study by Keeling et al. it was shown that grafts obtained by arthroscopy had a discrepancy of up to 1 mm in 69% of cases, and by arthrotomy - in 57%. It was noted that arthroscopy is more difficult when harvesting the graft from the lateral surface of the condyles, and it also increases the risk of marginal fractures.
What determines the stability of the graft?
Animal studies have established the following facts:
- grafts with a diameter of 11 mm and a length of 15 and 20 mm have better vertical stability;
- ideal adjustment of the graft length to the depth of the “planting socket” ensures a 2-3 times increase in stability;
- grafts with press-fit fixation are more stable (this effect is achieved due to the fact that the transplanted osteochondral fragment itself is slightly wider than the hole for implantation).
What happens if the curvature of the graft does not match the curvature of the area being restored?
In a study on sheep, it was shown that a curvature mismatch of up to 1 mm is acceptable and the cartilage is preserved; if the discrepancy reaches 2 mm or more, then aseptic necrosis of the graft occurs and it gradually resolves.
Does the viability of graft cartilage depend on the force during its fixation?
When the pressure force during fixation is up to 10 MPa, the chondrocytes do not suffer, but if pressure is applied with a force above 15 MPa, cartilage damage occurs. Therefore, it is recommended to insert the graft with several gentle pressures rather than intense ones.
DEGREES OF DAMAGE TO ARTICULAR CARTILAGE.
Normally, the thickness of articular cartilage is 1-6 mm; the processes of formation and destruction of cartilage are in balance and are regulated by the level of loads. With the development of osteoarthritis, this balance is gradually disrupted, destructive processes begin to prevail, which leads to disruption of the structure and mechanical properties of cartilage. Gradually, the cartilage becomes thinner, becomes looser, and cracks and cartilage defects form. In parallel, pathological changes occur in other articular structures of the joint, synovial fluid, joint capsule, subchondral bone. Depending on the degree and depth of cartilage damage, several stages of damage are distinguished. I degree - softening, loosening, decreasing the elasticity of the surface layer of cartilage. II degree - thinning, disintegration of the surface layer of cartilage, formation of cracks, erosions that do not reach the deep parts of the cartilage and subchondral bone. III degree - thinning, disintegration of the cartilage with the formation of deep cracks, defects and erosions reaching the deep parts of the cartilage and subchondral bone, the formation of zones of sclerosis of the subchondral bone, the appearance of osteophytes (pathological growths of bone tissue). IV degree - full-thickness cartilage defects with exposure of subchondral bone, the presence of bone deformation.
What happens to the donor site?
Control arthroscopy showed that the donor site remains empty, only after a sufficiently long time does it slightly lower and fibrous tissue forms in the depths.
Experiments have been conducted with filling the defect with an osteoperiosteal plug from the tibia, but this still does not provide bone filling.
Briefly summarizing all of the above, we can draw the following conclusions:
- osteochondral grafts from the lateral and medial surfaces of the condyles, as well as from the area of the intercondylar groove, can successfully correct cartilaginous defects;
- the diameter of the graft should be slightly larger than the landing hole;
- the length of the graft should be equal to the depth of the hole;
- Press-fit method is preferred;
- The osteochondral implant remains viable for a long time and ensures normal functioning of the joint.
Advantages and disadvantages of using osteochondral grafts
A short list of advantages:
- the osteochondral graft used for mosaic chondroplasty is a completely viable functional unit that allows the restoration of destroyed hyaline cartilage;
- the size of the graft can be easily adjusted to the size of the planting area;
- the procedure is one-stage in nature - no intermediate steps are required in the form of growing cells in the laboratory;
- low risk of complications.
Flaws:
- difficulty in choosing areas with the necessary curvature to ensure better congruence;
- When taking a large number of donor grafts, the risk of postoperative joint pain is high.
Who is indicated for mosaic chondroplasty of the knee joint?
This type of surgery is preferably performed in patients with focal destruction of articular cartilage in areas of greatest stress. This usually happens as a result of direct traumatic effects and osteochondritis. Local damage can be assumed clinically - based on pain that intensifies in a certain position of the joint.
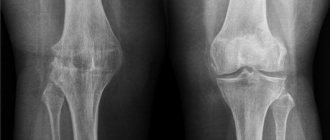
The patient must undergo an X-ray of the knee. It is advisable to conduct CT and MRI of the knee joint. At the same time, CT has greater specificity and makes it possible to identify superficial cartilage defects, while MRI is more suitable for assessing the degree of osteochondritis and for selecting donor sites.
MECHANISMS OF OSTEOARTHROSIS DEVELOPMENT, RISK FACTORS.
Osteoarthritis can be either primary (idiopathic), without a clearly defined cause, or secondary, developing as a result of a specific injury or disease. Risk factors for the development of arthrosis may be joint injuries, age-related changes, movement disorders, excess body weight, uneven distribution of loads caused by congenital or acquired deformation of the musculoskeletal system, genetic factors, inflammatory, metabolic, rheumatic diseases, etc. Typical symptoms of arthrosis are pain during exercise and movement, increased pain towards the end of the day, stiffness of the joints after a period of immobility, morning stiffness, cracking in the joints. As the process progresses, there is a gradual increase in pain, the appearance of pain at rest, limited joint mobility, swelling and deformation in the joint area, narrowing of the joint space, the formation of cartilage defects and bone growths. Also, one of the components of the development of osteoarthritis is a violation of the normal composition and visco-elastic properties of synovial fluid, which plays an important role in the “nutrition and lubrication” of articular cartilage.
Mosaic chondroplasty technique
The patient's position is on the back with the leg bent at 120°. An x-ray with a reference mark helps ensure that the knee is flexed enough to access the bone donor site.
Next, arthroscopic access is made to the femoral condyle with the damaged area of cartilage. The area is cleaned with a curette and the edges are excised to obtain a smooth, healthy contour. Then a probe with marks is inserted - it is used to measure the exact size of the defect. If the defect is too large or located very far away, the operation is performed using arthrotomy (open approach).
The next step is to make a tissue incision and gain access to the area of the bone from which the graft will be taken. The cross principle is used: if a defect is restored on the medial condyle, then the graft is taken from the lateral surface of the lateral one and vice versa. The tissue is taken with a tubular chisel. It is very important to maintain exact perpendicularity with respect to the surface of the cartilage at the moment of “driving in” the chisel.
The number of cylindrical osteochondral fragments harvested varies from three to five and depends on their size: the larger the graft, the fewer are required. Usually 3 grafts with a diameter of 10-11 mm or 5-6 with a diameter of 5-7 mm are taken.
After obtaining the required number of osteochondral fragments, the first “landing socket” is drilled on the defective area of the cartilage. This is also done with a tubular chisel, but its diameter is 1 mm smaller than that used to extract grafts. The length of the landing hole is measured, the length of the graft is adjusted to it, which is carefully fixed to the place intended for it using the press-fit method. The procedure is repeated the required number of times. In this case, the holes are drilled in such a way that they are not parallel and fan out from the hypothetical center of curvature of the condyle, this allows the curvature of the articular surface to be restored as accurately as possible.
Anatomy of the shoulder joint
home
Treatment
Shoulder arthroscopy
Anatomy of the shoulder joint
The shoulder joint is formed by the glenoid cavity of the scapula and the head of the humerus. The articular surfaces are covered with hyaline cartilage and their sizes do not correspond to each other. The area of the head is three times the area of the scapula. The congruence of the articular surfaces is increased by the articular labrum, which is located along the edge of the glenoid cavity.
The articular capsule is fixed on the scapula along the edge of the articular cartilage of the glenoid cavity and along the outer edge of the articular labrum; On the humerus, the articular capsule is attached along the anatomical neck. The joint capsule is spacious and weakly stretched. In the lower part it is thin, and throughout the rest of the length it is reinforced by the muscle tendons (supraspinatus, infraspinatus, subscapularis and teres minor muscles) interwoven into it. When moving in the shoulder joint, these muscles pull back the articular capsule and prevent it from being pinched between the articular surfaces of the bones.
The articular capsule on the humerus in the form of a bridge spreads over the intertubercular groove, where the tendon of the long head of the biceps brachii muscle lies, which starts from the supraglenoid tubercle and the edge of the articular labrum, passes through the cavity of the shoulder joint and then runs in the intertubercular groove. In the cavity of the shoulder joint, the tendon of the biceps brachii muscle is covered with a synovial membrane, which accompanies it in the intertubercular groove 2-5 cm below the level of the anatomical neck, then wraps upward and, following along the tendon, passes into the synovial membrane of the articular capsule.
There are three glenohumeral ligaments located on the inner surface of the joint capsule. They are attached on one side to the anatomical neck of the humerus, on the other - to the articular lip of the scapula. The superior and middle ligaments are separated by the openings of the bursa located under the subscapularis muscle. Ligaments strengthen the anterior surface of the shoulder joint capsule.
In addition, the shoulder joint has a powerful coracobrachial ligament. It is a compaction of the fibrous layer of the capsule that extends from the outer edge of the coracoid process to the greater tubercle of the humerus.
The coracoacromial ligament is located above the shoulder joint and, together with the acromion and coracoid process of the scapula, forms the arch of the shoulder. The arch of the shoulder protects the shoulder joint from above and, together with the tension of the joint capsule, inhibits abduction of the shoulder and raising the arm anteriorly or to the side above shoulder level. Further upward movement of the limb occurs due to the movement of the scapula along with it.
The shoulder joint is triaxial, shaped like a ball-and-socket joint. Due to the fact that the shoulder joint is the most mobile joint in the human body, the arm has significant freedom of movement.
Mosaic chondroplasty of the patella and tibial articular surface
As we know, the knee joint has two more articular surfaces - the inner side of the patella and the articular surface of the tibia. They can also become damaged and require “repair”.
In the case of the patella, mosaic chondroplasty is not difficult. It is always performed in an open manner, as it requires dislocation of the patella. The source of grafts is usually the intercondylar groove, and the osteochondral fragments themselves are thinner - no more than 12 mm (for operations on the femoral epicondyles, their length is 15-18).
Carrying out mosaic chondroplasty of the articular surface of the tibia of the knee joint is technically quite difficult. This requires a guide ligamentoplasty of the anterior cruciate ligament - this provides access to the operation site. The sources of transplants are still the same.
Postoperative period and rehabilitation
In the early postoperative period, ice packs are applied knee The use of anticoagulants is also undesirable, as they increase the risk of hemarthrosis.
The joint can be loaded the very next day if plastic surgery was performed with one graft, but only with a limited amount of flexion. Otherwise, it is recommended to completely eliminate the load on the joint for up to 3 weeks, and then gradually increase it over 3-4 weeks. After 10 weeks the patient is allowed to run.
NON-DRUG TREATMENT OF OSTEOARTHROSIS.
Treatment of osteoarthritis should be comprehensive, including both drug and non-drug treatment. Of great importance in non-drug treatment is the correct motor regimen and regular exercise therapy (PT). Joints vitally need movement. Moreover, the main load during exercise therapy should be aimed at cyclic movements in the joints and strengthening the muscles of the limb, without significant axial load on the affected joints. These can be simple exercises performed at home - walking, swimming, repeated straight leg raises, in a lying position, flexion-extension of the knee joint, raising on toes... or more specialized exercises on exercise machines and with an instructor. In this case, pronounced axial loads on the joints, heavy lifting, running, jumping, and uncoordinated movements should be avoided. It is also very important to reduce the load on the joints by reducing excess weight. Properly organized nutrition should also contribute to weight correction and improvement of metabolism. In addition, it is necessary to use comfortable shoes, as well as various means of orthopedic correction - instep supports, knee pads, orthoses, and, if necessary, additional support. Quite often, physiotherapy is used in the complex treatment of osteoarthritis. This could be an elector or phonophoresis with hydrocortisone (or other drugs), magnetic therapy, alternating electromagnetic fields, laser therapy, cryotherapy, shock wave therapy, etc. The choice of physiotherapy method is made by a doctor, taking into account the indications and contraindications for this type of treatment. Non-drug treatment also includes massage, reflexology, spa treatment, and various types of traditional medicine.