Articular cartilage of any joint, including the knee, has an extremely low self-healing potential. Deep cartilage defects are highly likely to lead to osteoarthritis. The frequency of such defects is about 5% in the overall structure of injuries to the knee joint.
Local traumatic injury of the knee joint, view through an arthroscope.
Treatment of local chondral defects still remains a complex and controversial problem in orthopedics. Many years of efforts by doctors and researchers are aimed at finding an optimal solution that would allow the restoration of “worn out” hyaline cartilage in the area of maximum load.
In the early 60s, the technology of drilling subchondral holes was proposed to stimulate the growth of stem cells, which, it seemed, would ensure cartilage regeneration. This technique became quite widespread in the 90s and was called “microfracture.” It has found its use in a fairly limited group of patients - young people with small and “fresh” cartilage damage.
In 1983, M. Brittberg and L. Peterson began using autologous cultured chondrocytes to treat cartilage damage. The essence of this method is to obtain and cultivate the patient's chondrocytes, and then transplant them onto a periosteal flap. The results of this technology are quite satisfactory, but the method itself is technically quite complex. Currently, matrix implantation of autologous chondrocytes using the arthroscopic method is more often used.
In the 90s of the last century, various techniques of osteochondral transpallantations were also proposed and actively used. This term refers to the transplantation of osteochondral fragments from one area of the joint to another, where there is an area of destroyed cartilage.
Schematic representation of mosaic plastic.
Historical aspects of mosaic plastic surgery of the knee joint
First, procedures were developed for transplanting large osteochondral grafts obtained from the patella, the medial and lateral surfaces of the condyles, and the intercondylar groove. These methods were too invasive and did not allow obtaining sufficiently congruent grafts, and also often led to disruption of the biomechanics of the joint.
Therefore, it has been proposed to use multiple cylindrical osteochondral grafts. Successful surgery using this technique was demonstrated by Matsusue et al. in 1993. During the operation, a 15 mm defect in the femoral condyle, caused by a rupture of the anterior cruciate ligament, was successfully closed. This technique is called mosaic cartilage plastic surgery (“Mosaicplasy”).
Mosaic plastic surgery - questions on biomechanics and histology
There are several questions regarding mosaic plastic surgery of the knee joint:
What is the minimum size of a cartilage defect that can be closed with mosaicplasty?
Studies on cadavers show that the maximum pressure at the periphery of the defect is observed when its size is more than 10 mm. Therefore, this threshold value is used to determine indications for surgery.
Does mosaicplasty reduce the load on cartilage?
It was found that destruction of cartilage over an area of 16 mm (about 2 cm2) leads to an increase in peripheral tension by 92%, which further increases the destruction of cartilage and contributes to increased pain. When three 8-mm grafts are transplanted, peripheral tension increases by only 35%
Where is the best place to get transplants?
The optimal location for the fence is the areas with the least load, sufficient thickness and curvature of the surface similar to the recipient area.
Studies have shown that the lateral and lateral surfaces of the femoral condyles experience the least load in the knee joint. It is from these areas that transplants are taken.
Does the curvature of the grafts matter?
Restoring the curvature of the joint as close as possible to the original one is very important for even distribution of the load. Therefore, it is very important to select the curvature of the grafts.
Is the thickness of the cartilage on the donor fragment important?
The thickness of cartilage directly depends on the load and varies in different parts of the joint. Naturally, in donor areas the cartilage is somewhat thinner (on average 1.8 mm), and in areas requiring restoration it is thicker - up to 2.5 mm. However, this difference does not cause big problems.
Arthroscopy or arthrotomy - which is better when harvesting a transplant?
In a study by Keeling et al. it was shown that grafts obtained by arthroscopy had a discrepancy of up to 1 mm in 69% of cases, and by arthrotomy - in 57%. It was noted that arthroscopy is more difficult when harvesting the graft from the lateral surface of the condyles, and it also increases the risk of marginal fractures.
What determines the stability of the graft?
Animal studies have established the following facts:
- grafts with a diameter of 11 mm and a length of 15 and 20 mm have better vertical stability;
- ideal adjustment of the graft length to the depth of the “planting socket” ensures a 2-3 times increase in stability;
- grafts with press-fit fixation are more stable (this effect is achieved due to the fact that the transplanted osteochondral fragment itself is slightly wider than the hole for implantation).
What happens if the curvature of the graft does not match the curvature of the area being restored?
In a study on sheep, it was shown that a curvature mismatch of up to 1 mm is acceptable and the cartilage is preserved; if the discrepancy reaches 2 mm or more, then aseptic necrosis of the graft occurs and it gradually resolves.
Does the viability of graft cartilage depend on the force during its fixation?
When the pressure force during fixation is up to 10 MPa, the chondrocytes do not suffer, but if pressure is applied with a force above 15 MPa, cartilage damage occurs. Therefore, it is recommended to insert the graft with several gentle pressures rather than intense ones.
Indications for ankle arthroscopy
Arthroscopy of the ankle joint for a fracture of the talus.
Most often, ankle arthroscopy is performed for the following indications:
Osteochondritis dissecans
This is an aseptic disease characterized by necrotization of parts of cartilage and bone over time, with further separation of necrotic areas and the formation of free chondral bodies. The disease occurs in young people. During arthroscopy, necrotic tissue is removed, viable areas of cartilage are fixed, foci of inflammation are eliminated, and the articular surface is sanitized (debridement).
Impingement syndrome
This is the name given to the collision of the bone structures of the joint. There are anterior and posterior ankle impingement syndrome, each of which has its own characteristics. In both cases, the edge of the tibia collides with the talus, pinching the articular capsule and synovial membrane occurs, which is accompanied by pain symptoms and limitation of movements up to blockade. The anterior one is most common among professional athletes, who often intensively extend the foot (basketball players, football players), and is a consequence of injuries, mainly of the ligamentous apparatus, the posterior one - among ballet dancers.
Ostrigonum may be a predisposition to posterior impingement—in some people, the talus tuberosity may be a separate bone. Impingement is accompanied by periodic inflammation, which subsequently leads to the formation of bone growths (osteophytes), connective tissue scar structures, and adhesions. Osteophytes and other pathologically altered tissues and pathological adhesions are removed arthroscopically. The function of the joint is usually restored completely.
Damage to cartilage tissue
They may be of traumatic or degenerative etiology, single or multiple, with or without complete separation of parts of the cartilage. Treatment tactics are selected for each patient individually depending on the timing, causes, features, and distribution of cartilage deformations. The possibility of restoring its integrity and fixing the separated fragment, restoring a smooth surface (abrasive chondroplasty, debridement) is being assessed.
Chronic synovitis of the ankle joint
A fairly common pathology, caused by many factors, in which the pain syndrome is of a constant aching nature, some swelling and limited mobility may be observed. Synovitis (inflammation of the synovial membrane of the joint) with persistent recurrence is treated surgically. Arthroscopically, complete or partial removal of the membrane is performed (synovectomy). Subsequently, such patients are indicated for observation and comprehensive treatment to avoid complications.
What happens to the donor site?
Control arthroscopy showed that the donor site remains empty, only after a sufficiently long time does it slightly lower and fibrous tissue forms in the depths.
Experiments have been conducted with filling the defect with an osteoperiosteal plug from the tibia, but this still does not provide bone filling.
Briefly summarizing all of the above, we can draw the following conclusions:
- osteochondral grafts from the lateral and medial surfaces of the condyles, as well as from the area of the intercondylar groove, can successfully correct cartilaginous defects;
- the diameter of the graft should be slightly larger than the landing hole;
- the length of the graft should be equal to the depth of the hole;
- Press-fit method is preferred;
- The osteochondral implant remains viable for a long time and ensures normal functioning of the joint.
Contraindications
- Irreversible destruction of the joint, severe deformation of the bones of the foot, which does not allow the correct installation of the endoprosthesis.
- Acute inflammatory diseases (infectious and aseptic) in the area of the planned operation (in bones, soft tissues, on the skin).
- Osteoporosis (sparse bone tissue) in the lower legs.
- Significant disturbances in the blood supply and innervation of the operated limb.
- Long-term hormone therapy on the eve of surgery.
- Acute infectious diseases in the recent past.
- State of immunodeficiency.
- Decompensated somatic diseases (heart failure, diabetes mellitus, etc.)
- Childhood (due to the continued growth of the child).
Advantages and disadvantages of using osteochondral grafts
A short list of advantages:
- the osteochondral graft used for mosaic chondroplasty is a completely viable functional unit that allows the restoration of destroyed hyaline cartilage;
- the size of the graft can be easily adjusted to the size of the planting area;
- the procedure is one-stage in nature - no intermediate steps are required in the form of growing cells in the laboratory;
- low risk of complications.
Flaws:
- difficulty in choosing areas with the necessary curvature to ensure better congruence;
- When taking a large number of donor grafts, the risk of postoperative joint pain is high.
Who is indicated for mosaic chondroplasty of the knee joint?
This type of surgery is preferably performed in patients with focal destruction of articular cartilage in areas of greatest stress. This usually happens as a result of direct traumatic effects and osteochondritis. Local damage can be assumed clinically - based on pain that intensifies in a certain position of the joint.
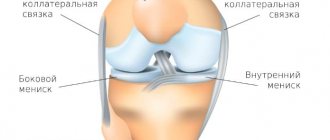
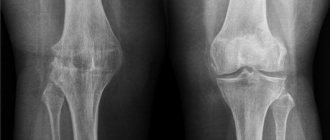
The patient must undergo an X-ray of the knee. It is advisable to conduct CT and MRI of the knee joint. At the same time, CT has greater specificity and makes it possible to identify superficial cartilage defects, while MRI is more suitable for assessing the degree of osteochondritis and for selecting donor sites.
Consultation with an orthopedist-traumatologist
First of all, an in-person consultation with an orthopedist-traumatologist is necessary.
Only an experienced traumatologist specializing in the treatment of foot and ankle pathologies can correctly assess its condition and the possibilities of treatment - conservative or surgical, and determine the need and possibility of endoprosthetics. To do this, you need to conduct an x-ray of the joint in 2 projections and a computed tomography of the ankle joint. If a decision is made to replace a joint, the patient undergoes a preoperative examination (laboratory - blood and urine tests; ECG, fluorography, consultations with related specialists - dentist, urologist/gynecologist, therapist), and the doctor plans the operation.
To make an appointment with a doctor
Mosaic chondroplasty technique
The patient's position is on the back with the leg bent at 120°. An x-ray with a reference mark helps ensure that the knee is flexed enough to access the bone donor site.
Next, arthroscopic access is made to the femoral condyle with the damaged area of cartilage. The area is cleaned with a curette and the edges are excised to obtain a smooth, healthy contour. Then a probe with marks is inserted - it is used to measure the exact size of the defect. If the defect is too large or located very far away, the operation is performed using arthrotomy (open approach).
The next step is to make a tissue incision and gain access to the area of the bone from which the graft will be taken. The cross principle is used: if a defect is restored on the medial condyle, then the graft is taken from the lateral surface of the lateral one and vice versa. The tissue is taken with a tubular chisel. It is very important to maintain exact perpendicularity with respect to the surface of the cartilage at the moment of “driving in” the chisel.
The number of cylindrical osteochondral fragments harvested varies from three to five and depends on their size: the larger the graft, the fewer are required. Usually 3 grafts with a diameter of 10-11 mm or 5-6 with a diameter of 5-7 mm are taken.
After obtaining the required number of osteochondral fragments, the first “landing socket” is drilled on the defective area of the cartilage. This is also done with a tubular chisel, but its diameter is 1 mm smaller than that used to extract grafts. The length of the landing hole is measured, the length of the graft is adjusted to it, which is carefully fixed to the place intended for it using the press-fit method. The procedure is repeated the required number of times. In this case, the holes are drilled in such a way that they are not parallel and fan out from the hypothetical center of curvature of the condyle, this allows the curvature of the articular surface to be restored as accurately as possible.
How is the operation performed?
The operation is performed under epidural anesthesia. An injection is made in the spine, which “turns off” the sensitivity of the body below the belt for the duration of the operation.
- Having cut the soft tissue, the surgeon carefully moves aside the nerves, vessels and ligaments, without crossing them, but providing access to the joint.
- Next, the doctor removes the joint capsule, scar tissue and very sparingly excises the deformed areas of the tibia and talus bones that form the ankle joint.
- Then all the components of the artificial joint are installed in the prepared bed, including a polymer liner that serves as a gasket between the metal parts.
- The endoprosthesis is installed using the press-fit method (tight fit into the bone). The implant has a special coating that facilitates its ingrowth into bone tissue. This allows the endoprosthesis to be firmly fixed in the bone.
- The surgeon then sutures the soft tissue.
After the operation, an x-ray is taken to verify the correct installation of the prosthesis.
At the end of the operation, the joint is fixed with an orthosis. The patient is transferred to the hospital inpatient unit.
Mosaic chondroplasty of the patella and tibial articular surface
As we know, the knee joint has two more articular surfaces - the inner side of the patella and the articular surface of the tibia. They can also become damaged and require “repair”.
In the case of the patella, mosaic chondroplasty is not difficult. It is always performed in an open manner, as it requires dislocation of the patella. The source of grafts is usually the intercondylar groove, and the osteochondral fragments themselves are thinner - no more than 12 mm (for operations on the femoral epicondyles, their length is 15-18).
Carrying out mosaic chondroplasty of the articular surface of the tibia of the knee joint is technically quite difficult. This requires a guide ligamentoplasty of the anterior cruciate ligament - this provides access to the operation site. The sources of transplants are still the same.
Abrasive chondroplasty
All methods from the first group of the list are based on one principle: with a special awl or drill, holes are made in the cartilage through which mesenchymal stem cells, the ancestors of connective tissue cells, enter the defect area. The body tries to close these defects - and in their place, after a few months, fibrous cartilage appears.
abrasive chondroplasty technique has been used for a long time, but there is a significant drawback: fibrous cartilage is not as strong and elastic as the original hyaline cartilage. In addition to lack of stability, it does not always fill the defect entirely. Therefore, this method can be used to delay joint replacement.
Postoperative period and rehabilitation
In the early postoperative period, ice packs are applied to the operated knee - this reduces the risk of hemarthrosis. The use of anticoagulants is also undesirable, as they increase the risk of hemarthrosis.
The joint can be loaded the very next day if plastic surgery was performed with one graft, but only with a limited amount of flexion. Otherwise, it is recommended to completely eliminate the load on the joint for up to 3 weeks, and then gradually increase it over 3-4 weeks. After 10 weeks the patient is allowed to run.
Damage to the articular cartilage of the knee
Microfracturing
Stages of microfracturing. Left : Removal of damaged cartilage. Center : Using an awl to create holes in the subchondral bone. Right : Illustration of the reparative response leading to the formation of new healthy cartilage cells.
The goal of microfracturing is to stimulate the growth of new articular cartilage by forming new blood vessels in the damaged area. Using a sharp instrument called an awl, multiple holes are created in the damaged articular surface. These holes form in a bone plate located under a layer of cartilage. This leads to the development of a reparative response. New vessels and new cells grow into the area of damage, from which new cartilage is formed.
Microfracture is performed arthroscopically. This surgery is best suited for young patients with a single lesion of cartilage damage and healthy subchondral bone.
Normal healthy knee cartilage ( left ). Significant defect of the articular cartilage of the knee joint ( center ). Perforation of the subchondral bone in the defect area with an awl for microfracture ( right ).
Tunneling
Tunneling, like microfracturing, stimulates the formation of healthy cartilage. In this case, multiple holes are also formed in the defect area using a drill or knitting needle. This stimulates the development of a reparative response.
Tunneling is also performed arthroscopically, however this technique is less precise than microfracturing and the heat of the drill can damage some tissues.
Abrasive chondroplasty
This operation is similar to tunneling, but instead of drills or wires, high-speed burs are used to remove damaged cartilage down to the subchondral bone.
Abrasion chondroplasty is performed arthroscopically.
Autologous chondrocyte implantation (ACI)
IAC is a two-stage operation that involves culturing new cartilage cells and then implanting them into the area of the cartilage defect.
The first step is to remove healthy cartilage cells from the patient. This is done on an area of the articular surface that is not subject to stress. This step is performed arthroscopically. The tissue containing healthy cartilage cells—chondrocytes—is sent to the laboratory. There the cells are cultivated for 3-5 weeks, thereby increasing their number.
The second stage is arthrotomy, i.e. open joint surgery in which these cartilage cells are implanted into the defect area. The articular cartilage defect is pretreated. The defect area is then covered with a flap of periosteum, which is sutured along the periphery of the defect, and the suture area is additionally sealed with fibrin glue. A solution containing a suspension of chondrocytes grown in the laboratory is injected into the defect under the periosteal “patch” using a syringe.
IAC is most effective in young patients with single cartilage defects larger than 2 cm in diameter. The advantage of this method is that it uses the patient's own cells, which eliminates the risk of rejection. Disadvantages include two stages of surgery and the need for open access to the joint. All together it takes several weeks.
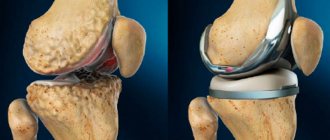
Osteochondral autotransplantation (mosaic plastic)
In osteochondral autotransplantation, cartilage is moved from one part of the joint to another. Healthy cartilage tissue - a graft - is taken from an area that is not subject to stress (non-load zone). The graft has the shape of a cylindrical plug consisting of cartilage and subchondral bone. In the area of the defect, a cylindrical channel corresponding in size is formed, in which this plug is installed. In this way, a smooth articular surface is restored.
This osteochondral plug may be one or there may be several. This operation is called mosaic plastic surgery.
Osteochondral autoplasty is used for relatively small cartilage defects. This is due to the fact that the areas of the joint where the graft can be harvested without compromising the function of the joint are quite limited. The operation can be performed arthroscopically.
Mosaic version of osteochondroplasty
Osteochondral allotransplantation
If the cartilage defect is too large to undergo autoplasty, alloplasty may be considered. Allotissues are tissues of cadaveric origin. As with autoplasty, they are blocks consisting of cartilage and subchondral bone. In laboratory conditions, such blocks are processed and sterilized. They are preliminarily tested for the absence of blood-borne infections.
Allografts are usually larger than autografts. They can be shaped to exactly match the shape of the defect.
Alloplasty is most often performed openly.
Stem cells and tissue engineering
Modern research is focused on new ways to create healthy tissue in the human body. The science that deals with this is called tissue engineering. Growth factors that stimulate the formation of new tissues can be isolated and used, among others. to stimulate the growth of new cartilage tissue.
Another subject of research is mesenchymal stem cells. These are the precursor cells of all other cells in the human body. Their source is living tissues of the body, for example, bone marrow. If such a cell is placed in a specific environment, it will give rise to new cells similar to the cells of the corresponding body tissue.
It is hoped that stem cells placed in areas of damaged articular surfaces will stimulate the growth of new hyaline cartilage.
Tissue engineering is still in the experimental stage of its development. Most of the work in this area is carried out in research centers and is part of various clinical studies.