When it comes to basic physical training (BPT), the prone flexion and extension is the first exercise that comes to mind for many. And this is not surprising, since absolutely everyone knows it, even those people who are far from the topic of sports. In our article today, we will tell you in detail about performing flexions and extensions of the arms while lying down, the nuances and features of this movement, and also share a few tips that will help you improve the technique of this exercise.
Lower limb
The starting position should be considered the position in which the joint is installed with a free vertical position of the torso and limbs.
SHOULDER JOINT
The starting position is the position of the arm hanging freely along the body. Possible movements: abduction, forward flexion, backward extension, outward and inward rotation.
Abduction in the shoulder joint is partially carried out together with the scapula. In a healthy shoulder joint, abduction is possible up to 90° (without the participation of the scapula - Chaklin), and up to an angle of 180° - with the scapula. The protractor is attached to the joint from behind in the frontal plane, the hinge should coincide with the head of the humerus, one of the branches is installed along the body parallel to the spinal column, the other along the axis of the shoulder. To avoid deviation of the torso in the opposite direction, it is recommended to move the healthy arm at the same time as the patient.
Flexion (raising the arm forward) in the shoulder joint occurs in the sagittal plane, in the same plane a protractor is installed on the outer surface of the shoulder, one branch runs vertically, parallel to the body, so that the patient does not throw the body back. Flexion in the unchanged joint is possible by 20-30° (Gerasimova, Guseva) and with the participation of the scapula by 180°. Chaklin points out that 90° flexion is possible. According to Marx – 70°.
Extension also occurs in the sagittal plane. The protractor screw is installed in the middle of the head of the humerus. Extension is possible up to an angle of 45° (according to Marx 37°), it depends on the elasticity and fitness of the ligamentous apparatus of the joint and muscles. Therefore, it is necessary to measure extension in diseased and healthy joints.
Shoulder rotation is measured with the patient in a supine position. The arm is bent at the elbow joint at a right angle. The protractor is applied to the forearm so that its screw is at the level of the olecranon, the branches of the protractor go in the middle of the forearm, which is in the average physiological position (the average between supination and pronation).
When rotating the shoulder inward or outward, one branch of the protractor follows the movement of the forearm, the second remains in the sagittal plane. In a healthy shoulder joint, outward rotation is possible by 80°, inwardly by about 90° (compare with the rotation of the other shoulder). According to Marx, internal rotation is 60°, external rotation is 36°.
ELBOW JOINT
Possible: supination, pronation, flexion and extension.
When measuring flexion and extension at the elbow joint, the forearm is in a mid-position between supination and pronation. The protractor is applied to the outer surface of the arm, the screw is at the level of the outer condyle of the shoulder. One branch goes along the middle of the shoulder, the other to the third finger of the hand. In a healthy elbow joint, flexion is possible up to an angle of about 40°, extension up to 180° (according to Marx, extension/flexion 10°/0°/150°).
Supination and pronation occur due to rotation of the head of the radius around the longitudinal axis of the bone and movement of the lower end of the radius around the lower end of the ulna. The hand is connected to the lower end of the beam, the latter also changes its position (supination - hand with palm up, pronation - palm down).
Starting position: shoulder lowered, elbow at a right angle and pressed to the body. The forearm is in a horizontal plane, the forearm and hand are in a position midway between supination and pronation. Protractor in the frontal plane in front of the hand. The protractor screw is at the level of the extended third finger. Both branches are shifted and are in a vertical position.
RADIAL JOINT
Possible: flexion, extension, abduction and adduction. Starting position – the hand is turned downwards and has one axis with the forearm. The goniometer is located on the side. On the side of the fifth finger, the screw is at the level of the joint space of the wrist joint. One branch runs along the ulnar side of the forearm, the second along the fifth metacarpal bone.
The extension angle varies individually and is equal to 110°.
Flexion in a healthy wrist joint is possible up to 130° (according to Marx, from the zero position flexion/extension is 80°/0°/70°).
When determining abduction and adduction in the wrist joint, the starting position is: the forearm and hand along the same axis in the supination position. The protractor is applied to the palmar surface of the hand, the screw is on the line of the wrist joint. One branch runs along the forearm, the other along the third metacarpal bone. Protractor arrow 180°.
Abduction (movement towards the thumb) in a healthy joint is possible up to 160°, adduction (movement towards the little finger) is possible up to an angle of 135° (according to Marx, according to the neutral position - radial/ulnar abduction 20°/0°/30°).
Metacarpophalangeal and interphalangeal joints
Possible: flexion and extension.
Starting position: the metacarpal bone and the main phalanx of the finger are located along the same axis. The goniometer is attached to the outer (movement in the 5th and 4th fingers) or inner (movement of the 1st, 2nd, 3rd fingers) side of the hand. Flexion in the metacarpophalangeal joint of the II, III, IV, V finger is possible up to 80°, extension up to 0°.
The metacarpophalangeal joint of the thumb has a different range of motion: flexion up to 45°, extension up to 15°.
Flexion and extension are possible at the interphalangeal joints. The protractor is placed on the side of the finger, the branches run along the phalanges of the fingers. Flexion is possible up to 90°, extension up to 0°.
When flexion is limited, when the ends of the fingers do not reach the palm, the distance (in cm) to the end of the fingers or nail phalanx from the middle of the palm should be measured at the maximum possible flexion.
HIP JOINT
The starting positions can be: lying on your back, or on your side with your legs extended.
Possible: abduction, adduction, flexion, extension, inward and outward rotation.
When measuring abduction and adduction, the starting position is on the back, the protractor screw is at the level of the middle of the inguinal fold, one branch runs along the middle of the thigh, the other along the front surface of the body parallel to the midline.
The angle formed between the thigh during abduction and the length of the body is noted. In a healthy joint this angle is 130°. Adduction is possible up to an angle of 160-150°. If movement is severely limited, the assistant must fix the patient's pelvis. According to the neutral (0) position (according to Marx), abduction/adduction 50°/0°/40°.
Hip flexion can be measured in the supine position or on the unaffected side. The protractor is attached to the outer surface of the joint, the screw is at the level of the greater trochanter. One branch goes on the outer surface of the thigh, the other on the lateral surface of the body. The angle of flexion in healthy people is different (muscle, subcutaneous fat), therefore, for comparison, the angle of flexion is measured in the other leg.
Extension in the hip joint is determined with the patient positioned on the stomach or healthy side. Protractor for the outer surface of the thigh and torso. Extension varies from person to person and depends on the elasticity of the joint ligaments. The angle between the thigh and the torso can be 165°; in order for the measurement to be correct, one must ensure that the pelvis does not tilt forward or backward, for which the healthy leg must be straight or an assistant fixes the pelvis. According to Marx, extension/flexion is 10°/0°/130°.
Rotation is determined with the patient lying on his back, with his legs extended. The patellas are facing upward. The soles of the feet are at a 90° angle to the shin. The protractor is placed in the middle of the foot, the jaws are closed, they go to the second toe, the protractor screw is in the middle of the heel. (It is possible to determine rotational movements with the limb bent in the hip and knee joints at an angle of 90°, the branches of the protractor are located along the axis of the lower leg.
) In internal or external rotation, the entire leg rotates inward or outward, with one branch following the movement of the foot, the other remaining in place. Rotation outward by 60°, inward by 45° (depending on the elasticity and fitness of the ligamentous apparatus). According to Marx, rotation is external/internal 50°/0°/50°.
KNEE-JOINT
Possible: flexion and extension.
When measuring flexion, the patient can lie on his back, on his side or on his stomach, depending on the performance of which muscle groups we are testing. The protractor is applied to the outer surface of the leg, the screw at the level of the joint space of the knee joint. Flexion in a healthy knee joint is possible up to 45°, extension up to 180° (depending on the development of muscles and the subcutaneous fat layer).
Abduction and adduction in the knee joint becomes possible with certain diseases or after injury as a result of damage to the ligamentous apparatus.
ANKLE JOINT
Possible: flexion, extension, supination and pronation.
Flexion and extension occur at the supratalar joint. The protractor is attached to the inner side of the ankle joint, the screw is at the level of the inner ankle, one branch goes along the middle of the shin, the other to the metatarsophalangeal joint of the big toe. In the middle position between flexion and extension (a person stands, leaning on the entire sole), the plane of the sole is at 90° with respect to the lower leg.
When bending (moving towards the sole), this angle increases and can reach 170°.
During extension (movement to the rear), the angle decreases and can be up to 70°.
According to Marx, dorsiflexion/plantar flexion is 20°-30°/0°/40°-50°.
Brachial plexus lesions
The brachial plexus includes : axillary nerve (nervus axillaris), musculocutaneous nerve (nervus musculocutaneus), radial nerve (nervus radialis), ulnar nerve (nervus ulnaris), median nerve (nervus medialis). The anterior branches of the four lower cervical nerves and two upper thoracic nerves take part in the formation of the brachial plexus (plexus brachialis). The brachial plexus has two parts: supraclavicular and subclavian. The nerves that form the brachial plexus innervate the muscles of the shoulder girdle and upper limb. The anterior branches of the thoracic nerves do not participate in the formation of the brachial plexus. They form intercostal nerves that innervate the intercostal muscles, the levator ribs, and the abdominal muscles.
CLINICAL PICTURE
As a result of exposure to various etiological factors, damage to the entire brachial plexus, or its supraclavicular or subclavian part, is possible. The first place among the etiological factors contributing to the development of brachial plexitis is given to infections such as influenza, syphilis, typhus, and brucellosis. Brachial plexitis can be caused by other diseases, in particular gout, diabetes, alcoholism, etc. Injuries, such as shoulder dislocation, injury are also among the etiological factors of damage to the brachial plexus. Damage to the supraclavicular part of the brachial plexus (Duchenne-Erb palsy).
With this pathology, the axillary nerve, musculocutaneous nerve, and radial nerve are affected. In this case, the function of all of the above nerves, as well as the muscles receiving innervation from them, occurs. These muscles are the deltoid, biceps, brachialis, brachioradialis, and supinator. In case of damage to the supraclavicular part of the brachial plexus, abduction of the affected arm, elevation to the horizontal line and adduction to the face are impaired. There is a loss of the flexion-ulnar tendon reflex from the biceps brachii muscle, upon palpation there is a sharp pain in the area of the supraclavicular fossa, all types of sensitivity on the skin of the shoulder girdle are impaired. The muscles of the forearm and hand retain their functional ability.
When the subclavian part of the cervical plexus is damaged, Dejerine-Klumpke palsy develops. The cause of paralysis is dysfunction of the ulnar, radial and median nerves. This leads to movement disorders in the forearm, hand and fingers. There is a disappearance of tendon and periosteal reflexes in the upper limb. On palpation, sharp pain is noted in the area of the subclavian fossa, radiating throughout the arm. In addition, there is a violation of all types of sensitivity on the inner surface of the shoulder, forearm and hand of the radicular type.
SYMPTOMS
Damage to the entire brachial plexus is characterized by the following clinical manifestations:
- paralysis of the muscles of the entire upper limb of a peripheral nature
- periosteal and tendon reflexes decrease or disappear
- persistent pain appears that spreads throughout the arm
- in the zone of innervation of the brachial plexus nerves, all types of sensitivity are impaired
TREATMENT
Treatment should be carried out exclusively by a neurologist. Self-medication is unacceptable.
Knee joint: anatomical structure and functions
The knee joint is one of the largest and most complexly structured joints in the human musculoskeletal system.
It is the complex structure of the knee joint that allows it to withstand significant loads and ensure healthy motor activity, but due to such constant and intense work, the knee is subject to wear and tear faster than other joints.
Contents of the article: Bone structures of the knee joint video! Cartilaginous structures Ligamentous apparatus of the knee joint Synovial membrane
Endurance, complex structure and at the same time a high degree of vulnerability make this joint truly unique.
Bone structures
The knee joint is formed by the ends of two bones - the femur and tibia, as well as the patella (kneecap). In fact, this joint includes two joints: one of them is the femorotibial joint (the connection of two bones) and the femoral-patellar joint (the connection of the cap and the femur).
The biomechanics of the knee joint is very complex. It provides motor functions in several planes, each of which allows the knee to move in several directions:
- flexion-extension;
- rotational (rotational);
- sliding;
- rolling.
The last two movements are designed to cushion the knee joint during sudden and significant compression loads (running, jumping), when soft tissues are unable to fully compensate and absorb the impact energy. In this case, the articular parts of the bones shift (slide) in the joint cavity in order to maintain supporting force.
The rolling motion is a displacement of the articular parts of the bones, which reduces the load on the knee joint in the “wrong” direction of flexion or extension. By slightly rotating around its axis and in relation to each other, the heads of the joint allow the load to be distributed more evenly.
Like any other bone tissue in the human body, knee tissue is susceptible to inflammatory and degenerative diseases - arthritis and arthrosis.
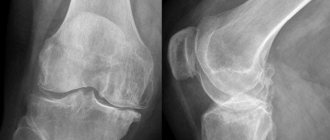
Osteoarthritis of the knee joint (gonarthrosis) is a slowly progressive condition that begins to develop in the cartilaginous tissues of the knee, and if left untreated, gradually affects its bone structures.
As the disease progresses, the articular part of the bones becomes deformed, which significantly reduces or even makes motor activity impossible.
The cause of gonarthrosis can be age-related changes, previous arthritis, a sedentary lifestyle, obesity and other conditions in which metabolic processes in the knee joint are disrupted.
Arthritis of the knee joint (gonitis) is an acute inflammation of the joint caused by the presence of a systemic infection or occurring as a complication of another disease (influenza, ankylosing spondylitis, systemic lupus erythematosus, trauma, etc.).
The complex biomechanics and complex structure of the knee joint (combining two joints in one) causes some instability, which is the cause of dislocations, subluxations and fractures of the internal structures of the knee.
Since the loads on the knee joints can be called the most intense (compared to other joints in the human body), it is in this joint that complex fractures with bone detachment, bone fragments entering the joint cavity, etc. are most often diagnosed.
Such injuries in most cases require surgical treatment, which restores the motor functions of the joint and prevents the development of complications.
Bone structures
But the bone structures play only the role of a frame to which soft tissues are attached, strengthening the knee joint and stabilizing its movements.
Cartilaginous structures
The inner surface of the knee joint is partially lined with cartilage tissue, which softens friction, absorbs stress and protects bone tissue from premature wear. Cartilage also serves as the main source of “nutrition” for the joint - absorbing nutrients from the synovial membrane and adjacent tissues, cartilage saturates bone tissue with them.
But the main elements of the knee joint, which belong to the cartilaginous tissues, are the menisci - elastic crescent-shaped cartilages, the function of which is to increase the supporting force of the knee, prevent its excessive mobility and stabilize all structures of the knee joint when exposed to impact forces (jumping, running, etc.). ).
Thanks to the menisci, the cartilage shells are protected from premature wear, and the entire knee joint as a whole is protected from injury. But the menisci themselves are quite vulnerable and their rupture is one of the most common knee injuries.
Treatment of grade 2 osteoarthritis of the knee joint
Determining the range of motion in the joints and assessing the functionality of the affected segment of the upper or lower extremities is often carried out by examining the degree of their mobility by the doctor. Such diagnostics are carried out only by a specialist from a medical institution. Examining the movements of the affected joints of an active and passive nature, the doctor determines with an inclinometer the angle of their maximum flexion and extension in one surface.
Fixation of mobility is carried out in an imaginary vertical plane, which runs from front to back and divides the human body into left and right parts. Such an examination complements the clinical picture of the joint disease, helps make an accurate diagnosis and prescribe effective therapy.
Basically, the measurement of the range of motion in the large joints of the arms and legs is carried out with a goniometer on a hinge. This protractor, which records the range of motion in the shoulder joint, consists of 2 branches, united by a special hinge and a half-arc with a scale from 0° to 180°. The range of motion in the hip joint or ankle structures is often measured with a goniometer with 4 diamond-shaped jaws.
Every day our joints are exposed to enormous stress. Therefore, it is quite logical that they wear out over time. The human body is not a car; you cannot immediately change a part after a technical inspection. The same applies to the knee joint: it is susceptible to cracks, pathological processes, and dislocations. The most common disease that affects this part of the body is osteoarthritis deformans.
- Symptoms of deforming osteoarthritis of the knee joint Causes of osteoarthritis
- Manifestation of osteoarthritis
- Degrees of the disease
Dystrophic disease of the knee joints caused by damage to the cartilage of the joint capsule is called osteoarthritis. This pathology leads to the fact that the articular cartilage loses its elasticity, becomes soft, thins, and cracks appear in it.
Deforming osteoarthritis of the knee joint can be called a disease of people over 45 years of age who are overweight. The greater the body weight, the faster joint pathology will appear, and the more difficult it will be to resolve. In obese people, it is often the legs that suffer, as they need to support the weight.
Disease of the knee joint begins to appear in the cartilage tissues with pathological changes. Initially, everything happens at the micro level and does not manifest itself clinically. But when exposed to certain factors, the nutrition of cartilage tissue is disrupted, which begins to die. Then the destruction process reaches the periarticular capsule, joint ligaments and menisci.
Knee osteoarthritis is a degenerative pathology and leads to disease of all joint structures and significant deformities. In advanced situations, without proper medical supervision and proper treatment, osteoarthritis leads to disability.
During destruction of the underlying bone cartilage tissue, bone compaction (osteosclerosis) appears and their pathological enlargement, called osteophyte, begins.
All these changes are constantly accompanied by aching pain. In addition to the listed deformities, changes also appear in the periarticular bursae, characterized by thickening of the capsule, inflammation of the tendon sheaths, and spastic muscle contraction. All these processes increase pain and disrupt the function of the joint.
The prevalence of this disease is often explained by minimal physical activity or its absolute absence, which is quite typical for the modern lifestyle of people.
In the knee joint, cartilage connects two bones. Near the cartilage there is synovial fluid, which ensures painless and smooth sliding of two bones relative to each other. Over time, during osteoarthritis, the cartilage is completely worn away, which leads to severe deformations of the knee joint, the appearance of growths and bone outgrowths.
Shoulder pain: What to do?
Home FEFU Medical Center Traumatology and orthopedics, endoprosthetics and reconstructive surgery Pain in the shoulder joint: What to do?
The shoulder joint is the most mobile joint in the human body.
The unique functions of the shoulder joint are determined by anatomical prerequisites:
✔ Ball-and-socket: The large, spherical head of the humerus rotates within the small glenoid socket of the scapula, allowing for a significant range of motion.
✔ Around the shoulder joint there is a capsule and interwoven ligaments and tendons of the muscles surrounding the joint, which provide exceptional mobility and stability to the shoulder joint.
✔ The joint is also surrounded by several muscles responsible for shoulder movement. The short muscles surrounding the joint form the so-called rotator cuff, stabilize the shoulder joint, and participate in abduction, external and internal rotation of the shoulder.
✔ Due to the high degree of joint mobility, injuries often occur. As a result of overloads, chronic microtraumas, sports associated with throwing, striking techniques, lifting weights, as well as in some professions, various pathological conditions arise that require diagnosis and treatment.
What are the symptoms characteristic of shoulder joint pathology?
The most common are: ○ discomfort, pain of varying intensity, possibly spreading to the area of the deltoid muscle, neck ○ limited movement in the joint, decreased range of motion ○ periodically occurring shoulder dislocations with instability (“habitual” shoulder dislocation) ○ noise effects during movements (crunch, knock)
Shoulder joint injuries often occur:
○ before 40 years of age, injuries to the structures stabilizing the joint are more common, which leads to dislocations and instability of the shoulder ○ after 40 years of age, damage to the tendons forming the rotator cuff
Other common pathological conditions of the shoulder: ○ Impingement syndrome of the shoulder joint (from English impingement - “impact”, “collision”) ○ Ossifying (“stone”, calculous) tendinitis of the supraspinatus tendon ○ Osteochondrosis of the cervical spine ○ Adhesive (adhesive) capsulitis shoulder joint ○ Osteoarthritis of the acromioclavicular joint ○ Tumor of the apex of the lung (Pancoast tumor)
What to do if YOU notice the following symptoms?
✔ After a shoulder injury, in the absence of bone damage (examination by a traumatologist), the shoulder hurts for a long time. After playing sports or physical work, my shoulder hurts.
✔ If the pain is dulled for a short time after taking painkillers, using local anesthetic ointments, creams and patches.
✔ The intensity of the pain increases over time, at night you wake up from pain.
✔ After rehabilitation for an injury, the range of motion in the joint is not restored. Against the background of long-term pain, increasing limitation of movements in the joint appears. You limit yourself in everyday life, everyday life, work, sports (it is difficult to dress, take care of yourself, etc.).
✔ With certain movements, such as raising your arm up, moving your arm away from your body, you hear (and often the people around you) a crunching, knocking sound accompanied by unpleasant, painful sensations in the shoulder.
There is no need to self-medicate. You need an examination by an orthopedist, a specialist who will decide whether you need treatment from him, or you need consultations with doctors of other specialties (rheumatologist, vertebrologist, oncologist) to make a diagnosis.
Diagnosis may require an examination ordered by a doctor. Clinical blood tests, x-ray examination of the joint, magnetic resonance imaging of the diseased joint, and in some cases ultrasound of the shoulder joint may be required.
Once a diagnosis is made, conservative treatment and rehabilitation may be prescribed, which should not be neglected. In most cases, competent rehabilitation, exercise therapy, and physical therapy help to achieve satisfactory and good results, significant improvement, and restoration of the function of the sore shoulder.
In some cases, you may be offered surgical treatment, the scope and nature of which depend on the existing joint pathology. It should be understood that treatment does not end after surgery. To fully restore joint function, improve quality of life and social adaptation, serious rehabilitation will be required with the active participation of both doctors and the patient himself.
The author of the publication
is a traumatologist-orthopedist at the Far Eastern Federal University Medical Center A.L. Osipov
What range of motion in joints is considered normal?
| Shoulder structure | 180 | 40 | 180 |
| Elbow joints | 40 | 180 | 90 |
| Hand and phalanges of fingers | 75 | 65 | 20—40 |
| Hip joint | 75 | 180 | 50 |
| Knee | 40 | 180 | — |
With ankylosis, the joint loses mobility.
Partial restriction or complete lack of activity in the joints is called contractures or ankylosis. Contracture is a limitation of passive mobility, and the development of ankylosis causes complete immobility. With this disease, a functionally advantageous and functionally disadvantageous position of each element in the joint structures of the leg or arm is distinguished.
Measuring vibrations: the main rules of the technique
To study the change in oscillation of the upper and lower extremities from the position of free equilibrium, one branch of the device is fixed along the axis of the proximal segment, and the other along the distal segment. It is very important that the hinge rod is aligned with the articulation axis. In this case, angles should be counted only from the anatomical location of the arms or legs.
- significant;
- moderate;
- insignificant.
To correctly assess the viability of the hip joint, the leg must initially be located in the same plane as the body.
- The mobility of the shoulder joints is examined from the anatomical location of the limb when the arm hangs down. The countdown for fixing the amplitude of oscillations of movement in the shoulder joint starts from 0.
- For the ankle, the pathological change in the limits of oscillation is measured when the foot is positioned in relation to the lower leg at an angle of 90°.
- When determining the rotational mobility of the femur, the leg is placed along the axis of the body, and the patella should be rotated exactly anteriorly.
- For the elbow joint, the initial position is full extension of the forearm (180°). To check its pronation and supination, bend the forearm at the elbow 90° and place the hand in the sagittal plane.
- To find out the limits of wrist oscillation, its distal part is fixed along the axial line of the forearm (180°).
- Functional changes in the hip joint, knee or hands are recorded in the initial position of extension up to 180°.
Main conclusions
Assessment of the range of motion in joints is an accessible and inexpensive determination of pathology, allowing you to check and find out how limited the motor properties of the affected joints are. Incorrect range of motion, altered angles of extension and flexion, and impaired amplitude indicate destructive processes in the osteoarticular system.
To restore functionality in the joints of the limbs, the doctor, having studied the deviations in these indicators, prescribes treatment. Joint therapy depends on the stage of the disease and the main cause of its development, so it is individual for each patient. Effective methods of restoring joint mobility and normalizing amplitude include exercise therapy and physiotherapeutic measures.
Hyperextension
Next on the opposite end of the spectrum from flexion is hyperextension. Hyperextension is an extreme version of extension.
You often hear that an athlete has suffered from hyperextension. This is what this diagnosis says.
Hypertension is defined as excessive joint motion in which the angle formed by the bones of a particular joint opens or straightens beyond its normal healthy range of motion. Thus, while extension of a joint refers to stretching or straightening it within its normal limits, hyperextension refers to stretching it excessively beyond its normal range of motion limits.
Since extension is usually limited to a 180-degree range of motion, hyperextension usually refers to bending the joint 180 degrees. Bending a joint in this way often results in injuries such as torn ligaments or tendons, or damaged cartilage.