Pain caused by degenerative processes in the joints causes a person considerable discomfort. One of the mandatory prescriptions of an orthopedic doctor is non-steroidal anti-inflammatory drugs, which sometimes the patient begins to take at his own discretion in large quantities. What do you need to remember so as not to further harm your health?
Uncontrolled use of NSAIDs is a direct path to exacerbation of gastrointestinal diseases
How to treat joint pain.
July 7, 2021
17457
4.4
3
Content
- Why do my joints hurt?
- The best ointments and gels for joint pain
- Fastum gel
- Viprosal
- Finalgon
- Voltaren Emulgel
- Dolgit
- Capsicam
Often joint pain (arthralgia) bothers people who do not have joint diseases. Pain can occur after excessive physical activity, during pregnancy, and in children and adolescents, “growing pains” may occur. In these cases, you don't have to worry. If the joints hurt due to some disease, treatment is necessary. Only a doctor can determine the cause of joint pain and select the correct therapy. So don't let things get worse.
Why do my joints hurt?
There are many reasons for joint pain. Let's look at the main ones.
- Intoxication of the body due to certain diseases.
Diseases such as influenza, ARVI, chickenpox, cholecystitis, tonsillitis, oncology, etc. can cause pain in the joints. Toxins are formed in the body that negatively affect the joints. To eliminate joint pain, you need to cure the underlying disease. - Rheumatoid arthritis.
With arthritis, the joint becomes inflamed. It usually starts with the small joints of the feet and hands, and later the disease affects the ankle, knee, hip, wrist and elbow joints. Severe joint pain appears suddenly and becomes more severe over several days. Painful joints swell, the skin takes on a reddish tint. Rheumatoid arthritis can be suspected by morning stiffness in the joints. Sometimes there is a rash and fever. In advanced cases, the affected joints ache constantly, and the stiffness of movement does not go away. - Rheumatic polyarthritis.
Usually diagnosed a few weeks after the flu or sore throat, but may not be associated with them. The onset of the disease is acute, with high fever. Large joints begin to ache and swell, and symmetrically. Against the background of joint problems, the heart muscle can become inflamed (and this is much more dangerous than arthritis). - Gout.
With this disease, small crystals of uric acid fall into the joint cavity. Most often, the joint of the big toe (which is further from the nail) begins to hurt first. Later, other joints may become inflamed. The attack usually begins abruptly, often at night or in the morning. The pain can be very intense, and the exacerbation can last from several days to several weeks. Attacks of gout recur periodically, and near the joints you can feel tophi - nodes. Gout destroys articular cartilage and ligaments, and over time the joints become deformed. - Reactive arthritis.
The joint becomes inflamed some time after suffering from infectious diseases (chlamydia, pseudotuberculosis, etc.).
The small joints of the extremities are primarily affected; sometimes arthritis affects the large joints. Arthritis has symptoms similar to gout. Sometimes one disease can be distinguished from another only by a blood test: gout - high levels of uric acid in the blood, arthritis - C-reactive protein. The attacks are followed by remissions, and during this time no symptoms of arthritis may be observed. Sometimes arthritis can cause problems with the heart, kidneys and other organs. Read also How to treat varicose veins: top 9 best ointments Varicose veins are easier to treat at the initial stage, so control the development of this disease. To treat varicose veins, there are effective ointments and gels that strengthen capillaries, relieve pain, swelling and inflammation. - Psoriatic arthritis.
This disease may sometimes not be accompanied by skin manifestations of psoriasis, which makes diagnosis difficult. Psoriatic arthritis can be symmetrical or asymmetrical; the pathological process involves small joints of the extremities (closer to the nail), as well as large joints. Intervertebral joints may also be affected. Psoriatic arthritis has symptoms similar to rheumatoid arthritis, arthrosis, or another disease. - Arthrosis.
This disease is characterized by premature wear (degradation) of the cartilage in the joint. Arthrosis is also called osteoarthritis, osteoarthrosis, deforming arthrosis. Arthrosis usually develops in older people with obesity, more often in women. The nutrition of articular cartilage deteriorates due to poor metabolism or injury. Cartilage is destroyed, and the surrounding joint tissues also suffer. Osteoarthritis affects the small joints of the fingers, ankles, knees and hips. Joint pain increases with exercise and decreases with rest. Swelling and crunching appear. In its advanced state, arthrosis causes gait disturbance and even immobility. - Radiculitis.
This disease develops against the background of spinal osteochondrosis, when the distance between the vertebrae decreases and the spinal cord root is compressed. Depending on which part of the spine the pathology develops, pain occurs in the back, chest or neck. With radiculitis, the pain can be very severe and radiate to the arm or leg. - Inflammation of periarticular tissues.
The joint capsule, ligaments or tendons become inflamed, but the joint tissue is not affected. This happens with periarthritis, bursitis, tendinitis. - Injury.
After an injury, the ligamentous apparatus and articular cartilage take a long time to heal, so pain in the joint can be painful for a long time. By the way, arthrosis can develop against the background of injury to the joint and periarticular tissues.
Other causes of joint pain. In addition to the above reasons, there is also functional pain in the joints, when, against the background of disruption of the autonomic system, a spasm of the vessels that feed the joint occurs. Joints can also hurt with systemic lupus erythematosus, systemic sclerosis, ankylosing spondylitis, hallux valgus, avascular necrosis of the femoral head, etc.
Release form of drugs for rheumatoid arthritis
Depending on the stage and specifics of the disease, as well as the patient’s convenience, drug therapy can be prescribed to him in the form of oral medications and injections.
Tablets and capsules
Drugs for rheumatoid arthritis in tablets and capsules are easily dosed and do not require manipulation by medical professionals
. Their disadvantage is the relatively low bioavailability of active substances (70-80%). Some groups of medications for the treatment of arthritis (for example, non-steroidal anti-inflammatory drugs, glucocorticoids) can affect the mucous membranes and are not used for patients with peptic ulcers, gastritis, duodenitis, dyspepsia and other diseases of the gastrointestinal tract. Therefore, they also require the addition of gastroprotective drugs for the duration of the course; they are usually not suitable for permanent use. Medicines in tablets and capsules should usually be taken strictly after meals.
As a rule, drugs in tablets are somewhat cheaper than capsules or injection solutions, and sometimes contain a higher concentration of active ingredients. At the same time, the tablets begin to act more slowly, but provide a longer therapeutic effect. Due to oral administration, the active ingredients of the tablets are partially destroyed in the digestive tract and, alas, are not completely absorbed by the body in the stomach
. Capsules, on the contrary, are a fast-acting release form that has a protective shell against hydrochloric acid, are tasteless and odorless, but spoil much more easily (for example, when carried in a bag). If there are difficulties with finger mobility or during inflammatory diseases of the throat, removing tablets and capsules from the blister can present additional inconvenience.
Injections with drugs to treat rheumatoid arthritis
Injection treatment of rheumatoid arthritis with drugs can be carried out intra-articularly
,
intramuscularly
or
intravenously
.
Intra-articular injection of arthritis medications is considered a last resort
, since it causes additional microtrauma to the joint, it can cause an increased immune response and the risk of progression of secondary arthrosis. In addition, injections of drugs for the treatment of rheumatoid arthritis have a fine-crystalline structure, and therefore can injure articular cartilage.
IM and IV infections bypass the stomach and therefore do not destroy the mucous membranes of the gastrointestinal tract
. However, proper injection requires special skills. Also, injections of drugs for the treatment of rheumatoid arthritis are not suitable for long-term use due to painful administration.
Sachet for rheumatoid arthritis
Sachet
- this is a single dose of medicinal powder in a bag.
Unlike drugs for the treatment of rheumatoid arthritis in injections and tablets, sachets have virtually no disadvantages. They are easy to dose and easy to track the progress of the course. Sachets are taken with ½ glass of warm water, so they have a pleasant fruity drink taste. Taking the sachet does not require the participation of medical professionals and does not create difficulties when swallowing. Due to its excellent solubility, this release form is absorbed by at least 90% and has maximum bioavailability
.
Some drugs for the treatment of rheumatoid arthritis (for example, chondroprotectors) in sachet form can be used on an ongoing basis. Such medications for the treatment of arthritis include Artracam
, which is included in the list of the best chondroprotectors for rheumatoid arthritis.
Fastum gel
Typically, joint pain occurs due to acute or chronic inflammation. There is no point in taking painkillers until the source of the pain calms down. “Fastum Gel” contains ketoprofen (NSAID), which relieves inflammation, which means swelling and pain too. "Fastum Gel" is prescribed for many problems with joints, ligaments and soft tissues. But it is worth remembering that Fastum Gel is contraindicated if the integrity of the skin is compromised. Also, this remedy for joints is not prescribed to children, during pregnancy, during breastfeeding and for some systemic diseases. A huge advantage of Fastum Gel is that it is an excellent pain reliever for joints.
Fastum gel
Berlin-Chemie/Menarini, Germany
Articular syndrome (rheumatoid arthritis, osteoarthritis, ankylosing spondylitis, gout);
symptomatic treatment of inflammatory and degenerative diseases of the musculoskeletal system (periarthritis, arthrosynovitis, tendonitis, tenosynovitis, bursitis, lumbago), pain in the spine, neuralgia, myalgia. Uncomplicated injuries, in particular sports injuries, sprains, sprains or ruptures of ligaments and tendons, bruises, post-traumatic pain. As part of combination therapy for inflammatory diseases of the veins, lymphatic vessels, lymph nodes (phlebitis, periphlebitis, lymphangitis, superficial lymphadenitis). from 208
5.0 1 review
487
- Like
- Write a review
Viprosal
Many people suffering from joint diseases note that with prolonged use of one or another product, addiction occurs - after some time, the ointment or gel simply stops relieving pain, and you have to buy more and more new drugs. If this happens to you, try Viprosal for joints. This is an ointment made entirely of natural ingredients that will give the body a break from NSAIDs. Contains: viper venom, pine resin, camphor and salicylic acid. “Viprosal” has a good irritant effect, which stimulates tissue nutrition - and this is very important when the cartilage is worn out and depleted (with degenerative joint diseases). Viprosal relieves inflammation and reduces pain without the need to take medications.
Viprosal
Grindeks, Latvia
Locally irritating, analgesic, used topically for joint and muscle pain.
Causes irritation of sensitive receptors of the skin and subcutaneous tissue, dilates blood vessels, improves tissue trophism. from 201
5.0 1 review
903
- Like
- Write a review
Finalgon
This ointment contains nonivamide (an analogue of capsaicin), which dilates blood vessels, warms the joint and penetrates deeper into the tissue. Finalgon relieves pain well by “distracting” nerve fibers from transmitting the pain signal to the brain. Finalgon should be used carefully so as not to overdo the warming effect and cause a burn. After rubbing with Finalgon, immediately wash your hands thoroughly with soap so as not to accidentally touch your eyes, mouth or any mucous membranes. Doctors say that with regular use of Finalgon, it is possible to restore joint mobility in case of bursitis and bruises.
Finalgon
Boehringer Ingelheim, Germany
- arthritis;
- arthralgia and myalgia of rheumatic origin; - sports injuries, bruises and damage to the ligamentous apparatus; - myalgia caused by excessive physical activity; - lumbago; - neuritis; - sciatica; - bursitis and tendovaginitis; - acute nonspecific pain in the lower back; - for preliminary “warming up” of muscles before physical exercises, sports competitions; - as part of complex vasodilator therapy for peripheral circulatory disorders. from 246
5.0 1 review
739
- Like
- Write a review
Pharmacological groups of drugs for rheumatoid arthritis
Rheumatoid arthritis requires complex treatment aimed at relieving inflammation and pain, suppressing the immune response, healing erosions on the articular surfaces, restoring nutrition to the joint and periarticular tissues. Various pharmaceutical groups of medications for the treatment of arthritis serve this purpose.
Immunosuppressive drugs for the treatment of rheumatoid arthritis
Immunosuppressants are used as the main group of drugs for rheumatoid arthritis.
- drugs that selectively suppress the activity of certain immune cells.
Since immunosuppressants have different profiles, for rheumatoid arthritis, only drugs designed to suppress autoimmunity are prescribed
. They help relieve inflammation and pain, stop the destruction of articular surfaces, and in some cases, even give the joints a “delay” to recover.
Immunomodulators are always combined with anti-inflammatory drugs and chondroprotectors.
As a rule, basic therapy is taken once a week.
Basic drugs for the treatment of rheumatoid arthritis are used in courses or on an ongoing basis for life. Please note that in case of ARVI and other diseases, immunosuppressants should be stopped until complete recovery.
.
Immunosuppressants are available in tablets, capsules and injection solutions. The best effect is achieved by combining 2-3 basic drugs at the same time.
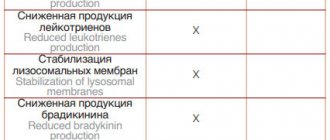
Nonsteroidal anti-inflammatory drugs for the treatment of rheumatoid arthritis
Nonsteroidal anti-inflammatory drugs
in the treatment of rheumatoid arthritis, they help reduce the activity of inflammatory mediators (prostaglandins, enzymes).
They relieve swelling and inflammation, relieve pain, normalize blood circulation and metabolism of tissues around the joint, and facilitate movement in the diseased joint. NSAIDs irritate the mucous membranes of the stomach and intestines, and therefore are used in short courses of 10-12 days to relieve exacerbations. This group of medications for the treatment of arthritis has only a symptomatic effect and does not help restore the joint or stop the progression of the disease
.
NSAIDs are available in the form of tablets, capsules, injection solutions, gels and suppositories.
Glucocorticoids
Glucocorticosteroids
(hormonal) drugs are used only in cases where the effect of NSAIDs is not enough to relieve pain.
Since such medications have serious contraindications and complications, rheumatologists recommend using them in short courses no more than 1-3 times a year
. In severe cases, it is possible to use prednisolone for up to 6-12 months. Their more frequent and prolonged use is justified only in case of a sharply unfavorable course of the disease, its rapid progression, or severe complications from basic therapy.
Glucocorticoids can only be taken as prescribed by a doctor and in strict accordance with the dosage, otherwise the condition of the joints may even worsen.
There are many types of drugs for rheumatoid arthritis
Chondroprotective drugs for rheumatoid arthritis
Chondroprotectors
is a group of drugs for the treatment of rheumatoid arthritis that contain glucosamine and/or chondroitin sulfate. They are helping:
- Enrich synovial fluid, the quality of which suffers during the inflammatory process. The composition of synovial fluid, the natural lubrication of the joint, is directly related to its health. If the viscosity is insufficient, the lubricant does not ensure sliding of the articular surfaces and normal shock absorption of the joint. Its depletion leads to the fact that the cartilage tissue does not receive enough nutrients, loses its elasticity, dries out and cracks. At the same time, normal cartilage regeneration is also inhibited, because new cells grow unstable and are quickly destroyed.
- Strengthen cartilage cells, making them more resistant to adverse factors. This helps to grow new cartilage tissue and even completely restore small areas of erosion on the cartilaginous lining of the joint. Thanks to chondroprotectors, the progression of the disease slows down. Maintaining and preserving cartilage helps delay the disability of rheumatoid arthritis for many years!
- Avoid switching to heavier medications or delaying their use.
To achieve a lasting effect, chondroprotectors are taken in long courses of 3-6 months, 1-2 times a year. Since they have virtually no contraindications and cannot cause complications, this group of drugs remains one of the preferred ones in the treatment of rheumatoid arthritis.
Chondroprotectors are produced in the form of tablets and capsules, injections, sachets and gels. Artracam is considered one of the best chondroprotectors
.
Angioprotectors and microcirculation correctors
Microcirculation correctors
used as auxiliary drugs to prevent complications. On the quality of blood circulation, incl. in small capillaries, the nutrition of the joint depends. In severe cases, disruptions in the circulatory system and subchondral sclerosis of the articular surfaces can lead to death (necrosis) of the bone heads that form the joint.
Swelling and inflammation can cause compression of the articular walls
;
Vasculitis
(inflammation of blood vessels) is also common in rheumatoid arthritis
Antispasmodics and muscle relaxants
The inflammatory process in the joint also affects the soft periarticular tissues. Muscles and ligaments are no exception. Constant muscle tension accelerates muscle atrophy in rheumatoid arthritis due to their destruction and increases the feeling of fatigue. Spasms can also cause serious discomfort: intensify or cause pain (cramping pain), interfere with normal sleep, the patient’s movement and performance of household chores, and cause disturbances in fine motor skills.
New generation drugs for the treatment of rheumatoid arthritis
New generation drugs in the treatment of rheumatoid arthritis mean genetically engineered biological drugs that control the course of the disease. T.N. targeted therapy with synthetic drugs
lasts about 3-6 months from the moment RA symptoms are identified.
The use of new generation products is due to the fact that in rheumatoid arthritis, the cartilage is “self-damaged” by enzymes from the affected cells. Increased production of cytokines triggers a cascade reaction in cells, provoking chronic inflammation and, as a consequence, disability of the patient.
Modern biologics help slow down this process by blocking cytokines (messenger molecules that are responsible for the body's immune responses) or producing antibodies to them, inactivating T-lymphocytes, or otherwise preventing the transmission of signals to attacking immune cells.
In some cases, according to rheumatologists, it is possible to get by with new generation drugs for the treatment of rheumatoid arthritis.
Voltaren Emulgel
The active ingredient in this ointment for joint pain is diclofenac. Among ointments with NSAIDs, Voltaren Emulgel has long occupied a leading position. Due to its ability to perfectly relieve inflammation in the joints, this remedy is often prescribed for injuries and all kinds of age-related changes in the joints. "Voltaren Emulgel" relieves pain in different tissues: connective, bone and muscle. That is, this ointment for joint pain treats complex joint problems.
Voltaren emulgel
Novartis Europharm Ltd, UNITED KINGDOM
Voltaren emulgel is a non-steroidal anti-inflammatory drug (NSAID).
It has a pronounced analgesic, anti-inflammatory and antipyretic effect. from 92
5.0 1 review
970
- Like
- Write a review
Drugs for the treatment of rheumatoid arthritis at different stages
The specifics of treatment depend on how far the changes in the cartilage and bone tissue of the joint have gone
. Since many medications for rheumatoid arthritis, when taken for a long time, have a negative effect on the condition of internal organs, doctors are trying to move from safe drugs to potent ones.
Stage 1 of the disease
After stopping the first inflammation in rheumatoid arthritis, taking chondroprotectors
and
immunosuppressants
. This supportive therapy gives the body the opportunity to recover on its own.
NSAIDs
are used only in the acute phase of the disease.
Also, in the early stages of RA, long-term remission is possible, which is maintained not by the use of heavy drugs, but by following a diet. It is important to dress according to the weather, alternate periods of exercise and periods of rest, be less nervous, take vitamin courses 2 times a year
.
At stage 1 of the disease, glucocorticoids are never used
- they are indicated only in case of a destructive process with the formation of bone erosions. Antispasmodics, painkillers and microcirculation correctors, as a rule, are not required.
In the early stages of arthritis, it is important to maintain a moderate lifestyle and daily routine.
Stage 2 of the disease
At the second stage of the disease, rheumatologists usually add anti-inflammatory drugs (NSAIDs), angioprotectors, decongestants to chondroprotectors and immunosuppressants, and, in the presence of spasms, muscle relaxants. In addition to external agents (gels, ointments, creams, balms), systemic therapy drugs are added. If the course is unfavorable, new generation drugs for the treatment of rheumatoid arthritis are usually prescribed.
Stage 3 of the disease
Stage 3 rheumatoid arthritis is characterized by severe destruction of the joints, therefore basic therapy, drugs for the treatment of new generation rheumatoid arthritis, NSAIDs and glucocorticoids come first, and chondroprotectors are taken exclusively as an auxiliary supportive agent. Patients may also be prescribed additional medications to mitigate the side effects of the main therapy.
Dolgit
This joint remedy perfectly relieves pain and swelling, restoring joint mobility. “Dolgit” is indicated for gout, rheumatism, arthritis and other joint problems. This ointment is also prescribed for dislocations and bruises. “Dolgita” contains herbs with an anti-inflammatory effect, and the active substance here is ibuprofen. The positive effect after applying the drug begins within 15 minutes and lasts about five hours.
Dolgit
Dolorgiet, Germany
The drug has a local analgesic, anti-inflammatory and anti-edematous effect.
Suppresses the production of inflammatory mediators. Non-selective blocks cyclooxygenase (COX-1 and COX-2) and have an inhibitory effect on the synthesis of prostaglandin E2 (GTGR.2), prostacyclin (PG12) and thromboxane B2 (TV2). The analgesic effect is most pronounced for inflammatory pain. Causes a decrease or disappearance of pain, including pain at rest and during movement; reduces morning stiffness and swelling of joints. Helps increase range of motion. In addition to the anti-inflammatory effect, ibuprofen reduces platelet aggregation at the site of inflammation, as well as the migration of leukocytes and the release of lysosomal enzymes in the area of inflammation. from 91
5.0 1 review
2063
- Like
- Write a review
Adverse effects of NSAIDs
Even short-term use of NSAIDs in a certain proportion of patients leads to the development of serious side effects. The most common adverse effects of NSAIDs are:
- damage to the gastrointestinal tract;
- violation of platelet aggregation (sticking);
- kidney damage;
- negative effect on the circulatory system.
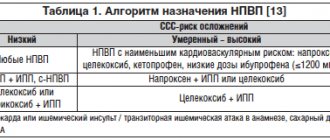
The side effects of NSAIDs are associated with the suppression of the activity of the “physiological” isomer of COX (COX-1). Other unwanted effects are less common. Most often, in elderly people suffering from concomitant diseases, long-term use of NSAIDs develops coronary heart disease, diabetes mellitus, and renal failure.
The risk of developing serious complications in a number of NSAIDs increases as follows: ibuprofen, diclofenac, naproxen, indomethacin. For most NSAIDs, the risk of gastrointestinal bleeding becomes maximum on average by the eighty-fourth day of treatment, for indomethacin - during the first seven days. Endoscopic features of NSAID gastropathy, which make it possible to distinguish it from ulcers associated with Helicobacter pylori, are the predominant localization of damage in the antrum of the stomach, moderate or minimally expressed signs of inflammation of the mucous membrane.
The relative risk of developing serious complications from the gastrointestinal tract occurs in the following cases:
- availability of information about previously diagnosed peptic ulcer disease;
- use of high doses of NSAIDs;
- simultaneous use of NSAIDs of various groups (including low doses of aspirin);
- elderly patient (over 70 years old);
- taking anticoagulants and high doses of glucocorticoid hormones.
If there is a risk of developing digestive complications from NSAIDs, doctors at the Yusupov Hospital prescribe synthetic prostaglandins and proton pump inhibitors to patients. Histamine H2 receptor blockers are effective in treating NSAID-induced ulcers and erosions of the duodenum, but not the stomach. Proton pump inhibitors appear to be more effective than histamine receptor blockers and misoprostol. The course of therapy with proton pump inhibitors should be at least four weeks. For large sizes and localization of ulcers in the stomach, it varies from 8 to 12 weeks. Patients take “gastroprotectors” throughout the entire duration of the NSAID course.
An increased risk of developing cardiovascular pathology is observed when patients with arthrosis take naproxen, celecoxib, ibuprofen, diclofenac and rofecoxib. Indomethacin, naproxen, piroxicam in moderate therapeutic doses and ibuprofen in high doses reduce the effectiveness of diuretics, beta blockers, and ACE inhibitors. When using non-selective NSAIDs (indomethacin, ibuprofen, piroxicam, pyrazolone, aspirin) and non-narcotic analgesics (analgin, phenacetin, paracetamol), acute kidney damage (nephropathy) and acute renal failure develop.