Our expert
Marina Pozdeeva
City Dnepropetrovsk
First category pharmacist and pharmacy manager. Author of numerous works on pharmacology and pharmacotherapy
Disappointing statistical reports indicate that almost 80–90% of people over the age of 65 years have radiographic evidence of osteoarthritis [1]. This disease often proceeds hidden for many years, and then attacks a person with unbridled force. What are the ways to control it with medication and can a pharmacist help a customer suffering from osteoarthritis of the joints?
Difficulty of definition
The concept of “osteoarthritis” is not as simple as it seems. It is understood not as one pathology, but as a whole group of degenerative joint diseases that have similar manifestations. The “point of application” of osteoarthritis is, as a rule, large joints that bear the main load: knees, hips, shoulders, and lumbosacral joints. Sometimes smaller joints of the hands are also involved in the pathological process. The crooked fingers of elderly people, striking at just a quick glance, are a clear sign of progressive osteoarthritis.
With a local course of the disease, one or two joints are affected, and with a generalized course, three or more joints are affected. In the first case, osteoarthritis of the knee joints - gonarthrosis - most often develops. It is one of the main causes of disability in Russia [2]. By the way, women suffer from gonarthrosis more often than men: the gender ratio is 1.7:1 in “female favor” [1]. In general, the weaker sex with osteoarthritis is much more “lucky” than the stronger sex. Women are the leaders among patients over 55 years of age, and the severe course of the disease—erosive osteoarthritis—occurs 12 times more often in them than in men [1].
Risk factors
Experts distinguish between primary, or idiopathic, osteoarthritis, the cause of which remains unknown, and secondary, which develops due to known risk factors.
One of the main factors is age. It is known that the prevalence of osteoarthritis increases critically among people over 50 years of age. Doctors associate this trend with inevitable age-related changes in the synthesis of the main building materials of bone, cartilage and connective tissue, collagen and proteoglycans, leading to a decrease in the tensile strength of articular cartilage and a decrease in its nutrient content. Obese people who are overweight or obese are also more prone to developing osteoarthritis - the higher the body weight, the greater the load on the load-bearing joints.
Risk factors also include injuries, including in the distant past, muscle weakness, infectious diseases, some blood diseases (for example, sickle cell anemia), diabetes mellitus, genetic metabolic disorders, inflammatory arthrosis. The likelihood of developing osteoarthritis in women with low estrogen levels increases, which partly explains “sexual injustice” in old age. They make a negative contribution to joint health and working conditions. Regular heavy physical activity also takes its toll, leaving a “destructive” mark on cartilage and large joints.
Pathogenesis: how does it happen?
The first obvious sign of the disease is pain. As a rule, it is accompanied by a decrease in the range of motion and the appearance of crunching in the joints. During or after rest, including at night, patients experience joint stiffness, which disappears half an hour after activity is restored.
For a long time, osteoarthritis of the joints was considered exclusively a degenerative disorder characterized by the biochemical breakdown of cartilage. However, today there is no longer any doubt that both bone and connective tissue are involved in the pathological process, and inflammation plays an important role in it.
The disease begins with an increase in the synthesis of the main component of connective tissue - proteoglycans, leading to swelling of the cartilage. This stage can continue for many years, often without any clinical manifestations. Sometimes the patient is surprised to notice only some swelling of the joint, but often does not attach any importance to it. Meanwhile, osteoarthritis is gaining momentum: the qualitative composition of proteoglycans and the cartilage itself is gradually changing, irreversible biochemical changes are developing, promoting further regeneration of both cartilage and bone tissue.
As the disease progresses, the release of pro-inflammatory mediators into the tissue, triggering the inflammatory response, increases. In addition, as a result of chronic inflammation, so-called angiogenesis occurs - the process of creating an additional network of blood vessels, which further activates inflammation. Ultimately, vertical clefts and cracks form on the surface of the cartilage, and it loses elasticity and functionality. In severe cases, the function of the cartilage is completely disrupted, which is accompanied by impaired joint mobility. The prognosis for osteoarthritis is most unfavorable in elderly people with a high body mass index, especially if several joints are involved in the pathological process.
NSAIDs
The most effective drugs for the treatment of arthrosis are non-steroidal anti-inflammatory drugs. Paracetamol is the drug of choice for the treatment of arthrosis of the knee joint and other localizations in patients with moderate pain. According to European recommendations (ESCISIT), the daily dose of paracetamol for continuous use is 2-4 g. In Russian recommendations, which are closer to real clinical conditions, the recommended dose of the drug for continuous use should not exceed 2 grams per day. At the indicated dose, paracetamol can be safely taken for the treatment of arthrosis for two years. When using higher doses of the drug, especially in elderly patients, the frequency of adverse reactions significantly increases.
To treat patients with arthrosis, doctors at the Yusupov Hospital use the following NSAIDs:
- acetylsalicylic acid - duration of action from 4 to 6 hours, single dose varies from 500 to 1000 mg, the highest daily dose is 3000 mg;
- ibuprofen – duration of action is 6-8 hours, single dose is 200-400 mg, daily dose is 2400 mg;
- diclofenac - acts for 8-12 hours, a single dose is 50-100 mg, a daily dose should not exceed 150 mg;
- indomethacin – duration of action is from 6 to 12 hours, a single dose is in the range of 200-400 mg, the highest daily dose is 2400 mg;
- naproxen – used 250-1000 mg at a time, but not more than 1200 mg per day, valid for 12 hours.
Non-selective NSAIDs can have significant side effects during long-term treatment of arthrosis. If there is a high risk of complications, doctors at the Yusupov Hospital use selective COX-2 inhibitors to treat arthrosis: meloxicam 7.5-15 mg once daily, nimesulide 100-200 mg twice daily, celecoxib 100-400 mg once daily . For the treatment of osteoarthritis, NSAIDs are used only during periods of increased pain in minimally effective doses.
Clinical manifestations of osteoarthritis
The initial manifestation of osteoarthritis is pain. As a rule, it is accompanied by a decrease in the range of motion and the appearance of crunching in the joints. During or after rest, including at night, patients experience joint stiffness, which goes away on its own within half an hour after activity is restored. Morning stiffness is also characteristic of another disease, rheumatoid arthritis, but it lasts longer than with osteoarthritis - an hour or even more.
Osteoarthritis of the fingers more often develops in women, disfiguring the phalanges of the fingers. Heberden's nodes appear on them - pathological growths, while in most cases inflammatory changes, which are accompanied by severe pain, remain mild or completely unnoticed.
Diagnosing osteoarthritis is not difficult - the most common x-ray, as a rule, perfectly visualizes the destructive processes in joints and cartilage. And then it’s a matter of treatment.
Non-steroidal anti-inflammatory drugs for osteochondrosis
Nonsteroidal anti-inflammatory drugs (NSAIDs) or drugs (NSAIDs) are a group of drugs that have analgesic, anti-inflammatory and antipyretic properties. The term “non-steroidal” in the name of the medications indicates their difference from glucocorticoids, which, in addition to the above qualities, carry a lot of undesirable side effects inherent in steroids.
The first anti-inflammatory substance was obtained from willow bark in 1829, it was salicylic acid. At that time, opiates were considered the main painkillers, which were quickly addictive, depressed the psyche and respiratory functions, and had sedative qualities.
Since then, non-steroidal drugs have firmly taken their place in medical practice in the treatment of diseases manifested by muscle pain, fever, inflammation and similar conditions. Modern medicine has significantly expanded the list of non-steroidal anti-inflammatory drugs, which combine high efficiency, improved tolerability and a minimum of side effects. In addition, most of these medications can be purchased in pharmacy chains at fairly affordable prices without a doctor's prescription.
For back pain, osteochondrosis, radiculitis, lumbodynia, neuralgia and other diseases of the musculoskeletal system, NSAIDs are used to eliminate pain, relieve spasms and inflammation of soft tissues, which allows partially restoring the patient’s motor abilities. It should be remembered that anti-inflammatory drugs only relieve pain, but are not a cure for the underlying disease.
Mechanism of action
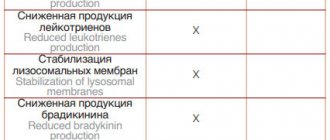
The main and main element of the effect of NSAIDs is the inhibition (suppression) of the synthesis (production) of prostaglandins from arachidonic acid. Prostaglandins are mediators of inflammatory reactions that provoke local dilation of the vascular bed at the site of pathology, swelling, spasm, exudation, migration of leukocytes and other phenomena.
Other biologically active qualities of drugs:
- sensitization (increased sensitivity) of receptors to pain mediators and mechanical influences, by reducing the threshold of pain sensitivity;
- increasing the sensitivity of the cells of the hypothalamus of the brain, which are responsible for thermoregulation, to the effects of endogenous pyrogens formed in the human body when pathogenic viruses, microbes, toxins, etc. enter it.
Less pronounced mechanisms of action:
- inhibition of lipid oxidation;
- stabilization of lysosomal membranes, which prevents the destruction of cellular structures;
- decreased ATP synthesis;
- inhibition of the production of rheumatoid factors;
- disruption or weakening of the conduction of pain impulses along the nerve fibers of the spinal cord, etc.
Classification of NSAIDs
Non-steroidal anti-inflammatory drugs are divided according to the activity of the main effect and chemical composition:
- Drugs with pronounced anti-inflammatory properties:
- group of salicylates (aspirin, diflunisal);
- group of pyrazolidines (phenylbutazone);
- group of oxicams (piroxicam, meloxicam);
- a group of indoleacetic acid derivatives (indomethacin, sulindac);
- a group of phenylacetic acid derivatives (diclofenac);
- a group of propionic acid derivatives (ibuprofen, naproxen).
- Preparations with non-acid derivatives:
- group of alkanones (nabumetone);
- a group of sulfonamide derivatives (nimesulide, celecoxib).
- Drugs with weakly expressed anti-inflammatory properties, but with a strong analgesic and antipyretic effect:
- group of pyrazolones (metamizole, aminophenazone);
- a group of paraaminophenol derivatives (paracetamol);
- a group of anthranilic acid derivatives (mefenamic acid);
- a group of heteroarylacetic acid derivatives (ketorolac).
In this case, according to the increasing anti-inflammatory effect on the human body, drugs can be arranged in the following order: aspirin, amidopyrine, ibuprofen, naproxen, ketoprofen, piroxicam, diclofenac, flurbiprofen, indomethacin.
By increasing analgesic qualities: aspirin, ibuprofen, naproxen, piroxicam, amidopyrine, flurbiprofen, indomethacin, diclofenac sodium, ketoprofen, ketorolac.
Indications for use
Nonsteroidal anti-inflammatory drugs are recommended for the treatment of chronic and acute diseases associated with inflammation, pain, and fever.
Most often, NSAIDs are prescribed for:
- osteochondrosis, spondylosis and other degenerative pathologies of the skeleton;
- osteoporosis, osteopathy, compression fractures of vertebral bodies, pathological fractures of limb bones;
- postural curvatures in the later stages, after surgical intervention in the spinal structures or traumatic injuries to the back;
- myositis, radiculitis, sciatica, lumbodynia, neuritis and neuralgia;
- rheumatoid arthritis, osteoarthritis, gout, inflammatory arthropathy, etc.;
- tumors and metastases in bone structures, accompanied by pain;
- headaches, migraines or fever.
Contraindications
Despite all the positive qualities of anti-inflammatory drugs, we should not forget that they also have certain side effects. They are most often associated with the digestive tract and kidneys (as most NSAIDs are acids), namely:
- peptic ulcer of the stomach or duodenum;
- gastritis or erosive inflammation of the mucous membranes of the gastrointestinal tract;
- gastrointestinal bleeding;
- dyspepsia, diarrhea;
- nausea and vomiting;
- disorders of the liver and kidneys, nephritis, nephrotic syndrome, acute renal failure, which is fraught with retention of sodium and water in the body tissues and the development of arterial hypertension or heart failure.
In addition, drugs of the aspirin group are contraindicated in children under 12 years of age; aspirin and indomethacin cause attacks of bronchial asthma. From the cardiovascular system, blood clotting disorders, cytopenia, myocardial infarction, stroke, peripheral vascular thrombosis and other disorders are possible.
Much less common when treated with anti-inflammatory drugs are:
- dizziness, headaches, confusion, impaired coordination of movements;
- photodermatitis or photosensitivity (increased sensitivity of the skin and mucous membranes to ultraviolet or other rays);
- fermentation disorders;
- allergic reaction or other skin rashes;
- insomnia, increased excitability, nervousness.
List of main drugs used for osteochondrosis
Indomethacin. Recommended for systemic use in the treatment of osteochondrosis, osteoarthritis, spondylitis, gout, rheumatism, spinal pain and other diseases. Taken in the form of tablets, capsules during or after meals, rectal suppositories in a dosage of 25-50 mg 2-3 times a day, but not more than 200 mg. May have side effects on the gastrointestinal tract and nervous system (dizziness, depression, tinnitus, visual impairment).
Ibuprofen. It is used for radiculitis, arthrosis, deforming osteoarthritis, ankylosing spondylitis, gout, bursitis, infectious and inflammatory diseases of skeletal structures. Available in the form of gels, ointments, tablets, capsules, ampoules, suppositories. Prescribed 0.4-0.8 g 3-4 times a day after meals for the treatment of diseases of the musculoskeletal system. To eliminate pain, in case of soft tissue injuries or sprained ligaments - 1.2-2.4 g per day, divided into several doses. May cause heartburn, diarrhea, nausea, dizziness, allergic reactions, etc.
Diclofenac. Used for post-traumatic treatment of joints and soft tissues, muscle pain syndromes, swelling and inflammation, rheumatic and non-rheumatic muscle pain. Available in the form of tablets of various dosages, coated and dissolving in the stomach, solutions for injections, rectal suppositories, gels and ointments of various concentrations. The daily dose when taken orally should not exceed 150 mg, for 1% gel - 2-4 g, 5% gel - 2 g. Local reaction to the use of the drug may be itching, redness, eczema, photosensitivity, peeling, systemic - Klinke's edema, bronchospasm, urticaria, gastritis, ulcer.
Ketonal. The product is intended for the symptomatic treatment of degenerative-dystrophic diseases of the skeleton, as well as for the relief of pain syndromes of various etiologies. The tablet form of the drug is prescribed for oral administration after meals, washed down with water or milk (at least 100 ml), at a dosage of 150-200 mg, divided into 2 doses. You can alternate use: in the morning - in the form of tablets, in the evening - in the form of rectal suppositories. Side effects: nausea, vomiting, diarrhea, flatulence, dizziness, drowsiness, fatigue, nervousness, allergic reactions.
Movalis. It is prescribed in the acute initial period for treatment or in short-term courses to eliminate the symptoms of arthritis, osteochondrosis, spondylitis, rheumatism and other lesions of the musculoskeletal system. Available in the form of gels, ointments, film-coated tablets, ampoules, suppositories. The drug is taken with meals, washed down with a sufficient amount of water at a dosage of 7.5-15 mg/day; a combination of various forms of the substance is allowed (tablets, suppositories, injections), but the daily dose should not exceed 15 mg. Undesirable consequences sometimes caused by the drug: changes in blood composition, drowsiness, disorientation, colitis, gastritis, ulcers, gastrointestinal perforation, nephritis, increased blood pressure, shortness of breath, allergies.
Piroxicam.
Recommended for the treatment of inflammatory and degenerative-dystrophic diseases of the joints and spine, pain and swelling of tendons, muscles, joints, after overexertion, injuries, surgical operations, infectious and inflammatory lesions of body tissues. Taken orally after meals with a sufficient amount of water in a dose of 20-40 mg, divided into 1-2 doses per day. Side effects may include: weakness, insomnia, depression, dry mouth, stomatitis, belching, constipation, rapid heartbeat, surges in blood pressure and other manifestations. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
How to treat osteoarthritis? Main goals of therapy
Treatment of osteoarthritis is a complex process. Along with pharmacotherapy, it should also include non-drug control methods. The importance of therapeutic exercises, physiotherapy and even occupational therapy should not be underestimated. Reducing the load on load-bearing joints also plays a significant role. For osteoarthritis, therapy should include the entire list of measures.
It is impossible to say that the disease can be easily corrected. On the contrary: treatment of osteoarthritis of the joints is a long, difficult and complex process. Along with pharmacotherapy, it should also include non-drug control methods. Patients suffering from increased body weight should make every effort to normalize it. The importance of therapeutic exercises, physiotherapy and even occupational therapy should not be underestimated. Reducing the load on load-bearing joints, for example, knees and hips, also plays a significant role.
Pharmacotherapeutic control over the course of osteoarthritis is based on the use of several groups of drugs.
Anilides
The only modern representative of this group, paracetamol, oddly enough, is included in the list of drugs that are used to reduce the severity of pain in osteoarthritis. Paracetamol has been proven to have a moderate analgesic effect and can be used in accordance with the recommended dosage and course duration.
Non-steroidal anti-inflammatory drugs - NSAIDs
For osteoarthritis, external forms (ointments, gels, patches, suppositories), oral (tablets, capsules), and parenteral forms are used. NSAIDs inhibit the enzyme cyclooxygenase (COX), suppressing the production of inflammatory mediators, which are responsible for both pain and the development of the inflammatory process. It should be remembered that taking oral and injectable non-selective NSAIDs - ketoprofen, ibuprofen, meloxicam, diclofenac, naproxen and some others - can lead to the development of NSAID-associated gastropathy. To avoid such side effects, patients suffering from gastrointestinal diseases are prescribed NSAIDs “under the guise” of proton pump inhibitors (for example, omeprazole). In addition, for safety reasons, local remedies have priority: if they effectively relieve pain and inflammation, they try not to resort to internal dosage forms.
Along with non-selective NSAIDs, selective agents that inhibit only the target COX-2, coxibs (celecoxib), can also be used for osteoarthritis.
Local analgesics
A special place in the local therapy of osteoarthritis is occupied by drugs containing capsaicin. It is a synthetic analogue of a natural compound found in hot peppers. Studies have shown that capsaicin copes well with pain in osteoarthritis. Therefore, authoritative international organizations dealing with the problems of degenerative joint diseases have included capsaicin in the list of drugs recommended for the treatment of osteoarthritis.
In domestic pharmacies, capsaicin is sold in the form of a patch, which is applied to the most painful areas of the skin.
Other drugs
Diacerein is used as a non-narcotic analgesic to reduce the severity of pain. It has also proven to have a moderate analgesic effect. In addition, diacerein is recognized as a safer drug than NSAIDs. Note that one of the most unpleasant side effects when using it is diarrhea.
In cases of severe pain, doctors may resort to prescribing narcotic analgesics, in particular tramadol. In case of pronounced progression of the disease, intra-articular injections of glucocorticosteroids are also prescribed.
Nonsteroidal anti-inflammatory drugs in the treatment of joint diseases
For citation.
Imametdinova G.R., Chichasova N.V. Non-steroidal anti-inflammatory drugs in the treatment of joint diseases // Breast Cancer. 2015. No. 25. pp. 1491–1495. Diseases of the musculoskeletal system are one of the most common reasons for patients to visit a doctor. Widespread prevalence in the population, long-term persistence of pain and inflammation, steady progression, rapid development of disability, deterioration in the quality of life, reduction in its duration, as well as significant economic damage to patients and society determine not only the clinical, but also the social significance of chronic diseases of the musculoskeletal system [1–3]. The main symptoms of musculoskeletal diseases are pain and inflammation. In most cases, pain in various structures of the musculoskeletal system is chronic, and the most common cause of its development is chronic inflammation in the synovium. Long-term persistence of pain and inflammation invariably leads to joint destruction and loss of musculoskeletal function. Treatment of chronic pain and inflammation is a complex task and requires long-term complex anti-inflammatory therapy, one of the components of which is non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs are among the most widely used drugs in clinical practice [4]. They are used by approximately every 4th person on the planet, every 3rd person over the age of 60 [5]. It is well known that the main mechanism of action of NSAIDs is inhibition of cyclooxygenase (COX) activity [6]. Moreover, most of the positive effects of NSAIDs (suppression of inflammation, pain, fever) are associated with suppression of COX-2 activity, and adverse reactions are associated with suppression of COX-1 activity [7–9]. According to the mechanism of action, NSAIDs are divided into non-selectively suppressing the activity of COX-1 and COX-2 (n-NSAIDs) and selectively suppressing the activity of COX-2 (s-NSAIDs). S-NSAIDs are effective in treating pain and inflammation with a lower incidence of adverse reactions compared to n-NSAIDs. Suppression of COX-1 causes a wide range of adverse reactions of n-NSAIDs. The most common is damage to the gastrointestinal tract (GIT) (NSAID gastropathy) [10, 11], which often becomes the basis for interrupting treatment. It should be emphasized that there is no connection between subjective side effects and endoscopically detected ulcers and severe gastrointestinal complications. Thus, in 58–80% of cases, ulcers are asymptomatic against the background of the analgesic effect of NSAIDs [12]. However, clinicians must clearly identify risk factors for the development of severe complications from the gastrointestinal tract - ulcerative bleeding and the cardiovascular system (CVS): myocardial infarction, stroke. In 2015, new clinical recommendations “Rational use of non-steroidal anti-inflammatory drugs in clinical practice” were published, prepared by the Association of Rheumatologists of Russia, the Russian Society for the Study of Pain, the Russian Gastroenterological Association, the Russian Society of Cardiology, and the Association of Orthopedic Traumatologists of Russia [13]. A joint discussion at the expert council developed a unified approach to identifying risk factors for adverse events from the gastrointestinal tract and cardiovascular system. The main provisions presented in the recommendations include: a structured approach to prescribing NSAIDs, stratification of cardiovascular risk factors, and an algorithm for prescribing NSAIDs. The algorithm for prescribing NSAIDs in accordance with the recommendations is presented in Table 1. According to these recommendations, s-NSAIDs are indicated for moderate risk of cardiovascular complications and moderate to high risk of gastrointestinal complications.
It is known that n-NSAIDs have a negative effect on cartilage and aggravate the course of arthrosis, have a negative effect on the function of the liver and kidneys, and in patients with concomitant bronchial diseases, they can cause bronchospasm and aggravate the course of bronchial asthma. In recent years, new data have emerged on the frequency of concomitant pathologies in patients with diseases of the musculoskeletal system. The need for anti-inflammatory therapy, sometimes long-term, more often occurs in elderly people, usually with comorbid conditions and accompanying therapy. According to many authors [14–17], the most common comorbid conditions are arterial hypertension (AH), coronary heart disease (CHD), diabetes mellitus, and gastrointestinal pathology. On the one hand, these are risk factors for intolerance to NSAIDs, and on the other hand, taking NSAIDs aggravates the course of hypertension, congestive heart failure, and reduces the effectiveness of antihypertensive therapy [18–22]. Thus, a drug for the treatment of chronic pain and inflammation should not only have high efficacy, but also a good safety profile. In this regard, the selective COX-2 inhibitor nimesulide, which has been successfully used by doctors of various specialties for about 30 years, is of interest. In terms of its analgesic, anti-inflammatory and antipyretic effects, nimesulide is not inferior to n-NSAIDs, and according to some data, even slightly superior to them [23]. The results of a number of in vitro and ex vivo studies indicate that nimesulide inhibits COX-2 more selectively than COX-1 [24–28] (Fig. 1).
At therapeutic concentrations, nimesulide inhibits 88% of COX-2 activity and 45% of COX-1 activity [29]. Moreover, if the effect on COX-1 stops after 24 hours, the effect on COX-2 lasts much longer [30], and this difference persists with long-term use [31]. This unique mechanism of action explains the low number of gastrointestinal complications. It is very interesting that the low incidence of gastrointestinal lesions during treatment with nimesulide is associated not only with the COX-2 selectivity of the drug, but also with the antihistamine effect, leading to a decrease in the secretion of hydrochloric acid in the stomach [32]. It was also found that nimesulide has the ability to inhibit interleukin-1β (IL-1β) in cultured synovial fibroblasts [33]. There is evidence that, along with COX inhibition, nimesulide has a number of COX-independent mechanisms, among which its ability to inhibit chondrocyte apoptosis is especially important [34]. In addition, the drug and its metabolites exhibit direct antioxidant activity against various free radicals [35]. Nimesulide reduces the degranulation of proteoglycans, inhibits the activity of elastase, collagenase, stromelysin, and suppresses hyperalgesia induced by bradykinin and tumor necrosis factor-α (TNF-α) [25, 27, 36]. The drug is able to suppress the activity of pro-inflammatory cytokines: interleukin-6, TNF-α, metalloproteinases, phosphodiesterase IV enzyme, which activates macrophage and neutrophil activity [25, 37, 38]. The short half-life (1.8–4.7 hours), the rapid achievement of maximum concentrations in blood plasma and synovial fluid determines the high rate of onset of the analgesic effect and a decrease in the frequency of side effects of nimesulide. When taken orally, the drug is quickly and almost completely absorbed, regardless of food intake. Due to its biochemical properties, nimesulide easily enters the site of inflammation. The concentration of free nimesulide directly at the site of inflammation (especially in the joint tissue), where the pH of the environment is lower, can be much higher than its plasma concentration [39, 40]. The results of studies conducted by domestic and foreign authors confirm the high effectiveness of nimesulide in the treatment of acute [41, 42] and chronic pain. Thus, it was shown that the effectiveness of nimesulide was comparable to the effectiveness of diclofenac [43] and naproxen [44] in patients with osteoarthritis (OA) and rheumatoid arthritis (RA) [44, 45]. A number of short-term and long-term studies have been devoted to assessing the safety of nimesulide. According to world literature, the frequency of side effects during treatment with nimesulide ranges from 6.8–36% with a clear dependence on the dose and duration of drug use. In particular, when analyzing the results of several clinical studies that included 22,938 patients with OA treated with nimesulide at a dose of 100–400 mg for 5–21 days (average 12 days), the overall incidence of adverse reactions was 8.2% [47]. According to another multicenter study, which involved 12,607 patients with various rheumatic and orthopedic diseases, during treatment with nimesulide 400–200 mg/day for 21 days, the incidence of side effects was 6.8% [48]. As evidenced by the results of numerous studies conducted by domestic and foreign authors, nimesulide is characterized by good tolerability in the gastrointestinal tract. Thus, Kriegel W. et al. conducted a comparative study of 370 patients with OA who received nimesulide 200 mg/day and naproxen 750 mg/day for 12 months. The effectiveness of both drugs was comparable, and the total number of drug complications when using nimesulide compared to naproxen was lower: 47.5 and 54.5%, respectively [44]. Studies conducted in real clinical practice deserve special attention. Bradbury F. presented data on the frequency of gastrointestinal complications when using diclofenac, nimesulide and ibuprofen. The total incidence of gastrointestinal lesions when using nimesulide was significantly lower compared to that of diclofenac (12.1%) and did not differ from that of ibuprofen - 8.1% and 8.6%, respectively [49]. Domestic authors assessed the safety of the use of nimesulide in real clinical practice in 322 patients with rheumatic diseases who received nimesulide at a daily dose of 200 mg for a long period (12 months). None of these patients had serious gastrointestinal complications such as bleeding or ulcer perforation. Gastric and duodenal ulcers were found in 13.3% of patients [50]. Data obtained from a previous endoscopic study of 4931 patients receiving n-NSAIDs demonstrated a higher incidence of upper gastrointestinal ulcers in 18.1% of patients [51] (Fig. 2). Attention should be paid to the data from a population-based study that assessed the risk of developing gastrointestinal bleeding while taking various NSAIDs. It was shown that the relative risk of bleeding for nimesulide was 3.2, for diclofenac – 3.7, meloxicam – 5.7 [52]. The results of the endoscopic examination conducted by A.E. Karateev demonstrated that when using nimesulide, damage to the upper gastrointestinal tract occurred much less frequently than when using diclofenac, ketoprofen, and indomethacin - the total number of gastric and duodenal ulcers was 4.4% and 14.6%, respectively [53]. In an analysis of 10,608 spontaneous reports of serious side effects of NSAIDs for the period 1988–2000, conducted by Italian scientists [54], it turned out that the frequency of adverse reactions from the gastrointestinal tract while taking nimesulide was 2 times lower than against the background of comparator drugs (Fig. 3).
Of great interest are studies of the safety of using nimesulide in a high daily dose. Thus, the use of nimesulide in a daily dose of 400 mg in patients with RA demonstrated not only high efficiency, but also good tolerability of the drug [55]. Later, domestic authors conducted a multicenter study of the effectiveness and safety of nimesulide in daily doses of 200 and 400 mg in comparison with diclofenac 100 and 200 mg/day for 4 weeks. with EGD control in early RA. The results of the study demonstrated that the effectiveness of nimesulide was slightly higher than that of diclofenac, and the development of ulcers and multiple erosions of the stomach or duodenum while taking nimesulide was significantly lower than in patients taking diclofenac - 1.3% and 5.9%, respectively [ 45]. More recently, the results of a population-based study conducted by Italian scientists were published. The risk of developing NSAID-associated gastrointestinal complications was assessed in 588,827 patients with 3,623,341 prescriptions of various NSAIDs for the period from 2001 to 2008. It should be especially emphasized that the low risk of developing serious gastrointestinal complications while taking nimesulide was comparable to that of celecoxib [56]. Aspects of the cardiovascular safety of s-NSAIDs are widely discussed in the world literature. According to the results of the analysis conducted by A. Helin-Salmivaara et al., the relative risk of myocardial infarction for nimesulide was 1.69, which did not exceed the total risk for the entire class [57]. According to domestic authors, out of 322 patients with RA, myocardial infarction was recorded in 1 man, 68 years old, with a long history of coronary artery disease and hypertension. A persistent increase in blood pressure was observed in 11.5% of patients; in 2 patients with a history of high risk of hypertension, negative dynamics were detected on the ECG [50]. It should be noted that in studies conducted by foreign authors (the results of which were mentioned above), there was no significant increase in the incidence of cardiovascular complications while taking nimesulide [43, 44]. The issues of hepatotoxicity of nimesulide have been repeatedly discussed by the medical community over the past few years. Analysis of literature data indicates that the hepatotoxicity of nimesulide is no higher than that of other NSAIDs [58]. With short-term use of nimesulide (no more than 30 days), an increase in ALT and AST by 2 or more times is observed in only 0.4% of patients, and with long-term use (more than 6 months) the frequency of such changes does not exceed 1.5% [59, 60]. In 322 patients who received nimesulide for 12 months, not a single case of the development of clinical symptoms of liver damage (jaundice, hepatomegaly, symptoms of liver failure) was detected. An increase in the level of hepatic transaminases (AST, ALT) by more than 2 times was recorded in 7 cases (2.2%) in RA patients who also received methotrexate and leflunomide [50]. The largest population-based study of nimesulide hepatotoxicity [61] analyzed the incidence of drug-induced liver injury in 397,537 patients treated with various NSAIDs during the period 1997–2001. It was shown that nimesulide caused hepatopathy in 35.5 cases per 100 thousand patients, which is significantly less common than diclofenac - 39.2 and ibuprofen - 44.6. According to Spanish researchers [62], over a 10-year period of nimesulide use, serious hepatotoxic complications developed extremely rarely (Fig. 4). Interesting are the results obtained by domestic authors while studying the effect of nimesulide on liver function in the treatment of gouty arthritis. As is known, patients with gout often have metabolic disorders and a high frequency of alcohol abuse, which increases the risk of developing adverse reactions from the liver. However, with the use of nimesulide in doses up to 400 mg/day, there was no negative dynamics of biochemical blood parameters indicating damage to liver cells or cholestasis [63].
The results of a meta-analysis over a 10-year period (from 1988 to 1997) demonstrated that per 100 thousand patients taking nimesulide, there were only 11 cases of possible association of renal complications with taking the drug, of which only 4 were treated with nimesulide monotherapy [ 64]. It has been established that nimesulide extremely rarely causes increased bronchospasm in patients suffering from bronchial asthma and hypersensitivity to acetylsalicylic acid or other NSAIDs, since it does not have cross-reactivity with acetylsalicylic acid and n-NSAIDs in relation to the induction of exacerbation of asthma and is one of the drugs of choice (among -NSAIDs) in these patients [25, 65]. As already mentioned, experimental data have demonstrated that nimesulide has no negative effect on cartilage [33, 34]. Somewhat later, W. Kullch et al. in a pilot clinical study, a positive effect of nimesulide on the course of OA of the hip and knee joints was noted [66]. The results of scientific research and extensive clinical experience with nimesulide indicate its high analgesic and anti-inflammatory activity and good tolerability. All of the above served as the basis for the emergence of a number of generics of this drug. Recently, a new generic nimesulide appeared in Russia - Nemulex® in the form of granules for the preparation of a suspension. This dosage form of the drug provides a faster onset of clinical effect compared to the tablet form. A distinctive feature of Nemulex is the absence of the high-calorie polysaccharide maltodextrin in its composition, which allows the drug to be prescribed to patients with diabetes, excess body weight, and metabolic disorders. To date, there are already data on the results of open prospective short-term (10–15 days) clinical studies of the drug at a daily dose of 200 mg in rheumatological and neurological practice [67–69]. Thus, the positive effect of the drug Nemulex® in relation to the main clinical manifestations of ankylosing spondylitis in 30 patients was demonstrated in the NAUTILUS study. According to the authors, 60% of patients achieved clinically significant improvement, while the severity of back pain decreased by 2 times. Adverse reactions included an increase in AST, ALT in 10% of patients (resolved within 1 week with diet and hepatoprotectors) and dyspeptic manifestations in 10% of patients (without the presence of erosive changes in the gastrointestinal tract during EGD control) [67]. Another study was devoted to assessing the effectiveness and safety of Nemulex® in comparison with diclofenac and indomethacin in 30 patients with OA. According to the authors, the effectiveness of all drugs was comparable and did not differ statistically. However, when using Nemulex, the analgesic effect developed approximately 2 days earlier than with comparison drugs. Side effects while taking Nemulex were observed in 4 patients (13% of cases). 3 patients had dyspeptic disorders, 1 had an increase in blood pressure. Adverse reactions were mild and did not require discontinuation of the drug [68]. According to D.I. Lakhin, in 30 patients with OA after 15 days of treatment, there was a disappearance of signs of synovitis, a significant reduction in pain (from 69.3±0.74 to 21±0.29), as well as an improvement in joint function in all patients. Among the adverse reactions, only signs of gastropathy appeared in 2 (6.7%) patients (with a history of gastric ulcer). According to the vast majority of patients (23 people - 76.6%), the treatment was well tolerated, and in 7 (23.3%) it was satisfactory [69]. A study was conducted in an outpatient setting that included 49 patients with dorsopathy. All patients received complex treatment, including Nemulex® and Chondroguard. After 15 days, the majority of patients (29 people - 59.5%) noted the disappearance of back pain. 2 patients (4%) noted the appearance of discomfort in the epigastrium, which led to independent discontinuation of the drug. At the same time, according to the author, control endoscopy did not reveal any pathological changes [72]. Thus, the research results showed that Nemulex® has distinct analgesic and anti-inflammatory properties combined with good tolerability. However, given the short time frame and small number of studies, it is advisable to study the effectiveness and safety of the drug over a longer period of time in different cohorts of patients.
Correctors of bone tissue metabolism in the treatment of osteoarthritis
A group of drugs that correct bone metabolism deserve special mention. These include chondroprotectors glucosamine, chondroitin sulfate, and risedronic acid. The latter is more often used for osteoporosis - it inhibits bone resorption. Combination preparations containing a complex of chondroitin sulfate and glucosamine are also popular among pharmacy clients. Sometimes ibuprofen is added to them as an additional pain reliever and anti-inflammatory component.
Chondroprotectors stimulate bone tissue regeneration and have anti-inflammatory and analgesic effects. Tablet and external forms (for example, chondroitin sulfate in capsules, tablets or ointments, as well as complex products) are classified as over-the-counter drugs. This means that when a client suffering from osteoarthritis comes to the pharmacy for a recommendation, the pharmacist has the right to expand the consultation and advise not only external or internal NSAIDs from the OTC group, but also chondroprotectors that protect cartilage from further damage.