The role of omega-3 unsaturated acids in the prevention and treatment of various diseases
Part 2. Read the beginning of the article in No. 7, 2021.
Non-alcoholic fatty liver disease and non-alcoholic steatohepatitis
Omega-3 polyunsaturated fatty acids have been studied in patients with nonalcoholic fatty liver disease and nonalcoholic steatohepatitis because of their potential hypotriglyceridemic, insulin-sensitizing, and anti-inflammatory effects. Observational studies have shown that patients with non-alcoholic fatty liver disease have low plasma levels of ω-3 PUFA. Several preliminary studies on the effects of ω-3 PUFA supplementation on various aspects of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis (biomarkers of liver damage, liver fat accumulation, and liver fibrosis) have shown some encouraging results. It is noted that the intake of ω-3 PUFAs can reduce radiological and histological indicators of liver steatosis and fibrosis in patients without cirrhosis. In addition, consumption of ω-3 PUFAs is inversely associated with the risk of hepatocellular carcinoma. One study included 442 nondiabetic patients in whom ω-3 PUFA supplementation significantly improved lipid profiles (decreased TG and total cholesterol and increased serum high-density lipoprotein cholesterol) and reduced plasma alanine aminotransferase levels, but with unclear results. implications for signs of steatosis and liver fibrosis and significant heterogeneity between studies. Similar results were also found in a meta-analysis of 4 randomized clinical trials that included 263 children and adolescents with non-alcoholic fatty liver disease. The results of this meta-analysis showed that ω-3 PUFA supplementation reduced hepatic steatosis as assessed by ultrasound and blood tests after at least 1 year of treatment [27, 28].
Application of ω-3 PUFAs in the treatment of inflammatory and dystrophic joint diseases
Omega-3 PUFAs are used in the treatment of inflammatory and dystrophic diseases of the joints - rheumatoid arthritis, osteoarthritis, reactive arthritis, etc. Omega-3 PUFAs are included in antirheumatic therapy in addition or in combination with other antirheumatic drugs. A combined preparation based on ω-3 PUFAs and plant extracts has received recognition from the European League Against Rheumatism (EULAR 2003, 2004, 2007) [29].
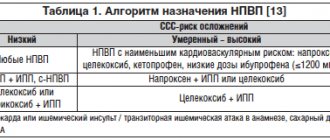
The anti-inflammatory effect of ω-3 PUFAs is due to a decrease in the production of pro-inflammatory eicosanoids (prostaglandin E2, leukotriene B4) from AA, an increase in the production of anti-inflammatory eicosanoids (prostaglandin E3, leukotriene B5), a decrease (due to suppression of the synthesis of leukotriene B4) in the production of platelet aggregation factor, interleukin- 1 and tumor necrosis factor, allows the use of ω-3 PUFAs in the treatment and prevention of various inflammatory diseases with an autoimmune and/or allergic component of pathogenesis, such as rheumatoid arthritis, systemic lupus erythematosus, Crohn's disease and ulcerative colitis, bronchial asthma and atopic dermatitis. For example, during a comparative study of the effectiveness of low doses of EPA and DCG (27 mg/kg and 18 mg/kg, respectively) in 20 patients with rheumatoid arthritis and higher doses (54 mg/kg and 36 mg/kg) in 17 patients, a pronounced reduction, compared with 12 patients in the control group who received olive oil capsules containing 6.8 g of oleic acid, in the number of patients who noted joint pain (at a low dose - by the 24th week and at a higher dose - by the 18th week week (p = 0.04)); the production of leukotriene B4 in neutrophils decreased by 19% at a low dose and by 20% at a higher dose (p = 0.03), while the production of interleukin-1b by macrophages in the control group decreased by 38.5% (not statistically significant), with when prescribing ω-3 PUFAs in small doses by 40.6% (p = 0.06) and when prescribing higher doses of ω-3 PUFAs - by 54.7% (p = 0.0005). A repeat trial attempted nonsteroidal anti-inflammatory drug (NSAID) withdrawal with fish oil and olive oil. In the main group, 8 weeks after discontinuation of diclofenac, patients did not experience a worsening of the disease compared to the control group receiving NSAIDs [30].
Treatment of autoimmune diseases
Because ω-3 PUFAs influence humoral as well as cellular immune factors, they have been used to treat autoimmune diseases. The effectiveness of complex therapy for systemic lupus erythematosus has been shown to increase when ω-3 PUFAs are included in its composition. A similar effect was obtained in the treatment of skin inflammatory and allergic diseases - atopic dermatitis and psoriasis. These studies found that in individuals with skin diseases, the level of arachidonic acid in affected tissues was 8 times higher than in healthy skin. The counteraction of ω-3 PUFAs to the proinflammatory effects of arachidonic acid metabolites (prostacyclin, leukotrienes, lipid peroxides, etc.) largely explains their therapeutic effect [31].
Renoprotective effect of ω-3 PUFA
The use of ω-3 PUFAs in patients with diabetic nephropathy helps reduce oxidative stress and has a positive effect on the condition of the kidneys. Preliminary data have been obtained on the possibility of reducing the rate of sclerosis of the glomerular apparatus in patients with chronic kidney pathology with the use of ω-3 PUFAs. It is possible that this drug may inhibit the progression of chronic renal failure in individuals with chronic kidney disease, which requires further study [32].
Application of ω-3 PUFAs in malignant neoplasms
The basis for studying the possibilities of using ω-3 PUFAs in malignant neoplasms were the results of a number of epidemiological studies that showed that women in Japan and Greenland have an extremely low incidence of breast cancer, which is most likely associated with diet. Traditionally, the diet of the inhabitants of Japan and Greenland includes large amounts of fish and seaweed containing ω-3 PUFAs. The results of subsequent studies revealed that the use of ω-3 PUFAs prevents the development, limits the growth and metastasis of breast cancer. In the mechanism of the protective effect of ω-3 acids against breast carcinogenesis, a decrease in the production of a number of arachidonic acid metabolites (prostaglandins E2 and F2, thromboxane A2), which are stimulators of tumor growth, is important. Along with the effect of ω-3 PUFAs on the synthesis of prostaglandins, a decrease in the immunoinhibitory effect of cortisol and a cytotoxic effect due to stimulation of peroxidation in tumor cell membranes are expected.
The inclusion of ω-3 PUFAs in the diet of women with an increased risk of developing breast cancer for 4 months leads to a significant reduction in the content of a tumor risk biomarker in the blood. In recent years, positive results have been obtained from the use of ω-3 PUFAs in experiments and in clinical settings also for a number of other tumors - colon, prostate [33].
Prevention and treatment of skin diseases
Docosahexaenoic acid is a structural component of the skin and is responsible for the health of the cell membranes that make up the majority of the skin. Healthy cell membranes mean soft, hydrated and elastic skin without wrinkles. Eicosapentaenoic acid provides the following skin benefits [34, 35]:
- controls sebum secretion;
- controls skin hydration;
- prevents follicular hyperkeratosis (small red pimples on the surface of the skin);
- prevents premature skin aging;
- prevents acne.
Omega-3 fatty acids can also protect your skin from sun damage. EPA helps block the release of substances that break down collagen in the skin after sun exposure.
ω-3 PUFAs are very promising for psoriasis, which is considered as a kind of lipoidosis (liponodosis) of the skin. The positive effect of ω-3 PUFA preparations was noted in almost all patients with psoriasis. Good results have been obtained in the treatment of patients with lichen planus and atopic dermatitis [36, 37].
central nervous system
Considering the high content of DHA in the organs of the central nervous system, its participation in the processes of myelination and transmission of nerve impulses, attempts are being made to use PUFAs in the treatment of patients with bipolar mental disorders [11]. Thus, 64.3% of patients who took part in a double-blind, placebo-controlled study of the effectiveness of a dietary supplement with ω-3 PUFAs showed a marked improvement in response to standard therapy, versus 18.8% of patients in the control group (p = 0 ,02). In schizophrenia, a significant relationship was found between the level of ω-3 PUFAs in the diet and the severity of symptoms. In a randomized, double-blind study of hyperexcitability syndrome in combination with decreased attention in children, it was shown that an increase in the content of these acids in the blood serum under the influence of a dietary supplement with ω-3 PUFAs significantly correlates with a decrease in symptoms of hyperexcitability.
Fish oil and Alzheimer's disease have been studied for several years with consistent results. Essential fatty acids, vital to brain function, found in fish oil may not only slow cognitive decline, but also help prevent brain atrophy in older adults. The study, published in the FASEB Journal, looked at the health effects of four to 17 months of supplementation with ω-3 fatty acids and antioxidants. The findings further support the possibility of using fish oil as a weapon to combat the onset of cognitive decline and Alzheimer's disease [38].
Low levels of ω-3 PUFA are associated with sleep problems in children and obstructive sleep apnea in adults. Low levels of DHA are also associated with decreased levels of the hormone melatonin, which helps you sleep. Studies in children and adults have shown that taking ω-3 PUFA supplements increases sleep duration and quality.
ω-3 PUFA supplements help prevent and treat depression and anxiety. EPA is the most effective PUFA in the fight against depression. In people suffering from mental disorders, the level of ω-3 PUFAs is significantly reduced. Supplementation with ω-3 PUFAs has been shown to reduce the incidence of mood swings and relapses in people with schizophrenia and bipolar disorder. Taking ω-3 PUFA supplements may also reduce aggressive behavior [39].
ω-3 PUFAs during pregnancy and in infants after birth
ω-3 PUFAs contribute to normal brain development in the fetus during pregnancy and in infants after birth. PUFA ω-3 fatty acids play a critical role in brain growth and development in young children. 40% of the PUFA DHA is found in the brain and 60% in the retina. It is therefore not surprising that children fed infant formulas supplemented with DHA have better vision than children fed infant formulas without this fatty acid [40, 41].
Getting enough ω-3 PUFAs during pregnancy is associated with numerous health benefits for the baby, including:
- higher level of intelligence;
- better communication and social skills;
- fewer behavioral disorders;
- reducing the risk of developmental delay;
- reducing the risk of developing attention deficit hyperactivity disorder (ADHD), autism and cerebral palsy.
Omega-3s may reduce ADHD symptoms in children
ADHD is a neurobehavioral developmental disorder characterized by inattention, hyperactivity, and impulsivity in children. Some studies have shown that ADHD in children is associated with lower blood levels of ω-3 PUFAs compared to their healthy peers. Moreover, numerous studies have shown that ω-3 PUFA supplementation can actually reduce ADHD symptoms. ω-3 PUFAs help improve alertness and task performance. They also reduce hyperactivity, impulsivity, anxiety and aggression. Recently, researchers have assessed the evidence for the effectiveness of various ADHD treatments. They found that one of the most effective natural treatments for ADHD is fish oil [42].
Noteworthy is the fact that ω-3 PUFA drugs are well tolerated and there are virtually no side effects. It was noted that taking therapeutic doses did not cause serious side effects. However, in certain groups of patients, for example, those with an increased risk of bleeding, ω-3 PUFA preparations should be prescribed with caution.
Optimal ratio of polyunsaturated fatty acids
According to nutritional biochemist William Landes, a National Institutes of Health researcher and world-class expert on the action of essential lipids, ω-3 and ω-6 fatty acids are in constant competition for possession of the enzyme desaturase. This active substance is included in the structure of all cell membranes, maintaining their normal structure. It has a greater affinity for ω-3. But, due to the excess of lipid compounds of the ω-6 type, they combine to a greater extent with this enzyme, which leads to their accumulation in the body. This means that in conditions of deficiency of ω-3 lipids in the food consumed, the human body cannot provide its tissues with these essential fatty acids. Since nature abhors a vacuum, ω-6 compounds take their place. All these data indicate only one thing: food must contain a sufficient amount of fatty acids from the ω-3 PUFA category. This will not only provide the body with vital components, but also protect it from the harmful effects of competitors of these compounds. In case of prolonged deficiency, the body slows down and distorts metabolic processes so much that it becomes very difficult to restore them.
A number of medical studies have shown that an excess of ω-6 PUFA relative to ω-3 PUFA significantly increases the risk of a number of diseases. The diet of modern people includes large quantities of ω-6 PUFAs and a lack of ω-3 PUFAs. These acids should enter the body in a ratio of 3:1, but we get approximately 40:1 from our food. This means that ω-6 PUFA is supplied in excess, and ω-3 PUFA is in deficiency. This leads to an imbalance in metabolic processes and a number of diseases. With an excess of ω-6 PUFAs, a weakening of the body’s protective functions, the immune system, disorders of the cardiovascular system, various types of inflammation and other diseases, including cancer, can occur. Why do Americans, and now not only them, suffer from excess weight: because they were brought up on fast foods and processed foods, in which the content of ω-6 PUFAs and saturated fats is off the charts. Abuse of fatty meat begins irreversible processes that can affect the nervous system, cause infertility, eczema and liver destruction. For children, this threatens to delay growth and overall development.
Scientists from the Division of Health Problems of the National Academy of Sciences (NAS) recommend consuming fatty acids in a ratio of 10:1. This is significantly higher than what is recommended in Sweden (5:1) or Japan (4:1). Perhaps it is due to this indicator that these countries have a relatively low level of heart and vascular diseases, and great progress has been made in the treatment of oncological pathology. At the same time, food should not contain more than 30% of the total calories. Based on this, it is recommended that less than 8% of calories come from PUFAs, with an ω-6/ω-3 ratio of 5:1–3:1. It must also be remembered that due to the participation of PUFAs in the processes of lipid peroxidation, it is advisable to take them simultaneously with antioxidants (tocopherol, etc.). Considering that food sources of ω-3 PUFAs are quite limited and the ratio of ω-6/ω-3 PUFAs in the modern human diet is far from optimal, biologically active food supplements that enrich the diet with PUFAs have now been developed and are available on the market in large quantities [ 43].
Recommendations for use of ω-3 PUFA
Recommendations from the Research Institute of Nutrition of the Russian Federation provide for daily consumption of 0.8–1.6 g of ω-3 fatty acids. More precise dosages depend on many factors and are suggested by foreign recommendations. According to experts, those who want to protect their hearts should eat a variety of oily fish (such as salmon, tuna and mackerel) at least twice a week. Those with heart problems should get 1 g of ω-3 PUFA per day, preferably from fatty fish. About 50 g of fish contain 1 g of ω-3 PUFA. 30 g, or one handful, of walnuts contains about 2.5 g ω-3. This is equal to approximately 100 g of salmon. Flaxseed oil contains alpha-linolenic acid, the most potent plant source of alpha-linolenic acid, which the body can use to produce eicosapentaenoic acid and decosahexaenoic acid. It's much better to choose whole flax seeds, as they also contain 3 grams of fiber per tablespoon as well as beneficial phytoestrogens. Other sources of ω-3 include canola oil, broccoli, cantaloupe, beans, spinach, grape leaves, bok choy, cauliflower and walnuts. Additionally, by consuming more ω-3, you can replace some ω-6 fatty acids from cooking oils (sunflower, soybean, etc.) with a third type of omega fatty acid known as ω-9 (oleic acid). It is a monounsaturated fat found primarily in olive oil.
Are all ω-3 PUFA preparations “equally beneficial”? Based on their origin, ω-3 fatty acids can be divided into two groups: “vegetable” and “marine”. The “sea” type primarily includes DHA. It is mainly found in fish, shrimp, crabs and the tissues of marine animals. The second representative of the “marine” ω-3 acids, DPA, is a substance found only in marine mammals.
Plants, both terrestrial and aquatic, almost do not synthesize “marine” forms of ω-3 polyunsaturated fatty acids and cannot serve as their source.
Plant-based ω-3 fatty acids include ALA and EPA. Plants mainly synthesize ALA. Once in the body of a healthy person, it is completely converted into the active “plant” form of ω-3 fatty acids EPA. When choosing a preparation of ω-3 polyunsaturated fatty acids, you should first of all pay attention to the amount of “marine” forms of DHA and DPA. The content of “plant” forms of EPA and ALA will be sufficient in any preparation. DPC-rich drugs deserve preference because they can more effectively cope with any form of ω-3 polyunsaturated fatty acid deficiency in the body. Required "marine" forms: 500 mg. Thus, it is necessary to compensate for the lack of ω-3 polyunsaturated fatty acids, amounting to at least 200 mg of “marine” forms (DHA, DPA) and 300 mg of “vegetable” forms (EPA and, optionally, ALA).
For effective prevention of atherosclerosis, it is recommended to take 300 mg of type ω-3 polyunsaturated fatty acids per day. In order to prevent malignant tumors, ω-3 type polyunsaturated fatty acids must be taken for a long time - for many years. In prophylactic doses, ω-3 type polyunsaturated fatty acids are well tolerated and have no side or toxic effects [45, 46].
In accordance with the recommendations of the European Association of Perinatal Medicine (EAPM), the daily dose of DHA and EPA for pregnant and lactating women is at least 300 mg, with an acid ratio of 5:1; and for patients with cardiovascular insufficiency, the ratio of EPA to DHA = 1.5:1.
Experts from the US National Institutes of Health have not established recommended amounts of ω-3 fatty acids, with the exception of alpha-linolenic acid. The average daily recommended amounts for alpha-linolenic acid are listed below in grams (Table 1).
For cardiac patients, ω-3 PUFAs are included in the recommendations of the All-Russian Scientific Society of Cardiology (2017) - “you can resort to prescribing polyunsaturated fatty acids in a dose of 2–4 g/day to reduce triglyceride levels”; and recommendations of the American Heart Association (American Heart Association, AHA 2003) (Table 2). The maximum safe amount depends on the sources of ω-3 - no more than 7–8 g per day in the form of fish oil capsules and unlimited in the form of regular food [47].
Based on the available scientific evidence, it is most advisable to prescribe ω-3 polyunsaturated fatty acids for the prevention of breast, colon and prostate cancer in patients at risk. In global oncology, it is planned to conduct long-term interventional clinical trials on the chemoprevention of cancer of these localizations using type ω-3 PUFAs. For auxiliary treatment of cancer patients: increasing the effectiveness of radiation and chemotherapy, during the period of preoperative preparation and rehabilitation, combating cancer cachexia during generalization of the tumor process, ω-3 type polyunsaturated fatty acids should be prescribed in doses of at least 1.8–2 g per day, in maximum doses - 13–18 g per day.
Tolerance of ω-3 PUFA
ω-3 PUFA preparations have proven high safety and good tolerability. No serious side effects have been reported when taken in therapeutic doses. If you have an individual intolerance to fish products, allergic reactions to taking ω-3 PUFAs are possible. Taking ω-3 PUFAs at a dose of up to 3 g per day does not lead to the development of undesirable reactions. However, in certain groups of patients, for example, those suffering from diabetes mellitus, with an increased risk of bleeding or with a high baseline level of low-density lipoproteins, ω-3 PUFAs should be prescribed with caution. Taking ω-3 PUFAs at a dose of more than 3 g per day increases the risk of bleeding, but cases of serious bleeding have not been reported. High doses are more likely to cause nosebleeds or hematuria. Very high intake of ω-3 PUFAs (“Eskimo” intake) increases the risk of hemorrhagic stroke. The reasons for such disorders are the ability of ω-3 PUFAs to reduce thrombus formation, prolong bleeding time and reduce von Willebrand factor.
An overdose of these compounds can be dangerous, which is much more severe than their deficiency. But it is extremely difficult to achieve an excess of polyunsaturated fatty acids in the body, since they accumulate very slowly. Therefore, only systematic and long-term intake of high doses of ω-3 PUFAs can be considered dangerous.
Symptoms of intoxication:
- headache;
- nausea;
- vomit;
- dyspeptic intestinal disorders;
- chest pain;
- heavy periods.
Among the side effects from the gastrointestinal tract, dyspeptic disorders in the form of nausea and, in some cases, diarrhea are possible, mainly against the background of high doses of ω-3 PUFAs. However, these phenomena are unstable and quickly passing. A number of scientific publications recommend cold-water fatty fish as a possible alternative to ω-3 PUFA intake, which is recommended to be consumed at least twice a week. At the same time, one should remember about the possible contamination of fish with potentially hazardous products - such as heavy metal salts, dioxins, methylmercury and polychlorinated biphenyls. Ingestion of heavy metal salts can lead to dysfunction of the central nervous system and other disorders. In addition, unrefined fish oil may contain pesticides. Therefore, for the prevention and treatment of cardiovascular diseases, it is recommended to use highly purified ω-3 PUFAs.
Literature
- Burr ML Lessons from the story of n-3 fatty acids // Am J Clin Nutr. 2000; 71(1):397S–398S.
- Kromann N., Green A. Epidemiological studies in the Upernavik district, Greenland. Incidence of some chronic diseases 1950–1974 // Acta Med Scand. 1980; 208:401–406.
- Kromhout D., Yasuda S., Geleijnse JM, Shimokawa H. Fish oil and omega-3 fatty acids in cardiovascular disease: do they really work? // Eur Heart J. 2012, Feb; 33(4):436–443.
- Sinclair HM The diet of Canadian Eskimos // Proc Nutr Soc. 1953; 12: 69–82.
- Bang HO, Dyerberg J., Sinclair HM The composition of the Eskimo food in north western Greenland // Am J Clin Nutr. 1980; 33:2657–2661.
- Lee KW, Lip GY The role of omega-3 fatty acids in the secondary prevention of cardiovascular disease // QJM. 2003, Jul; 96(7):465–480.
- Schuchardt J., Hahn A. Bioavailability of long-chain omega-3 fatty acids. Prostaglandins, Leukotrienes and Essential Fatty Acids // PLEFA. 2013; 89 (1): 1–8.
- Kris-Etherton PM, Harris WS, Appel LJ AHA Nutrition Committee. Omega-3 fatty acids and cardiovascular disease: New recommendations from the American Heart Association. Arterioscler // Thromb. Vasc. Biol. 2003; 23 (2): 151–152.
- Titova V. N., Lisitsyn D. M. Fatty acids. Physical chemistry, biology and medicine. M.: Publishing house. Triad, 2006. 670 p.
- Pristrom M. S., Semenenkov I. I., Olikhver Yu. A. Omega-3 polyunsaturated fatty acids: mechanisms of action, evidence of benefit and new prospects for use in clinical practice // Medical news. 2017; 3:13–16.
- Shimokawa H. Beneficial effects of eicosapentaenoic acid on endothelial vasodilator functions in animals and humans. In: Hamazaki T., Okuyama H., eds. Fatty Acids and Lipids - New Findings, World Review of Nutrition and Dietics. 2001; 88: 100–108.
- Singh RB, Niaz MA, Sharma JP, Kumar R., Rastogi V., Moshiri M. Randomized, double-blind, placebo-controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: the Indian experiment of infarct survival -4 // Send to Cardiovasc Drugs Ther. 1997, July; 11 (3): 485–491.
- Hopper L., Ness A., Higgins JP, Moore T., Ebrahim S. GISSI-Prevenzione trial // Lancet. 1999, Oct 30; 354(9189):1557.
- Marchioli R., Valagussa F. The results of the GISSI-Prevenzione trial in the general framework of secondary prevention // Eur Heart J. 2000, Jun; 21 (12): 949–952.
- Marchioli R., Marfisi RM, Borrelli G., Chieffo C., Franzosi MG, Levantesi G., Maggioni AP, Nicolosi GL, Scarano M., Silletta MG, Schweiger C., Tavazzi L., Tognoni G. Efficacy of n- 3 polyunsaturated fatty acids according to clinical characteristics of patients with recent myocardial infarction: insights from the GISSI-Prevenzione trial // J Cardiovasc Med (Hagerstown). 2007, Sep; 8(1):S34–37.
- Duda MK, O'Shea KM, Stanley WC Omega-3 polyunsaturated fatty acid supplementation for the treatment of heart failure: mechanisms and clinical potential // Cardiovasc Res. 2009; 84: 33–41.
- Leaf A. Dietary prevention of coronary heart disease: the Lyon Diet Heart Study // Circulation. 1999, Feb 16; 99(6):733–735.
- Vasiliev A.P., Streltsova N.N. Omega-3 fatty acids in cardiological practice // Consilium Medicum. 2017; 10: 96–104.
- Catapano A. et al. 2021 ESC/EAS Guidelines for the Management of Dyslipidaemias // European Heart Journal. 2016; 37(39):2999–3058.
- Nakamura N., Hamazaki T., Ohta M., Okuda K., Urakaze M., Sawazaki S., Yamazaki K., Satoh A., Temaru R., Ishikura Y., Takata M., Kishida M., Kobayashi M. Joint effects of HMG-CoA reductase inhibitors and eicosapentaenoic acids on serum lipid profile and plasma fatty acid concentrations in patients with hyperlipidemia // Int J Clin Lab Res. 1999; 29:22–25.
- Sampath H., Ntambi JM Polyunsaturated fatty acid regulation of genes of lipid metabolism // Annu Rev Nutr. 2005; 25: 317–340.
- Oi K., Shimokawa H., Hiroki J., Uwatoku T., Abe K., Matsumoto Y., Nakajima Y., Nakajima K., Takeichi S., Takeshita A. Remnant lipoproteins from patients with sudden cardiac death enhance coronary vasospastic activity through upregulation of Rho-kinase // Arterioscler Thromb Vasc Biol. 2004; 24:918–922.
- Rudenko V. G. Relevance of the use of omega-3 PUFAs in clinical practice // Newspaper “News of Medicine and Pharmacy”. 2010, 9 (325).
- Colussi G., Soardo G., Fagotto V., Sechi LA Omega-3 polyunsaturated fatty acids in the treatment of non-alcoholic fatty liver disease: are they so good? // J. Metabolic. Synd. 2017; 6: e120.
- De Caterina R., Madonna R., Bertolotto A., Schmidt EB ω-3 Fatty Acids in the Treatment of Diabetic Patients Biological rationale and clinical data // Diabetes Care. 2007, Apr; 30(4):1012–1026.
- Denisenko Yu. K., Novgorodtseva T. P., Zhukova N. V., Antonyuk M. V., Lobanova E. G., Kalinina E. P. Association of fatty acid metabolism with a systemic inflammatory response in chronic respiratory diseases // Biomedical chemistry. 2016; 3: 341–347.
- Henderson NC, Mackinnon AC, Farmworth SL et al. Galectin-3 regulates myofibrolast activation and hepatic fibrosis // Proc Natl Acad Sci USA. 2006; 103(13):5060–5065.
- Colussi G., Soardo G., Fagotto V., Sechi LA Omega-3 polyunsaturated fatty acids in the treatment of non-alcoholic fatty liver disease: are they so good? // J. Metabolic. Synd. 2017; 6: e120.
- Yates CM, Calder PC, Ed. Rainger G. Pharmacology and therapeutics of omega-3 polyunsaturated fatty acids in chronic inflammatory disease // Pharmacol. Ther. 2014; 141:272–282.
- Kremer JM, Lawrence DA, Petrillo GF, Litts LL, Mullaly PM, Rynes RI, Stocker RP, Parhami N, Greenstein NS, Fuchs BR et al. Effects of high-dose fish oil on rheumatoid arthritis after stopping nonsteroidal antiinflammatory drugs. Clinical and immune correlates // Arthritis. Rheum. 1995; 38(8):1107–1114.
- De Winther MP, Kanters E., Kraal G., Hofker MH NF-kB signaling in atherogenesis // Arterioscler Thromb Vasc Biol. 2005; 25:904–914.
- Kulina E. V., Smolina Yu. A., Osmanov I. M., Sukhorukov V. S., Mamedov I. S., Zolkina I. V. The role of omega-3 fatty acids in progressive kidney diseases // Russian Bulletin of Perinatology and pediatrics. 2012; 4:81–86.
- Kaizer L., Boyd NF, Krinkov V. Fish consumption and breast cancer risk: an ecological study/\Nutr. Cancer. 1989; 12:61–68.
- Bjorneboe A., Soyland E., Bjorneboe GE Effect of dietary supplementation licosapentaenoic acid in the treatment of atopic dermatitis // Br. J. Dermatol. 1987; 117:463–469.
- Golousenko I. Yu. Background treatment of atopic dermatitis with essential fatty acids Omega-3 and Omega-6 // Bulletin of Dermatology and Venereology. 2004; 3:58–59.
- Gupta AK, Ellis CN, Tellnes DC Double-blind, placebo-controlled study to evaluate the efficacy of fish oil and low-dose UVB in the treatment of psoriasis // Br. J. Dermatol. 1989; 120:801–807.
- Gavrisyuk V.K. Application of Omega-3 polyunsaturated fatty acids in medicine // Ukr. pulmonary magazine 2001; 3:5–10.
- Kokjohn TA, Roher AE Amyloid precursor protein transgenic mouse models and Alzheimer's disease: understanding the paradigms, limitations, and contributions // Alzheimers Dement. 2009; 5:340–347.
- Stoll AL, Locke CA, Marangel LB, Severus WE Omega-3 fatty acids and bipolar disorder: a review // Prostaglandins. Leukot. Essent. Fatty. Acids. 1999; 60: 329–337.
- Koletzko B., Agostoni C., Carlson SE, Clandinin T., Hornstra G., Neuringer M., Uauy R., Yamashiro Y., Willatts P. Long chain polyunsaturated fatty acids (LC-PUFA) and perinatal development // Acta Paediatr. 2001; 90:460–464.
- Gromova O. A., Torshin I. Yu., Sukhikh G. T., Baranov A. A., Prilepskaya V. N., Tetruashvili N. K., Uvarova E. V. The roles of various forms of omega-3 PUFAs in obstetrics and neonatology. Publication within the framework of the national project “Health”. M., 2009. 64 p.
- Bloch MH, Qawasmi A. Omega-3 fatty acid supplementation for the treatment of children with attention-deficit/hyperactivity disorder symptomatology: systematic review and meta-analysis // J Am Acad Child Adolesc Psychiatry. 2011, Oct; 50 (10): 991-10-00.
- Plotnikova E. Yu., Sukhikh A. S. Lipids: hepatoprotectors, points of application, pharmacological effects // Consilium Medicum. 2016; 1:5–12.
- Kling D.F., Johnson J., Rooney M., Davidson M. Omega-3 Free Fatty Acids Demonstrate More Than 4-Fold Greater Bioavailability for EPA and DHA Compared with Omega-3-acid Ethyl Esters in Conjunction with a Low-Fat Diet: The ECLIPSE Study // Journal of Clinical Lipidology. 2011, May–June; 5 (3): 231.
- WHO, URL: https://www.earlynutrition.org/perilip/PeriLipRecommendations.html.
- Diagnosis and correction of lipid metabolism disorders for the prevention and treatment of atherosclerosis. Russian recommendations VI revision. M., 2021. URL: https://webmed.irkutsk.ru/doc/pdf/noa.pdf.
E. Yu. Plotnikova1, Doctor of Medical Sciences, Professor M. N. Sinkova, Candidate of Medical Sciences L. K. Isakov, Candidate of Medical Sciences
Federal State Budgetary Educational Institution of Higher Education Kemerovo State Medical University, Ministry of Health of the Russian Federation, Kemerovo
1 Contact information
The role of omega-3 unsaturated acids in the prevention and treatment of various diseases (part 2) / E. Yu. Plotnikova, M. N. Sinkova, L. K. Isakov For citation: Attending physician No. 8/2018; Page numbers in the issue: 56-61 Tags: polyunsaturated lipids, ratio, nutrition, cardiovascular diseases, prevention
Non-surgical treatment of acute and chronic hemorrhoids
G
Emorrhoids are one of the most common human diseases.
Although there are no exact statistics on this matter, there is every reason to believe that up to 80% of the adult population suffers from hemorrhoids
. Patients with this disease often seek help not only from coloproctologists, but also from specialists related to the treatment of diseases of the gastrointestinal tract, i.e. internists and gastroenterologists. The ability to correctly diagnose and choose adequate treatment tactics is the main task of a doctor.
Etiology
In the light of modern concepts, hemorrhoids are based on the pathology of cavernous vascular plexuses that arise during normal embryogenesis in the submucosal layer of the distal part of the rectum. There are two theories explaining the development of hemorrhoids: “mechanical” and “hemodynamic”.
According to the “mechanical” theory, hemorrhoids are formed as a result of distal movement of the anal ridges. The latter are a normal anatomical structure and play an important role in retaining the contents of the rectum. The venous plexuses, contained in their submucosal layer, are normally fixed by connective tissue fibers of the longitudinal muscle, and below by the ligament of Parks. As intra-abdominal pressure increases, the ridges move distally. With prolonged straining and other unfavorable conditions, accelerated natural wear of the fixing apparatus occurs. Fiber rupture, degenerative and dystrophic changes are observed. Hemorrhoids increase in size and fall out of the anal canal. According to the “hemodynamic” theory, the formation of nodes is facilitated by stagnation of venous blood, which occurs as a result of mechanical obstacles (hard feces, its constant presence in the ampulla of the rectum) and the lack of relaxation of the internal sphincter during defecation. The reverse flow of venous blood is aggravated by the opening of arteriovenous shunts and spasm of precapillary arterioles. Apparently, both mechanisms are equally involved in the genesis of hemorrhoids. However, venous congestion more often causes thrombosis of nodes, and increased arterial blood flow and the opening of shunts lead to bleeding, varicose veins and inflammatory changes in the rectal mucosa. Predisposing or resolving factors include insufficient dietary fiber, constipation and straining during bowel movements, sedentary lifestyle, hot baths, heavy lifting, pregnancy and childbirth. Loose stools, abuse of laxatives, enemas, excessive anal hygiene, and spicy foods also have a negative impact.
Clinic
Characteristic manifestations of hemorrhoids are bleeding from the anus and prolapse of hemorrhoids.
.
The blood is bright red, without clots. The patient notices its presence most often in the toilet. It is released in drops or streams during bowel movements. Blood is never mixed with feces, as is the case with inflammatory diseases of the colon, and is absent from toilet paper, which is typical for an anal fissure. When hemorrhoids prolapse, blood may stain your underwear. Very rarely, the blood may become dark in color and appear in clots. This occurs due to the accumulation of blood in the ampulla of the rectum and its release during subsequent bowel movements. Pain and discomfort are usually associated with thrombosis of nodes or anal fissure. Anal itching
is a symptom that occurs for many reasons.
These include insufficient hygiene after defecation, fecal contamination of linen, prolapse of nodes with or without mucous discharge. Typically, such a patient complains that after defecation he has to repeatedly use toilet paper in order to properly clean the anus. Sometimes the patient experiences perianal edema due to the filling of the external venous plexus with blood or thrombosis of the external hemorrhoids. Since internal hemorrhoids are covered with columnar epithelium, trauma leads to inflammation and copious secretion of mucus
. The predominance of certain symptoms in the clinical picture of the disease will dictate the choice of appropriate drugs for local treatment.
Clinically, hemorrhoids manifest themselves in two main syndromes:
chronic and acute. These syndromes are phases of the same process. For the first stage of chronic hemorrhoids, a characteristic sign is the discharge of blood from the anal canal without prolapse of hemorrhoids. The second stage is accompanied by the loss of nodes, which are independently retracted into the anal canal. A distinctive feature of the third stage is the need for their manual reduction. Prolapse of nodes occurs not only during bowel movements, but also during heavy lifting and coughing. The fourth stage is characterized by constant loss of nodes and the impossibility of their reduction into the anal canal. With each stage, the symptoms become more diverse. By this time, the connective tissue frame of the anal ridges is significantly damaged and cannot be restored. This classification makes it possible in practice to select a treatment method. The basis for the development of an acute process is thrombosis of hemorrhoids - internal or external.
Treatment
Indications for conservative treatment are the initial stages of chronic hemorrhoids and the acute uncomplicated course of the disease. At the first stage, preference is given to drug treatment or infrared photocoagulation. In the second stage, drug treatment is still acceptable, but ligation with latex rings is considered an alternative. It is also acceptable in the third stage, but in the fourth stage the only adequate treatment method is hemorrhoidectomy. It should be noted that currently minimally invasive methods of treating hemorrhoids have become widespread. They provide a positive effect in 88% of cases, are associated with a low risk of complications, are painless and can be performed on an outpatient basis without loss of ability to work.
Conservative treatment of hemorrhoids
Includes general measures in the form of diet, careful personal hygiene, physical activity, taking analgesics, non-steroidal anti-inflammatory drugs, systemic venotonics, as well as local treatment with combination drugs.
Regardless of the type of hemorrhoids, special attention should be paid to simple hygiene practices
. These include refusing to use toilet paper, using baths or showers at a comfortable temperature with washing both the perianal skin and the anal canal itself with plain water without soap or other detergents. Eliminating fecal contamination reduces inflammation and itching, and warm water relieves pain associated with sphincter spasm.
Some types of exercise
that help eliminate venous stasis, for example, swimming or gymnastics.
It is very important to regulate stool consistency and frequency
. Diarrhea and constipation are equally unacceptable. In case of stool retention and strained bowel movements, irritating laxatives should be avoided. Patients are recommended to increase their intake of plant fiber (vegetables, fruits) and fluids. Additionally, wheat bran, microcrystalline cellulose or other hydrophilic colloids are included - seaweed, flaxseed. It is recommended to take preparations from plantain seeds or macrogol 4000. The choice is quite individual. These drugs are useful both during exacerbation of hemorrhoids, and in preparation for surgery, and in the postoperative period. In controlled studies, plantain seeds - Plantago ovata - have been shown to effectively reduce the incidence of bleeding and other symptoms of stage 1 and 2 hemorrhoids, but have no significant effect on the size and blood supply of hemorrhoids (Perez-Miranda et al., 1996). Patients with diarrhea are prescribed astringents, loperamide, hydrophilic colloids in combination with oral hydration. Drinking alcohol, spicy food, tea or coffee is prohibited.
An important element of the treatment program is the use of phlebotropic drugs
. This should include preparations from horse chestnut fruits, troxerutin, rutoside, escin and others. Purified micronized diosmin has been better tested in clinical trials, which effectively reduces the clinical manifestations of acute and chronic hemorrhoids, and also prevents its exacerbations (Godegere, 1994; Meyer, 1994). Drugs in this group increase the tone of the veins and the speed of lymph flow, improve microcirculation, and reduce capillary permeability caused by ischemia and inflammatory mediators. It should be noted that micronized diosmin can be safely used for acute hemorrhoids in pregnant women (Buckshee et al., 1997), in whom outpatient surgical treatment is contraindicated. The drug is prescribed 4-6 capsules for 7 days, but treatment can be prolonged - 2 capsules per day for many months.
multicomponent ointments and suppositories are widely used.
. Almost all of them include anti-inflammatory, antimicrobial, sclerosing, anticoagulant agents, anesthetics, venotonics and reparants in various combinations. The optimal composition of agents for topical treatment of hemorrhoids has not been precisely established. It remains not entirely clear whether the presence of anticoagulants, antibiotics or anesthetics in the composition has a significant impact on the therapeutic effectiveness, whether they potentiate each other, whether they are necessary and, therefore, mandatory components of therapeutic drugs. In our study (unpublished data), we compared the therapeutic effectiveness of well-known antihemorrhoidal ointments - aurobin, proctosedyl and Hepatrombin G in identical groups of patients with acute hemorrhoids of the first and second stages. The choice of these drugs was determined by the fact that each of them contained a different component. Thus, Hepatrombin G and proctosedyl contained heparin, proctosedyl and aurobin contained an antimicrobial agent, Hepatrombin G and aurobin contained an anesthetic. Thus, Hepatrombin G should be used for conditions such as:
- external and internal hemorrhoids;
— thrombophlebitis of hemorrhoidal veins of the anus;
- fistulas, eczema and itching in the anus;
- anal fissures;
— preparation for surgical intervention in the anorectal area;
- as part of combination therapy for thrombosed and operated hemorrhoids.
The ointment can be applied to the affected areas or inserted into the rectum using a screw-on tip.
When using the drug in recommended doses, no toxic effects are observed.
As the results of the study showed, Hepatrombin G reduced the frequency of bleeding from 80% to 5% within a week.
. Pain and inflammatory manifestations in the nodes and anal canal quickly subsided, and thrombosis of the nodes decreased. Excellent and good results according to the survey of doctors and patients were 90% and 85%, respectively.
If we evaluate the efficiency and cost indicators
, then
undeniable advantages were on the side of Gepatrombin
G.
The conducted study emphasizes the need for a conscious choice of certain agents for local therapy, taking into account their composition and clinical manifestations in a particular patient. In case of thrombosis of external nodes and prolapse of internal nodes, preference should be given to ointments. Suppositories are indicated only for hemorrhoids in the initial stages. They should not be pushed into the ampulla of the rectum, but held by hand until they melt completely into the anal canal. For pain, drugs with lidocaine are prescribed, for predominant inflammatory changes - with corticosteroids (Hepatrombin G, aurobin), for thrombosis - with heparin (Proctosedyl, Hepatrombin G), for swelling and enlargement of nodes - with venotonics. In patients with erosive sphincteritis and anal itching, in order to accelerate reparative processes, drugs that have an immunostimulating effect and improve tissue regeneration are used. Adverse reactions occur rarely. However, you should refrain from long-term use of corticosteroid ointments due to the dryness and microcracks they cause in the anal canal, with infectious diseases of the perianal skin, and during pregnancy. Ointments and suppositories are administered 4-6 times a day during the acute period of the disease for 2-3 weeks.
Two days before surgery and for 2 weeks after it, lactulose is prescribed (20 ml twice a day); administer suppositories with diclofenac 50 mg 3 times a day, as well as 0.2% nitroglycerin ointment; prescribe metronidazole 400 mg 3 times a day for a week; paracetamol and dehydrocodeine as indicated (Carapeti & Phillips, 2000).
Thus, the choice of treatment method for hemorrhoids is determined by the stage of the disease, the severity and nature of the symptoms.
Treatment is carried out as a complex of general measures of medicinal and non-medicinal nature. In this case, the option of modern therapy must necessarily include a combination of systemic venotonics, for example, micronized diosmin, and local treatment agents, for example, Hepatrombin G. The same measures are acceptable before preparing for ligation of nodes with latex rings and hemorrhoidectomy. It is necessary to realistically imagine the purpose and possibilities of conservative treatment, and not try to treat conservatively when the only way to relieve the patient from suffering is surgery. References:
1. Buckshee K., Takkar D., Aggarwal N. Micronized flavonoid therapy in internal hemorrhoids of pregnancy. Int J Gynaecol Obstet, 1997, 57, 145-151.
2. Carapeti EA, Phillips RKS Treatment of hemorrhoids. In: J.Beynon, NDCarr (eds): Recent advances in coloproctology, Springer-Verlag London Limited, 2000, 155-166.
3. Godegere P. Daflon 500 mg in the treatment of hemorrhoidal disease: a demonstrated efficacy in comparison with placebo. Angiology, 1994, 45, 574-578.
4. Meyer OC Safety and safety of Daflon 500 mg in venous insufficiency and in hemorrhoidal disease. Angiology, 1994, 45, 579-584.
5. Orkin B., Schwartz AM, Orkin M. Hemorrhoids: what the dermatologist knows. J Am Acad Dermatol 1999, 41, 449-456.
6. Perez-Miranda M., Gomez-Cenelilla A., Lean-Colombo T. et al. Effect of fiber supplements of internal bleeding hemorrhoids. Hepato-Gastroenterology, 1996, 43, 1504-1507.