Tendon[edit | edit code]
Tendon
is part of the non-contractile connective tissue of skeletal muscles. With the help of one or more tendons, muscles are connected to the bone skeleton or cartilage. They transmit the movement caused by muscle contraction to the bones or, conversely, the force of gravity acting on the axial skeleton to the muscles.
Tendon structure[edit | edit code]
Rice.
1.9. The structure of collagen fiber There are various forms of tendon.
- Long thin tendons
- for example, in the muscles of the hand. They provide free mobility of the distal parts of the upper limb, which short tendons cannot provide.
- Short tendons
- for example, in the deltoid and pectoralis major muscles. These muscles macroscopically have barely visible tendons. In this case, they talk about the beginning of the muscle and the place of attachment.
- Flat tendons
- the so-called
aponeuroses
, have muscles that form the walls of the body.
The tendon consists of 70-80% fibrous connective tissue. The remaining components of the matrix are the main substance (dermatan sulfate, hyaluronic acid and chondroitin sulfate, about 0.5-1%), non-collagenous proteins (fibronectin and tenascin) and cells - tenocytes (tendon tissue cells), fibroblasts, synovial cells (connective tissue membrane cells) and chondroblasts or chondrocytes (cartilage cells). Under the tendon fibers
refers to the majority (95%) of wavy type I collagen fibers, which impart mechanical strength to the tendon.
In addition, the tendon contains elastic fibers (about 1%). Collagen fibers
consist of collagen molecules, which are three protein chains twisted relative to each other (triple helix, each helix has the shape of an a-helix).
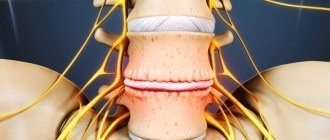
A group of fibers join together in the interstitium and form a so-called collagen microfibril. Numerous microfibrils, spirally twisting relative to each other, form a collagen fibril, from which, in turn, collagen fiber is formed (Fig. 1.9). rice.
1.10. Arrangement of collagen fibers in the tendon Collagen fibers have a wavy shape and are located in both long and short tendons parallel to each other. In the aponeuroses, bundles of collagen fibers intersect and look like a lattice.
Thanks to the spiral structure of collagen fibers and their wave-like course, the tendon can stretch by 5% of its length and optimally distribute the forces acting on it. Tensile loads during muscle contractions or passive muscle stretching lead first to tension in the collagen fibers, and then to uniform stretching of the collagen. This mechanism ensures the transfer of applied force between muscle and tendon. The spiral structure gives the tendon (even after straightening the wavy fibers) a very high tensile strength - about 500-1000 kg/cm2. The tendon is very strong and can withstand greater loads than steel cable of the same thickness (van den Berg, 1999). Elastic fibers located between the bundles of collagen fibers (Fig. 1.10) absorb loads and return the tendon fibers to their wave-like shape after they cease. Groups of collagen fibers are united into bundles by a thin layer of unformed connective tissue - endotenonium
.
The bundles, in turn, are surrounded by connective tissue internal peritenonium
and form large (secondary) bundles of fibers.
The external peritenonium unites large bundles into a tendon. All of these connective tissue layers are rich in blood vessels and nerves. The external peritenonium is covered with an additional layer - paratenonium
- which anatomically separates the tendon from the surrounding tissues. The paratenonium is formed by loose, fibrous, well-supplied connective tissue and, due to the presence of synovial cells, can produce fluid similar to synovial fluid. This reduces friction as the tendon glides and prevents loss of muscle contraction force.
The connective tissue sheaths of tendons pass into similar sheaths of muscles without a visible border. Between the bundles of tendon fibers are cells (tenocytes), also called pterygoid cells because of their thin, long cytoplasmic projections, with the help of which they connect with neighboring cells. Tenocytes synthesize collagen and elastic fibers, as well as a small amount of the main matrix substance. The function of the contractile actin and myosin filaments found in them is still completely unknown. Cells of connective tissue sheaths of tendons are represented by fibroblasts
.
In addition, tendon tissue contains non-contractile proteins
(fibronectin and tenascin), which connect the layers of connective tissue and perform a stabilizing function.
With age, the proliferative capabilities of tendon cells decrease. The number of cells and the production of ground substances decrease, and the number of elastic and collagen fibers decreases. As a result, there is an age-related decrease in tensile strength and tensile extensibility of the tendons by approximately 20%. The maximum load capacity of the tendon is also reduced (Weineck, 2003). Only with constant irritation (tension and relaxation) is it possible to maintain the strength of the constantly renewed tendon. With appropriate training, tendon strength can even be increased. Adequate irritation of tendon tissue leads to an increase in the activity of tenocytes and the synthesis of collagen and ground substance - the number of collagen fibrils and fibers increases and the diameter of the tendon increases (Oakes, 1998). Too much non-physiological stress, such as in professional sports, can lead to the replacement of thick collagen fibers with thin ones, resulting in the formation of a more stable but less elastic tendon (van den Berg, 1999). Too high non-physiological loads can often lead to partial ossification of the tendon due to the fact that tendon cells, like osteocytes (bone cells), can react with increased calcification. Tendon strength decreases with ossification and the risk of tendon rupture increases. When the tendon is immobilized or underloaded (for example, when the muscle is inactive), the number of collagen and non-collagen fibers decreases (see “Tip”).
Tendons differ not only in shape (see above), but also in structure
depending on the tissue surrounding them.
Some tendons are composed entirely of tendon tissue. In areas of particularly high stress (for example, in the area of bending bones), a zone of fibrocartilage forms in the thickness of the tendon (
for example, in the biceps brachii tendon in the radius region). If tendons slide over other tissues, primarily bones, tendon sheaths (the tendon bursa of the triceps brachii muscle between its tendon and the olecranon process) are formed to reduce friction.
Advice
:After immobilization for 4 weeks. tendon strength is reduced by approximately 20% (Cunnings and Tillmann, 1992; Tabary, 1972). After 12 weeks During immobilization, the loss of collagen fibers in the tendon reaches 16% (van den Berg, 1999). In addition, due to insufficient mechanical irritation, the organization of collagen fibers is disrupted, which increases the likelihood of injury even with light loads. The previous strength is achieved only after 4-12 months. (Oakes, 1998).
Tendon sheaths[edit | edit code]
rice.
1.11. The structure of the tendon sheath Tendon sheaths are sheaths that surround the tendons and facilitate their sliding. Their function is to reduce friction and pressure of surrounding tissues. They are located in places where the tendon bends or puts pressure on the underlying bones and ligaments. For example, there are a large number of tendon sheaths on the foot and hand. The inner layer of the two-layer connective tissue membrane ( epithenonium
) instead of the external peritenonium surrounds the tendon, and the outer layer is formed
by the external peritenonium
. The outer leaf is additionally reinforced with a paratenonium derivative - a fibrous membrane. The fibrous membrane extends throughout the tendon and is attached to the underlying bone at the sides. In the area of the tendon sheaths of the fingers and toes, dense connective tissue crosswise strands are additionally formed. The epitenonium and peritenium are covered by a synovial membrane, which can secrete fluid similar to synovial membrane. This reduces friction between the sheets and facilitates the sliding of the tendon. Both layers join at the end of the tendon sheath, forming a closed sac. The tendon sheath is attached to the underlying tissues with the help of the so-called mesotenium, through which blood vessels and nerves approach it (Fig. 1.11).
synovial bursae can also reduce friction of surrounding tissues.
.
Synovial bursae[edit | edit code]
Synovial bursae (bursae synoviales)
They are sac-like formations filled with synovial fluid (they are compared to cushions of water).
Like tendon sheaths, their shell consists of two layers: the outer (connective tissue fibrous layer
) and the inner (
synovial layer
).
The latter consists of synovial cells capable of producing synovial fluid, which reduces the friction of these two layers relative to each other. In addition, the bursae redistribute the pressure exerted on them and reduce friction when tissues shift. They are often located between tendons and bones, at the origin and insertion of muscles ( subtendinous bursae
), between fascia (
subfascial bursae
), ligaments (
interligamentous bursae
) and between subcutaneous tissue and underlying tissues (
subcutaneous bursae
). Near the joints, they often merge with each other and communicate with the cavity of the joints (for example, the suprapatellar bursa).
Blood supply and innervation of tendons[edit | edit code]
Tendon tissue, including its connective tissue components, is well supplied with blood and innervated. Vessels and nerves approach it through connective tissue membranes (endotenonium, peri-tenonium, paratenonium) and are located parallel to the tendon fibers. In addition to extratendinous vessels, there are also intratendinous vessels and nerves that anastomose with each other. In the area of the bone-tendon junction they connect with the vessels and nerves of the periosteum and bone. Anastomoses are also formed with the vascular and nervous structures of the tendon sheaths. At the site of fibrocartilage formation in the tendon, tissue nutrition is performed avascularly, i.e. through the processes of osmosis and diffusion. Tendons receive both autonomic and sensory innervation (for example, through Golgi receptors).
If you play sports, how to protect yourself from injury
Always remember that even a little prevention can help prevent injury from occurring. The easiest way to avoid damage is to be careful. This does not mean that you need to eliminate physical activity. On the contrary, the body needs to be trained, gradually increasing the load. It is especially important to exercise regularly at a young age, when the body is still developing.
In addition, follow the following recommendations of the doctors of the SANMEDEXPERT clinic:
- Prevention of ankle injuries. For sports, choose comfortable, preferably high, shoes. The presence of lacing will allow you to secure your ankle well. Say a categorical “No!” to worn-out shoes, since wearing such shoes increases the risk of injury several times.
- General prevention. When performing special exercises that involve a large load on the ligaments and tendons, use special clamps and elastic bandages. Be sure to warm up before any physical activity. Don't push yourself to the point of exhaustion by playing sports. Do not run on uneven surfaces or terrain that is unfamiliar to you. A balanced diet is also of great importance.
If you receive injuries, contact traumatologists and orthopedists at the SANMEDEXPERT clinic. Modern equipment allows for quick and accurate diagnostics and provides patients with fast and effective medical care.