Throughout our lives, we put stress on our joints every day. They are the ones who suffer primarily from various injuries and pathologies of bone tissue. Timely prevented destruction of joints, the treatment of which can be extremely difficult, helps to maintain mobility for many years. To do this, it is extremely important to carefully monitor the condition of the cartilage and consult a doctor if symptoms appear that impede movement.
It is important to understand what signs indicate the approach of pathology and can significantly damage the musculoskeletal system. In this article we will look at all the factors that can negatively affect the function of moving joints. You will also find several tips to help you effectively deal with diseases and unpleasant pathologies.
What is coxarthrosis
Arthrosis of the hip joint or coxarthrosis is a chronic, slowly progressive degenerative disease, accompanied by the destruction of cartilage and bone tissue of the joint, the growth of bone osteophytes that deform the joint, as well as the involvement of periarticular tissues in the pathological process. All this gradually leads to complete loss of leg function and disability. Women suffer from this type of arthrosis more often.
For a long time, the disease was considered age-related, but it has now been proven that in many people this pathology of the legs begins to develop after 20 years, and sometimes in childhood, remaining asymptomatic for a long time, appearing after 40 - 50 years. In terms of incidence, coxarthrosis is second only to arthrosis of the knee joint. But in terms of the duration of periods of incapacity, it is much ahead of it, since it is more severe. Coxarthrosis of both joints and one joint develop equally often.
In some cases, the disease is detected in late stages, but this is not a death sentence: conservative and surgical treatment methods have been developed for any stage. The code for coxarthrosis according to ICD 10 (International Classification of Diseases, 10th revision) is M16.
Treatment of arthrosis in remission
During the period of remission, therapy for arthrosis is aimed at preventing exacerbation and restoring the motor ability of the joint. Drug treatment at this stage is reduced to a minimum. As a rule, the patient continues the course of chondroprotectors and, if necessary, takes non-steroidal anti-inflammatory drugs. For better tissue trophism, vitamins, especially B12 and D, can be prescribed.
NANOPLAST forte in remission is used to reduce pain and prevent the development of inflammation. Since the patch itself improves local lymph and blood circulation, improves venous outflow and tissue trophism, reduces swelling and relaxes muscles, its use helps reduce the use of painkillers, and sometimes completely abandon them. In addition, NANOPLAST forte is an excellent prophylactic agent, as it helps to enhance natural regenerative processes in joint tissues and reduces the risk of developing an inflammatory process.
Causes and features of the development of arthrosis of the hip joint
Osteoarthritis of the hip joint (HJ) is actually a group of diseases that have different origins, but are similar in the mechanism of development of the pathological process, changes in joint tissues and main symptoms. The disease can be primary (the causes of this disease are not fully established) and secondary.
Reasons for the development of secondary coxarthrosis:
- Exogenous – factors of external influence. This is hard physical labor, sports, accompanied by increased stress on the legs and microtraumas. This also includes the consequences of macrotraumas - fractures, dislocations, ligament ruptures.
- Internal causes are various common diseases, one of the manifestations of which is coxarthrosis. Such diseases include chronic infectious-inflammatory and autoimmune (rheumatoid, reactive, psoriatic arthritis), as well as metabolic (gout) pathological joint processes. Over time, along with inflammation in the joints of the legs, degenerative-dystrophic processes develop - arthrosis-arthritis (osteoarthrosis).
- Congenital diseases - dysplasia (impaired joint formation) and osteochondropathy (malnutrition of the joint with subsequent bone necrosis) can also result in coxarthrosis, for example, aseptic necrosis of the femoral head (Perthes disease) - the causes of these diseases have not been precisely established.
- Genetic predisposition – hereditary structural features of the hip joint and genetic pathology of connective tissue.
- Age-related physiological processes accompanied by hormonal changes, including a decrease in the content of female sex hormones (women get sick more often than men), excess body weight, and less physical activity.
Under the influence of the listed factors (often several at once), changes gradually occur in the articular cavity at the cellular level: the metabolism in the cells of cartilage tissue changes, the processes of destruction in them begin to prevail over the processes of synthesis. The volume of joint fluid that nourishes the cartilage tissue decreases. The joint space narrows.
Damage to the hip joint due to coxarthrosis
This leads to a gradual thinning and then cracking of the articular hyaline cartilage and the growth of connective tissue in the subchondral zone of the bone. The bones along the edges of the articular surfaces begin to grow (protective reaction), forming growths (osteophytes) and deforming the leg. Degenerative-dystrophic processes occur in the articular cavity, periodically aggravated by aseptic (without infection) inflammation. Over time, the articular surfaces partially grow together due to the proliferation of connective tissue, which prevents the leg from bending, straightening and rotating inward. The surrounding muscles are constantly under tension, protecting the joint from additional injury and at the same time increasing pain, which leads over time to their atrophy (decrease in volume).
Restriction and pain of movements contribute to the fact that the patient takes a forced position when walking with a displacement of the pelvis, the head of the femur and the axis of movement in the leg. This leads to changes in the knee and ankle, and the development of flat feet.
Individuals at risk:
- whose work involves lifting weights - loaders, professional heavyweight athletes;
- those suffering from chronic infectious and inflammatory diseases of the joints or having close relatives suffering from such pathology;
- those suffering from spinal diseases – osteochondrosis, scoliosis, etc.;
- those who are overweight and lead a sedentary lifestyle;
- aged 50 years and older.
Is it possible to prevent cartilage destruction?
In the case of deforming osteoarthritis, prevention is possible only if we are talking about the primary form of the disease. If you have not yet been prescribed treatment for arthrosis, you can pay special attention to the load on your joints and prevent a possible problem. If, due to your line of work or as part of a hobby, you regularly expose your joints to microtrauma, it is not too late to stop this and thus protect the cartilage from damage.
It is almost impossible to prevent the development of so-called symptomatic osteoarthritis, caused by inferior cartilage due to abnormalities in other organs. If the cause of the destruction of cartilage tissue is congenital diseases, metabolic disorders, pathological conditions of the endocrine system or peripheral nerves, all that remains is to alleviate the symptoms of deforming osteoarthritis by turning to modern therapeutic methods.
In most cases, intra-articular injections of Noltrex can help relieve pain and restore joint mobility. The drug restores the viscosity of the synovial fluid, stops friction of cartilage and relieves pain, no matter what it is caused by - regular excessive stress on the knee, genetic predisposition or unfavorable environment.
Symptoms of coxarthrosis
The disease begins gradually, often unnoticed by the patient. It is very important to catch the first signs of the disease and not ignore them, but immediately consult a doctor.
But if this was not possible and serious changes have already occurred in the leg, the doctor will be able to help. It will eliminate pain and stop the progression of the disease.
The first signs of arthrosis of the hip joint
The initial symptoms of arthrosis of the hip joint are mild morning stiffness and the appearance of pain after a long walk or standing. The pain is usually localized in the hip joint and radiates to the groin or buttock. But sometimes the first signs of coxarthrosis are pain in the leg from the knee and below. They quickly pass in a state of rest.
Unfortunately, patients rarely consult a doctor when such signs appear; more often they simply ignore them and miss the opportunity to suppress the development of the pathological process at the very beginning, when this is easiest to do.
Obvious symptoms of arthrosis of the hip joint
The pain syndrome intensifies, spreads to the groin area, buttock, along the outer and inner surface of the thigh down to the knee, and then along the lower leg to the foot. There is a restriction in leg movements, especially during internal turns (inward rotation) and outward abduction. Pain also appears regardless of physical activity, including at night. They are often associated with changing weather conditions. Lameness appears, which forces the patient to walk using a cane.
The gait gradually becomes waddling, “duck-like.” The leg takes a forced position: it bends slightly at the hip joint, while the lower back protrudes slightly forward, and the pelvis tilts sideways, towards the coxarthrosis.
The patient begins to notice that the diseased leg becomes shorter and smaller in volume than the healthy one. Obvious symptoms of the disease do not raise doubts that the cause is damage to the hip joint. It is in this condition that patients most often consult a doctor.
Coxarthrosis is characterized by pain in the groin and on the outer side of the thigh.
Dangerous symptoms of hip arthrosis
If the following symptoms appear, you should immediately consult a doctor:
- severe joint pain, inability to step on the leg, feeling of instability - a sign of subluxation of the hip joint;
- an increase in body temperature in combination with increased pain in the leg is a sign of a joint inflammatory process; if the temperature is high, then there may be an infection;
- the affected leg has become significantly shorter than the healthy one, abduction to the side and inward rotation are impossible - a sign of loss of a significant part of the function of the joint.
Characteristic symptoms
Damage to the bone junction may be isolated, for example due to trauma. But the older a person gets, the more pain he experiences when bending his legs or arms and a decrease in flexibility in general. This happens because the normal production of cartilage tissue is inhibited. As a result, the frictional force begins to destroy the bone, thereby causing great discomfort.
The symptoms indicate destruction of the joints quite clearly. It is enough to pay attention to them to stop this process. A degenerative process in mobile bone junctions is indicated by:
- Pain and aching in the bones, especially when moving,
- Creaking, crunching and clicking in places where the limbs bend,
- Deformation and change in size of bone junctions,
- Swelling and hyperemia,
- Difficulty in movement, chronic arthrosis,
- Muscle stiffness and atrophy.
Why is coxarthrosis dangerous?
Any localization and form of arthrosis has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Osteoarthritis of the hip joint is dangerous because the disease constantly progresses to the point of complete loss of function, when the leg simply stops moving. There is also a danger of infection joining and spreading to adjacent tissues.
Degrees of coxarthrosis of the hip joint
There are 4 clinical and diagnostic stages of coxarthrosis (degree of damage to articular cartilage).
1st degree arthrosis of the hip joint
It can be asymptomatic, sometimes moderate pain appears after physical activity, quickly disappearing with rest. X-ray: no changes or slight narrowing of the joint space. MRI at stage 1 of coxarthrosis: signs of heterogeneity appear in the cartilage tissue.
Stage 2 arthrosis of the hip joint
The pain intensifies, radiates to the knee, shin and ankle, and does not go away immediately with rest. X-ray: obvious narrowing of the joint space and isolated growths of bone tissue (osteophytes) along the edge of the glenoid cavity. MRI at stage 2 of coxarthrosis: obvious defects (erosions, cracks) of cartilage with loss of less than half the volume of cartilage joint tissue.
3rd degree arthrosis of the hip joint
It is difficult to move the leg to the side and turn inward, the pain intensifies, and often appears at rest during sleep. Pain in the leg when walking forces the patient to take a forced position and rely on a cane. X-ray: the joint space narrows even more, many osteophytes lead to deformation of the hip joint. MRI at stage 3 of coxarthrosis: more than half the volume of cartilage tissue is destroyed. The third stage can still be treated conservatively.
Stage 4 arthrosis of the hip joint
Significant loss of joint function. The whole leg hurts: hip area, groin, gluteal area, hip, knee, ankle. Flat feet develop, the leg shortens, and the muscles atrophy. X-ray: multiple large osteophytes, the joint space is narrowed to a minimum or absent. MRI at stage 4 of coxarthrosis: there is no cartilage, changes appear in the bone subchondral tissue in the form of compaction (sclerosis).
Degrees of coxarthrosis
Possible complications of hip arthrosis
Regardless of the degree of coxarthrosis, treatment should begin immediately. It is better, of course, to do this in the early stages, but even in advanced stages, the doctor will always be able to help the patient, relieving him of pain and preventing the following possible complications:
- infectious and inflammatory purulent processes in the hip joint and adjacent tissues - accompanied by severe fever, chills, severe pain, tissue swelling; emergency surgery is required;
- subluxations and subluxations of the hip joint - manifested by severe limitations of movements in the leg and severe pain; will require hospitalization in the trauma department;
- pinching of the sciatic or femoral nerves by overgrown osteophytes - accompanied by severe radiating pain along the back of the leg (sciatic nerve) or the inner surface of the thigh and groin (femoral nerve); you will need urgent help from a neurologist and possibly a neurosurgeon;
- bursitis - inflammation of the synovial bursae - small cavities filled with joint fluid and located around the hip joint; they act as shock absorbers between the joint and surrounding tissues; in case of injury, cold, against the background of various diseases of the hip joint, they become inflamed; painful swelling, malaise, fever appears;
- tenosynovitis - inflammation of the inner lining of the sheath of the muscle tendons attached to the head of the femur; often develops in advanced stages of coxarthrosis, when the affected leg is shortened; manifests itself in severe pain when stepping on the foot;
- tunnel syndrome - nerve entrapment by large osteophytes; accompanied by severe neurological pain.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Exacerbations of arthrosis of the hip joint
Exacerbations of coxarthrosis are associated with periodically occurring inflammatory processes in the joint. Usually they are aseptic in nature and develop after additional injuries and any previous diseases. This pathological process is called arthrosis-arthritis; today it is more often called osteoarthritis or osteoarthritis, depending on which process (inflammatory or degenerative-dystrophic) predominates.
Exacerbation is manifested by increased pain, swelling of the periarticular tissues and a slight rise in temperature. If the fever is high and the general condition suffers, then this is most likely a sign of infection of the joint. If signs of exacerbation appear, you should:
- call a doctor at home - you cannot cope with this problem on your own;
- take any sedative (2 tablets of valerian extract, Novo-Passit tablet) and pain reliever (Paracetamol 500 mg tablet, Ketorol 10 mg, etc.); apply ointment or gel Diclofenac, Voltaren, Ketorol, etc. to painful areas of the body;
- lie down and take a position that minimizes pain;
- follow all doctor's orders; if the doctor believes that hospitalization is necessary, you should not refuse it.
Diagnosis of joint and bone diseases
The basis for diagnosing any disease is a thorough history taking. It is important to objectively assess the patient’s complaints and differentiate them from other diseases. For example, pain in the lumbar region can occur not only with lumbar osteochondrosis, but also with diseases of the pelvic organs, and the clinical picture of osteochondrosis of the thoracic spine is similar to the symptoms of pain in the heart and even heart attacks.
It is important to establish how long ago the complaints began, whether there are congenital anomalies, previous injuries, surgeries, infectious, inflammatory and chronic diseases. It is necessary to note when and how often exacerbations occur, how quickly these symptoms stop, whether they are associated with physical activity or occur at rest. Next, a visual inspection and palpation of the joints is necessary. The integrity, shape, size of the joint, color and temperature of the skin are assessed. You can palpate rheumatoid nodules, establish pain during passive movements, crunching, degree of loss of function, range of mobility.
Laboratory diagnostics is of great importance. A biochemical, general blood and urine test will allow you to assess the presence of an inflammatory process in the body. Synovial fluid can be used for research, which reflects the presence or absence of infectious agents in the joint cavity. To confirm the inflammatory process, its color, transparency, consistency, and viscosity are assessed.
Instrumental diagnostic methods are often the gold standard for diagnosing joint disease. X-ray examination is most informative for injuries of bones and joints, fractures, dislocations, and sprains. Ultrasound diagnostics (ultrasound) is used to assess the condition of soft tissues, muscles, ligaments, cartilage, and the level of synovial fluid. Magnetic resonance and computed tomography (MRI and CT) are reliable, non-invasive and safe research methods. It is possible to assess the degree of joint destruction, the spread of the pathological process, and evaluate the labor and clinical prognosis.
Types of arthrosis of the hip joint
Coxarthrosis is divided into types, forms and types according to different criteria: origin, nature of the course, characteristics of changes in tissues, etc.
By origin
On this basis they distinguish:
- primary or idiopathic type, the origin of which cannot be determined;
- secondary, with established causes, previous injuries, diseases, for example:
- post-traumatic coxarthrosis - develops after injuries (fractures, dislocations, ligament ruptures) or against the background of prolonged minor injury in athletes and people engaged in heavy physical labor;
- against the background of inflammatory processes in the joints (arthritis):
- localized – pathological process only in the hip joint;
- generalized - multiple joints become inflamed (rheumatoid, psoriatic, reactive arthritis).
According to the nature of the flow
Degenerative-dystrophic lesions of the hip joint always occur slowly and chronically. But during such diseases there are two types:
- low-symptomatic – occurs unnoticed or with mildly expressed symptoms, while radiological changes can progress regardless of the absence of clinical signs; develops more often in young and middle-aged people;
- manifest - all symptoms are clearly expressed, changes on x-ray lag behind them or are completely consistent; more common in old age; the course of this type is divided into rapidly and slowly progressing.
Sore joint on x-ray (right)
According to the characteristics of changes in articular tissues
The destruction of intra-articular cartilage is accompanied by the proliferation of replacement connective tissue. On this basis, the following types of changes in the TBS are distinguished:
- hypertrophic – connective tissue grows excessively, forming numerous osteophytes and sclerosis of bone subchondral tissue; is formed:
- deforming arthrosis of the hip joint is the most common outcome of the disease; due to overgrown osteophytes, the shape of the joint changes, branches of the nerves innervating the joints may be pinched, which leads to severe pain; dysfunction of the leg quickly develops;
- atrophic – the growth of connective tissue is insignificant, which leads to further injury and destruction of bone tissue.
Sedentary lifestyle
Not only dynamic loads are dangerous for joints, when a person, for example, works a lot physically, but also static ones, when he stays in one position for a long time.
Therefore, those who sit in an office chair most of the day and move little in their leisure time suffer from arthrosis quite often.
Article on the topic
Take care of your joints from a young age! How to reduce the risk of arthrosis This is due to a decrease in blood supply to the joint, which in this case is practically inactive.
Without receiving enough nutrients, intra-articular cartilage recovers more slowly.
Diagnostics
The correct diagnosis of the disease can only be made in a clinical setting. The Moscow Medical School has all the conditions for this.
Do not try to treat yourself: without a preliminary examination, this will lead to the progression of the disease and increased pain!
The following diagnostic tests are prescribed:
- Clinical – the doctor interviews and examines the patient.
- Laboratory:
- general and biochemical blood test - inflammatory processes and metabolic disorders are detected;
- If necessary, additional laboratory tests are performed to clarify the diagnosis.
- Instrumental:
- radiography of the hip joint - reveals violations of bone structures;
- MRI (magnetic resonance imaging) - detects changes in all joint tissues.
Chondroprotectors: what are they, how to choose, how effective are they?
Joint pain at rest
Causes of joint destruction
The source of joint disease can be both external factors and internal problems. If we ignore age-related changes, there are still quite a lot of factors that can disrupt the normal functioning of the musculoskeletal system.
First of all, these are professional and accidental injuries. They violate the integrity of bone structures and lead to various pathologies. It is also worth noting some inflammatory processes caused by fungi and viruses.
Another reason for joint destruction is heredity. The body's inability to regenerate cartilage normally may be inherited. To determine your susceptibility to bone joint diseases, conduct a DNA test. In our laboratory we will help you identify abnormalities and mutations in genes responsible for the musculoskeletal system.
Treatment of coxarthrosis
Therapy is prescribed individually and depends on the cause of the leg lesion, the stage of the disease, and the presence or absence of concomitant diseases. First, a complex of conservative therapy is prescribed. If this does not help and the disease progresses, accompanied by severe pain, surgical treatment is recommended.
At any stage of the disease, the main goals of treating arthrosis of the hip joint are:
- pain relief;
- suppression of disease progression;
- restoration of destroyed cartilage.
The complex of conservative therapy includes drug treatment and non-drug methods - diet, physiotherapy, therapeutic exercises, etc.
Drug treatment (pharmacotherapy) of coxarthrosis
All medications for the treatment of arthrosis of the hip joint are selected individually for each patient, taking into account the characteristics of his body.
To eliminate pain the following is prescribed:
- Paracetamol - tablets or rectal suppositories in a dosage of 500 mg are enough to relieve pain and minor inflammation (if any); can be repeated up to 4 times a day; the safest pain reliever;
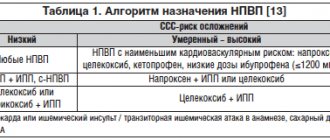
- drugs from the group of non-steroidal anti-inflammatory drugs (NSAIDs); Depending on the severity of the pain syndrome, they can be prescribed in the form of intramuscular (IM) injections, rectal suppositories, orally in the form of tablets and externally:
- diclofenac (trade names - Diclofenac, Voltaren) - an effective analgesic but often gives side effects from the stomach;
- ketorolac (Ketorol, Ketanov) is the most powerful pain reliever from the NSAID group, but also has side effects;
- ketoprofen (Ketonal) - less effective than Ketorol and Diclofenac, but there are fewer side effects;
- ibuprofen (Ibuprofen, Nurofen) - more suitable for relieving fever and inflammation, but also effective as a pain reliever; fewer side effects;
- nimesulide (Nimesulide, Nise) - belongs to a new generation of NSAIDs and almost does not irritate the stomach;
- Any ointment (cream, gel) based on NSAIDs is applied externally to the site of pain.
All NSAIDs have side effects, including irritating the gastric mucosa (risk of ulcers) and thinning the blood (risk of bleeding). In addition, they do not treat degenerative processes in the joints, but simply eliminate pain.
To eliminate muscle tension, muscle relaxants are prescribed. Tension of the muscles adjacent to the joint is a protective reaction of the body, but increases pain in the leg. To relax the leg muscles, tolperisone (Mydocalm) or tizanidine (Sirdalud) are prescribed.
To improve blood circulation and nutrition of the joint - pentoxifylline (Pentoxifylline, Trental) - dilates small blood vessels, improves blood circulation.
Drugs for the treatment of coxarthrosis
Chondroprotectors are used to restore cartilage tissue. This group of drugs includes chondroitin sulfate (CS) and glucosamine sulfate (GS):
- Dona (contains GS) is an effective remedy with a relatively short course of treatment;
- Structum (contains cholesterol) - you will have to be treated for at least six months;
- Teraflex (CS + GS) - course of treatment from 3 to 6 months;
- externally: Chondroitin (CS) ointment - 2 times a day for 3 weeks, Teraflex M (CS + GS) cream 2 - 3 times a day for a month; A small amount of ointment is applied to the skin and lightly rubbed.
Biologically active food additives (dietary supplements) of targeted action used in the treatment of arthrosis of the hip joint:
- Boswellia extract (Now Foods, USA) is a herbal preparation that protects cartilage from destruction, has an anti-inflammatory and analgesic effect; course of 1 capsule three times a day for a month;
- Connect Ol (Naturas Pluse, USA) – contains CS, GS, bromelain, calcium, zinc, copper, vitamin C, alfalfa, Chinese sea cucumber; course of 1 – 2 tablets per day for a month;
- Joint Formula (Cevan Nutritionals, USA) – contains GS; course of 1 capsule per day for a month.
Non-drug treatment of coxarthrosis
This is an even more significant section of the conservative treatment of arthrosis of the hip joint than medication. It includes proper nutrition, exercise and massage, and physiotherapy.
Nutrition for coxarthrosis
There is no special diet for degenerative-dystrophic diseases of the leg joints. But many people with sore feet are overweight. Therefore, sweets, baked goods, and sweet carbonated drinks should be excluded from the diet. It is necessary to significantly reduce the consumption of high-calorie foods: fatty meat, fish caviar, sausage. Regular consumption of alcohol is harmful - blood circulation in the joint is impaired.
You can eat lean meat, fish, dairy products, cottage cheese, cheese, buckwheat and oatmeal, first courses with vegetable or non-concentrated meat broth, compotes, fruit drinks.
Exercise therapy for arthrosis of the hip joint
The most important thing is to perform the exercises correctly, gradually increasing the load and not ignoring the appearance of pain (if pain appears, gymnastics should be stopped). Training should take place regularly. The first classes should be conducted under the supervision of a physical therapy instructor. And only after a while you will be able to conduct them yourself at home. Swimming in the pool, smooth gymnastics in the style of Pilates or yoga are very useful.
Exercise therapy for arthrosis of the hip joint strengthens muscles, activates blood circulation and metabolism, and helps restore the function of leg joints. Exercises for arthrosis of the hip joint can be performed from the starting position lying or standing.
Several exercise therapy exercises for the treatment of arthrosis of the hip joint
Physiotherapy for coxarthrosis
Physiotherapy procedures are of auxiliary importance, since the BTS is located deep under the muscle layer. However, sometimes electrophoresis with painkillers is prescribed to eliminate pain, and laser and magnetic therapy is prescribed to improve blood circulation.
In the absence of inflammatory phenomena in the joint, sanatorium-resort treatment with courses of ball and mud therapy is recommended. The resorts of Caucasian Mineralnye Vody are suitable.
How to treat arthrosis of the hip joint using traditional methods
Folk remedies are often included in complex treatment to reduce drug load:
- warming the upper part of the leg with sea salt; sew a long linen bag (must match the length of the upper leg), fill it with hot sea salt; First put a towel on the joint area, and then a bag; when the salt has cooled slightly, remove the towel, hold the sea salt until it has cooled completely; relieves pain, stimulates cartilage restoration, improves joint movements;
- honey massage; Use liquid warm honey as a massage oil: apply to the upper part of the leg and rub into the skin of the leg with light circular movements, patting occasionally, for three minutes; then wrap your leg and hold it there for two hours; perfectly relieves pain and activates blood circulation.
Surgical operations for coxarthrosis
Surgical treatment of arthrosis of the hip joint is recommended only in cases where all possibilities of conservative therapy have been exhausted, and the disease continues to progress and is accompanied by severe pain.
To help the patient, the following types of surgical interventions are used:
- arthrodesis – strong fastening of joint bones in the desired position using various structures; over time, this leads to their complete fusion; the leg fully performs the supporting function, but does not move, therefore arthrodesis is performed only if there are contraindications to other surgical interventions;
- femoral osteotomy – dissection of the femur to create an artificial fracture and subsequent fastening in the desired position using various metal structures; not only the supporting, but also partially motor function of the leg is preserved, pain disappears;
- endoprosthetics is the replacement of a destroyed joint with an artificial one that fully performs all the functions of the removed one.
Preventive actions
To prevent joint destruction, it is necessary to start taking care of their health as early as possible.
The following measures are recommended as prevention:
- Active lifestyle. Be sure to include sports in your life, move more, and do daily exercises.
- Proper nutrition. A balanced diet will help fill nutritional deficiencies and keep your weight under control.
- Use of chondroprotectors. The price of such products is low, but they help slow down the wear of joints.
- Quality rest. After physical labor, it is necessary to ensure proper rest, relaxation of muscles and ligaments.
- Avoiding injury. Even minor impacts and falls from low heights can negatively affect the condition of joints in the future.
- Taking vitamins. If there is a deficiency of calcium and other elements, it is necessary to replenish it with the help of nutritional supplements.
- Health monitoring. Internal problems inevitably affect the state of all body systems, so they must be eliminated without delay.
- Timely access to the hospital. If symptoms of joint destruction appear, you should immediately seek qualified medical help.
You can get more useful information about the destruction and subsequent restoration of joints from the video in this article.
Approach to treating the disease in our clinic
Moscow Medical Specialists have extensive experience in treating degenerative-dystrophic diseases of the leg joints. If coxarthrosis is suspected, a full examination of the patient is first performed using the most modern diagnostic methods, including MRI. And only after the final diagnosis and stage of the disease is established, comprehensive treatment is prescribed.
A special feature of the treatment in our clinic is that doctors use not only the most modern methods of treating leg diseases, but also the use of traditional oriental techniques that have been successfully used for centuries by doctors of Ancient China and Tibet. To treat coxarthrosis we use:
- PRP therapy is an advanced modern technique for activating restoration processes in the hip joint by introducing the patient’s platelets into the pathological focus; This method can restore cartilage tissue;
- methods of reflexology (RT) – influence in various ways on points on the human body that are reflexively connected with the tissues of the hip joint; techniques such as acupuncture, moxibustion with wormwood cigarettes, acupressure, auriculotherapy (impact on points in the ear area), etc. are used;
- manual therapy – a chiropractor uses his hands to correct the position of the hip bones;
- hirudotherapy - treatment with leeches that improve blood circulation in the leg, which leads to the restoration of cartilage tissue of the joint;
- kinesiotherapy – restoration of motor function of the hip joint with the help of specially selected therapeutic movements.
And these are not all the methods used. An integrated approach to treatment allows not only to quickly eliminate symptoms, but also to prevent exacerbations and improve overall well-being. If you have problems with your leg joints, contact the Paramita clinic, we will definitely help you!
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthrosis
Common diseases
Any pathology that provokes the destruction of cartilage can be divided into two types: inflammatory and non-inflammatory. The first affects the soft tissues located around the cartilage. It is caused by various viruses or infections. This process can be stopped with medication and therapy.
The second type develops regardless of external factors. This includes arthritis and arthrosis, osteoporosis and rheumatism. Treatment of such processes is a long and difficult process. In some cases, it is only possible to eliminate pain, since self-medication is ineffective.
Hip joints
The problem with the destruction of the hip joint, as this connection is called, is that it occurs with virtually no symptoms. You may not know about the destructive processes inside your body for years. The appearance of aching pain, difficulty moving and swelling in the morning indicates that the process has gone far. In this case, the pathological changes are practically irreversible.
To prevent complete destruction of the joint cartilage, undergo periodic check-ups with an orthopedist. This will allow you to monitor changes in cartilage. Timely treatment will protect you from serious consequences and disability.
Destruction of knee joint cartilage
The degenerative process in the knees begins quite early. Young people do not notice these changes, since the joint itself is protected by the menisci. You do not feel pain or discomfort. And only after they are completely thinned do the cartilaginous formations begin to suffer.
Dangerous consequences for the knees come from injuries, congenital pathologies, dislocations and uncomfortable shoes. If you spend a lot of time on your feet, choose shoes with increased shock absorption that will reduce the stress on bone joints. This will help maintain the functionality of your legs for a long time. Otherwise, you will lose the ability to move without pain and discomfort.
Ankle fracture
The special structure of the bone joints in the ankle allows you to avoid serious destruction. The load is evenly distributed over the entire surface of the system, thus protecting against damage. At a young age, tendons and ligaments in this area often suffer, especially in athletes. But the peculiarity of the body allows one to cope with such injuries quite quickly.
The main risk factor for cartilage joint destruction is excess weight. It leads to abnormal stress and the development of plantar fasciitis. Wrong shoes can also lead to inflammation and damage to the cartilage layers. This applies most of all to high heels and completely flat soles.
General clinical recommendations for coxarthrosis
To prevent the disease from progressing, you must adhere to the following rules:
- move more, but do not forget to give the sore leg rest;
- completely avoid lifting heavy objects and standing for long periods of time;
- daily perform a complex of exercise therapy prescribed by your doctor, swim, do yoga;
- eat properly, fully, but exclude high-calorie foods from the diet;
- get rid of excess body weight;
- Regularly visit your doctor and carry out preventive courses of treatment.
Prevention of arthrosis of the hip joint
Preventing the development of coxarthrosis is easier than treating it. To do this, you need to lead a healthy lifestyle, do as much sports as possible, and eat right. If you have close relatives suffering from coxarthrosis, it is better not to engage in strength sports and heavy physical labor.
Excess weight
The weight of the body puts pressure on the supporting joints - hip and knee, as well as on the joints of the spine.
And the more excess kilograms a person has, the higher the load and the correspondingly higher the risk that the intra-articular cartilage will begin to wear out ahead of time.
In addition, adipose tissue impedes the flow of blood to the joint, and therefore its nutrition. By the way, excess weight not only increases the risk of arthrosis, but also worsens the course of the disease - joint destruction progresses faster.
Frequently asked questions about the disease
How does arthrosis of the hip joint hurt?
Characterized by pain in the groin and on the outer side of the thigh, extending to the knee. The buttock area hurts less often.
Is it possible to cure a hip joint without surgery?
It will not be possible to completely cure, but it is quite possible to eliminate the pain, stop the destruction of the joint and partially restore the cartilage. Surgery is performed when conservative treatment does not help.
Who treats arthrosis of the hip joint?
Traumatologist-orthopedist.
How can I determine if I have coxarthrosis?
Coxarthrosis can be suspected when there is pain in the groin, radiating to the leg, as well as when pain occurs while walking. After this, it is better to consult a doctor immediately.
Degenerative-dystrophic diseases of the joints of the legs and primarily the hip joint are dangerous because, due to constant high load, they very quickly lead to disability. Therefore, it is very important to immediately consult a doctor at the slightest suspicion of such a pathology. And don’t be afraid of anything: the specialists of the Paramita clinic in Moscow will help you in any case, even if you have advanced disease and can barely walk.
Literature:
- Volokitina, E. A. Coxarthrosis and its surgical treatment: abstract. dis. Doctor of Medical Sciences / E. A. Volokitina. - Kurgan, 2003. - 46 p.
- Comprehensive characteristics of degenerative changes in coxarthrosis /E. A. Volokitina et al. // New technologies in medicine: abstract. scientific-practical conf. in 2 parts - Kurgan, 2000. - Part 1. - P. 48-49.
- Ganz R., Leunig M., Leunig-Ganz K. et al. The etiology of osteoarthritis of the hip. An Integrated Mechanical Concept. Clin Orthop Relat Res 2008;466(2):264–72.
- Mastbergen SC, Bijlsma JW, Lafeber FP Synthesis and release of human cartilage matrix proteoglycans are differently regulated by nitric oxide and prostaglandin-E2. Ann Rheum Dis 2008;67(1):52–8.
Themes
Arthrosis, Joints, Pain, Treatment without surgery Date of publication: 08/24/2021 Date of update: 08/25/2021
Reader rating
Rating: 4.33 / 5 (3)
Most common cartilage injuries
Most often, patients need treatment for arthrosis, osteoarthritis and its deforming form after such injuries:
- prolonged mechanical load on the joint, which exceeds the permissible limit, for example due to banal excess weight;
- chronic microtraumas of joints received during professional activities, for example among loaders, blacksmiths;
- sports injuries - while running, playing football, weightlifting, jumping.
For one reason or another, the amount of proteoglycans in the body rapidly decreases, and the collagen fibers of hyaline cartilage are damaged. This leads to the death of chondrocytes - the cartilage gradually becomes thinner.
Deforming osteoarthritis of the hand joints - an occupational disease of loaders and riggers