- General recommendations
Coxarthrosis of the hip joint of the 3rd degree is an extreme degree of manifestation of the degenerative-dystrophic process, depriving a person of the opportunity to work and leading to disability.
At the last stage of coxarthrosis, complete destruction of the joint is observed, which requires endoprosthetics
Signs of deforming osteoarthritis (DOA) are observed in patients after 40 years of age. Depending on the rate of cartilage destruction, from the moment the first symptoms appear to its final destruction, it can take from 5 to 15 years.
The disease often occurs against the background of anatomical and functional inferiority of the hip joint (congenital or acquired).
Reasons for the development of coxarthrosis
The main risk factors for arthrosis are:
- long-term overload of the joint in people with large body weights, athletes (gymnasts, wrestlers, divers);
- consequences of hip injury;
- recurrent arthritis of various etiologies;
- Perthes disease: congenital insufficiency of blood supply and nutrition of joint tissues;
- congenital hip dislocation;
- hip dysplasia;
- necrosis of the femoral head;
- diabetes mellitus, metabolic syndrome, dishormonal processes;
- passive lifestyle;
- involutive changes that accompany the aging process of the body.
The disease can develop in one joint (right-sided or left-sided coxarthrosis); in severe cases, the process is bilateral.
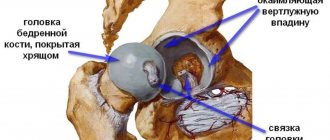
Mechanism of disease development
In the first two stages of DOA, gradual degradation of cartilage occurs (it becomes thinner, microcracks appear on the surface), sclerotic processes in the subchondral layer of bone, and the formation of osteophytes. Without treatment, joint damage continues to progress.
As the disease progresses, cartilage tissue thins and osteophytes grow
At the last stage of coxarthrosis, the cartilage becomes so thin that cracks in it reach the subcartilaginous layer, and in some places the cartilage tissue may be completely absent. The synovial cavity is filled with its fragments, which interferes with full movement.
In order to increase the area of contact between the articular surfaces and thereby reduce the load, an even greater number of osteophytes are formed along the edges of the bone. Overload of the subchondral area leads to the formation of cysts and disruption of the blood supply to the bone. The friction of exposed bones against each other increases pain.
Constant spasm of the muscles adjacent to the joint creates strong pressure on the articular surfaces. Fibrous ankyloses (fusions) are formed, which, without surgical treatment, completely immobilize the limb.
Symptoms of coxarthrosis of the hip joint grade 3
This stage of deforming osteoarthritis is characterized by the fact that all manifestations of the disease reach their maximum.
The main symptoms of grade 3 coxarthrosis:
| Symptom | Characteristic |
| Pain | Constant (including at night), worsened by the slightest movement of the limb. Even palpation of surrounding tissue causes discomfort to the patient. |
| Crunching | Can be heard clearly even from a distance |
| Limited mobility | The patient can move independently only with assistive devices over short distances. Internal rotation, abduction and flexion are most difficult |
| Deformation | Visually noticeable, multiple bone growths are palpable. The limb is greatly shortened, occupies a forced position (adducted and rotated inward) |
The muscles of the buttocks and thighs are weakened and atrophied. With a unilateral process, the difference in the volume of the limbs is visually noticeable. The patient's curvature of the spine in the lumbar region (lordosis) worsens. At this stage of progression of coxarthrosis, the gait becomes antalgic - when trying to load the affected limb, the pelvis drops.
In the third stage of DOA of the hip joint, complications are often observed:
- secondary bursitis, synovitis;
- pathological dislocations;
- secondary fracture of the femoral neck;
- aseptic necrosis of the femoral head;
- protrusion of the acetabulum.
Prevention
To prevent coxarthrosis, it is necessary:
- monitor your weight;
- prevent obesity;
- protect yourself from injury (for example, wear non-slip shoes);
- do physical education.
At risk are people over forty and those who have had a fracture of the femoral neck, athletes, and relatives of patients with coxarthrosis. All people entering here should see an orthopedist when the first symptoms of osteoarthritis appear. Early diagnosis and timely treatment will relieve pain, lameness, expensive therapy, the need to impose serious restrictions on life, and surgical intervention.
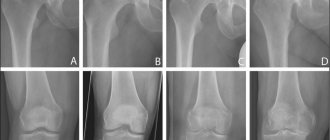
Diagnosis of coxarthrosis
It is not difficult to suspect the presence of DOA of the hip joint with such a clear clinical picture.
To confirm the diagnosis, radiography is performed
After interviewing the patient and examining him, the doctor will prescribe additional tests:
- x-ray of two hip joints;
- Ultrasound measuring cartilage thickness;
- arthroscopy;
- MRI or CT.
X-ray changes in coxarthrosis of the 3rd degree:
- significant narrowing or complete absence of the joint space;
- multiple osteophytes (mushroom-shaped head of the femur);
- subchondral sclerosis, cysts;
- bone tissue with areas of osteoporosis;
- change in the configuration of the femoral head;
- deepening of the acetabulum;
- aseptic necrosis of the femoral head;
- subluxations.
Treatment without surgery
For grade 3 coxarthrosis of the hip joint, treatment without surgery is a temporary supportive measure. If the disease has already reached this stage, the operation must still be performed, because it is impossible to restore the destroyed joint structures with pills and injections.
How you can treat grade 3 coxarthrosis of the hip joint without surgery - it depends on the severity of the degeneration of cartilage tissue. The treatment regimen is selected by the attending physician individually.
Drug therapy
The medicine relieves pain well (should be taken after meals)
For grade 3 arthrosis of the hip joint, treatment begins with the prescription of effective painkillers. Additionally, injections, restorative drugs and medications are used to improve blood supply to tissues.
- Potent non-steroidal anti-inflammatory drugs help relieve joint pain, so for grade 3 coxarthrosis, treatment begins with them. The most effective drugs are Diclofenac, Ketoprofen, Nimesulide. The downside is a negative effect on the stomach and intestines and many contraindications, so such medications are used for a short course.
- To treat grade 3 coxarthrosis without surgery, intra-articular injections of hormonal drugs are used. They reduce swelling caused by stagnation of synovial fluid, relieve the inflammatory reaction provoked by the pressure of osteophytes, and reduce pain. For this purpose, the drug hydrocortisone and analogues are used. Only a doctor gives injections.
- Various vasodilators are used to reduce pain. Such medications dilate peripheral vessels and improve the flow of blood, and with it oxygen, into the diseased joint. Cinnarizine, Nicotinamide and analogues are used.
- If the cartilage is not destroyed, but only thinned, it is advisable to use chondroprotectors. These drugs stimulate the nutrition of cartilage tissue and gradually restore it. Medicines based on chondroitin (Chondroxide) and biostimulants made from calf cartilage tissue extract are used.
- To speed up regeneration, improve metabolism and normalize blood circulation, the doctor may recommend general strengthening agents. For joint pathologies, vitamin and mineral complexes, nutritional supplements with chondroitin and glucosamine, amino acid complexes and Omega-3 are prescribed.
It is possible to treat grade 3 coxarthrosis of the hip joint with the listed drugs only in order to relieve the symptoms, but no drugs can completely restore the damaged joint.
Stem cells
While patients are wondering whether it is possible to cure grade 3 coxarthrosis of the hip joint without surgery, and whether they can manage with medications alone, science does not stand still. One alternative treatment method is stem cell therapy.
A stem cell is an immature cell capable of growth and self-renewal. Initially, research concluded that embryonic stem cells would help in the fight against various pathologies. This approach is inhumane and contrary to ethics. Research on human stem cells has officially stopped, and plant stem cells are used for treatment.
Many people do not understand what the drug is and are willing to pay a lot of money for a medicine made from soy stem cells. However, such drugs cannot relieve coxarthrosis, except perhaps due to the placebo effect. Treatment of grade 3 coxarthrosis of the hip joint with stem cells can theoretically initiate the process of renewal of cartilage tissue, but the method has not been sufficiently studied.
Exercises for the joint
Gymnastics is advisable only for initial forms of pathology
Having understood what grade 3 coxarthrosis of the hip joint is, and what stages of this disease there are, we should dwell in more detail on such a treatment method as exercise therapy.
Physical therapy (this is what the abbreviation stands for) helps a lot in the first stage of the disease, and does a good job of supporting movement in the joint in stage 2 of the disease. But with grade 3 coxarthrosis, this technique is not only effective, but also dangerous, because when performing special exercises, a person heavily loads the hip joint, which is deformed and cannot cope with the load. Physical education is allowed only as prescribed by a doctor and only in a physical therapy room, however, in 80% of cases of third degree coxarthrosis, exercise is contraindicated.
Massage and joint traction
Massage is a good way to eliminate symptoms of various joint diseases, including coxarthrosis of the hip joint, but must be prescribed by the attending physician. In general, manual therapy does not quickly restore the joint, but it does significantly reduce pain and lameness. A chiropractor can also stretch the joint, thereby relieving lameness due to a shortened limb.
Physiotherapy
Having figured out how to cure grade 3 coxarthrosis without surgery, you should pay attention to methods of improving blood supply to the hip joint. Physiotherapy is prescribed to reduce swelling, pain and inflammation, but is almost ineffective as a standalone remedy.
For grade 3 coxarthrosis, physiotherapy is prescribed to speed up recovery, reduce discomfort and as preparation for surgery. The most commonly used are medicinal electrophoresis, magnetic therapy, and laser treatment.
Diet and folk remedies
The third degree of coxarthrosis of the hip joint can be treated without surgery, but not with folk remedies. They are ineffective and a waste of time when a person is one step away from disability and complete loss of mobility in the joint. For those who cannot do without home remedies, you can try rubbing tinctures of lilac flowers or propolis.
Folk remedies are ineffective because they act on the surface and do not penetrate deep into the joint. The same is true for various pain-relieving ointments and gels.
Another questionable step in the treatment of stage 3 coxarthrosis of the hip joint is diet. In many sources you can find descriptions of miraculous products for joint destruction - chicken paw broth, gelatin drink, jellied meat and fatty fish soup. All of these products do stimulate collagen production, contain collagen and Omega-3, and may be generally beneficial for health, but they do not restore joints.
The diet is recommended for obese people to reduce the load on the joint. To lose weight, you need to reduce the calorie content of your meals and give preference to simple, healthy foods.
Treatment of coxarthrosis of the hip joint 3rd degree
It is impossible to cure a joint affected by osteoarthritis; it cannot be restored. Basic therapy with chondroprotectors and intra-articular injections of glucocorticosteroids are ineffective.
Analgesics, such as Paracetamol, are prescribed to relieve pain.
Therapy for the advanced stage of DOA is aimed at pain relief, training in the use of auxiliary instruments and preparation for surgical intervention (muscle strengthening, physiotherapy, hardware traction, treatment of concomitant pathologies, weight correction).
To reduce the intensity of pain, the following are prescribed:
- non-steroidal anti-inflammatory drugs (NSAIDs): preferably from the group of selective COX-2 blockers;
- non-narcotic painkillers: Paracetamol;
- narcotic analgesics: Tramadol, used for severe pain resistant to other drugs.
Passport part. Full name: Age: 61 years old (12/3/1944) Place of residence: Profession: pensioner Date of admission: 03/27/2006 810 Date of supervision: 04/27/2006-05/6/2006
Complaints. Complaints upon admission: pain in the hip joints, pain on the outer surface of the right thigh; pain in the right knee joint; tingling sensation in right thigh; restriction of movement in the right hip joint. Complaints at the time of supervision: pain in the area of the right hip joint; limited mobility in the right hip joint due to pain.
Anamnesis morbi. She has been ill since 2002, when pain in the right hip joint first appeared. She did not seek medical help. Gradually the pain intensified, and limited mobility in the joint appeared. She took ortofen on her own, after which she noted a decrease in pain. Since September 2005, he has noticed increased pain and limited mobility in the right hip joint. On March 27, 2006, she was hospitalized in the 17th department of the regional clinical hospital in Ryazan, where examinations were carried out and the diagnosis was made: Bilateral coxarthrosis on the right, stage III, on the left, stage I. Mixed contracture of the right hip joint. Preoperative preparation, treatment of concomitant pathologies and surgery on April 26, 2006 were carried out: primary total arthroplasty of the right hip joint, cement fixation of the components.
Anamnesis vitae. Born in the Tambov region with. Vanovo in 1944. She grew and developed normally. Household history: living conditions are satisfactory. Food: satisfactory. Work history: Bad habits: does not smoke, does not abuse alcohol, does not use drugs. Past diseases: acute respiratory viral infections, acute respiratory infections. In 1994, she underwent surgery - arthrodesis of the left knee joint; in 2003, 2004, 2005, operations for a hernia of the anterior abdominal wall. Concomitant diseases: Osteochondrosis. Spondylosis of the thoracic and lumbar spine, osteoporosis. Coronary heart disease, aortic atherosclerosis, combined aortic valve disease. Chronic heart failure stage I Hypertension, stage II. III Art. risk IV. Peptic ulcer of the stomach and duodenum is in remission. Cholelithiasis. Chronic calculous cholecystitis in remission. Allergic history: without features. Heredity: not burdened.
Status praesens. The patient's condition is satisfactory. The situation is forced. The body type is normosthenic, proportional. The type of hair growth corresponds to gender and age. Skin: pink in color, no rashes, on the anterior abdominal wall there is a postoperative scar of about 10 cm, on the lateral surface of the thigh there is a postoperative suture of about 30 cm. The nails are oval, brittle, and there is no deformation of the nail plates. Visible mucous membranes are pink. Increased deposition of subcutaneous fat on the abdomen, hips, and shoulders. The thickness of the subcutaneous fat fold in the navel area is 5 cm. Peripheral lymph nodes: occipital, parotid, submandibular, supra and subclavian, axillary, cubital, inguinal, popliteal - not enlarged, painless, of normal density, mobile. The pharynx is clean, the tonsils are not enlarged, their mucous membrane is pink. The muscles are moderately developed, muscle tone and strength are preserved and are the same on both sides. In the left hip joint, movements are limited and moderately painful; in the left knee joint, movements are absent; in the left ankle joint, movements are reduced and painless. In the right hip joint, movements are limited and painful; in the knee joint, movements are slightly reduced and painless. In other joints, movements are complete and painless. The nail phalanges of the fingers are not changed. The skull is round in shape, medium in size.
Status localis.
The area of the hip joints is without features. Painful on palpation. Movement in the hip joint is limited by pain. There is a deficit of extension in the right hip joint. Movements in the hip joint: Right Left Flexion/extension 30°/30° 80°/0° Abduction/adduction 0°/0° 0°/0° Internal/external rotation 0°/0° 0°/0°
Right Left Thigh volume 51 cm 50 cm Shin volume 35 cm 35 cm
Research of the cardiovascular system
Complaints of shortness of breath that occurs after physical activity (walking a distance of about 200 m). Examination of the heart area.
The shape of the chest in the area of the heart is not changed. The apical beat is visually and palpably determined in the 5th intercostal space, 1.5 cm inward from the linea medioclavicularis sinistra, reinforced, with an area of 1.5 cm. The cardiac beat is not palpable. A cat's purr in the second intercostal space on the right at the sternum and at the apex of the heart cannot be detected. There is no “carotid dance”. On palpation, pulsation in the peripheral arteries is preserved and is the same on both sides. On palpation of the radial arteries, the pulse is the same in both arms, synchronous, rhythmic, with a frequency of 76 beats per minute, satisfactory filling, not tense, the shape and size of the pulse are not changed. The veins of the lower extremities are varicose.
Limits of relative cardiac dullness.
The right border is determined in the 4th intercostal space - 2 cm outward from the right edge of the sternum; in the 3rd intercostal space 1.5 cm outward from the right edge of the sternum. The upper border is determined between the linea sternalis and linea parasternalis sinistra at the level of the 3rd rib. The left border is determined in the 5th intercostal space 1.5 cm outward from the linea medioclavicularis sinistra; in the 4th intercostal space 1.5 cm outward from the linea medioclavicularis; in the 3rd intercostal space 2 cm outward from the line parasternalis sinistra. Limits of absolute cardiac dullness.
The right border is determined in the 4th intercostal space 1 cm outward from the left edge of the sternum. The upper border is determined on the 3rd rib, between the linea sternalis and parasternalis. The left border is determined 0.5 cm inward from the left border of relative cardiac dullness. The vascular bundle is located in the 1st and 2nd intercostal spaces, and does not extend beyond the edges of the sternum. On auscultation, heart sounds are muffled, there is an accent of the second sound on the aorta. Blood pressure 130/90.
Respiratory system.
There are no attacks of suffocation. There is no pain or hemoptysis, no sputum. Examination: the shape of the nose is not changed, breathing through the nose is not difficult. The larynx is not deformed. The inhalation/exhalation ratio is not changed. Accessory muscles are not involved in the act of breathing. The chest is normosthenic, the supra- and subclavian fossae are filled, the width of the intercostal spaces is not increased. The type of breathing is mixed, respiratory movements are symmetrical, breathing is rhythmic, shallow, respiratory rate is 25. On palpation, the chest is painless, elasticity is reduced. Voice tremors are not weakened. On percussion, a pulmonary sound is noted on both sides. Boundaries of the lungs:
Upper front standing height standing height back right 3cm VII cervical left 3cm VII cervical
lat. margins Krenig 8 cm 8 cm Lower
along the parasternal 6th rib is not identified. along the midclavicular 7th rib is not identified. along the anterior axillary 8 rib 8 rib along the mid-axillary 9 rib 9 rib along the posterior axillary 10 rib 10 rib along the scapular 10 rib 10 rib along the paravertebral 11 rib 11 rib Respiratory excursion of the lower edge of the lung along the mid-axillary 8 cm 8 cm On auscultation: weakened vesicular breathing. No wheezing or pathological noises are heard.
Digestive system.
The mucous membranes of the cheeks, lips, and hard palate are pink. Gums are pink, normal moisture. There is no caries, the teeth are not loose. Examination of the tongue: the tongue is of normal size, pink, moist, not coated, the papillae are preserved. The belly is rounded and symmetrical. On superficial palpation the abdomen is soft and painless. Deep palpation. In the left iliac region, a painless, elastic, shifting, slightly rumbling, with a smooth surface sigmoid colon with a diameter of 2 cm is determined. The cecum with a diameter of 2.5 cm is palpated in the right iliac region, painless, mobile, slightly rumbling. The transverse colon is determined at the level of the navel in the form of a soft, elastic cylinder, 3 cm in diameter, not rumbling, easily moved, painless, with a smooth surface. The greater curvature of the stomach is determined by ballot palpation 3 cm above the navel. The lower edge of the liver does not protrude from under the right hypochondrium. Smooth, painless, densely elastic consistency. The gallbladder is not palpable. The spleen is not palpable. Painless.
Urinary system. Urination is painless, the amount of urine is normal. The kidneys are not palpable. Pasternatsky's sign on the right and left sides is negative. Palpation along the ureter is painless. The bladder is not palpable; palpation in the area of its projection is painless.
Neuropsychic status.
Consciousness is clear, sleep is normal, mental state is without any peculiarities. Pupillary and tendon reflexes were preserved and were identical on both sides. Skin sensitivity is preserved. There are no pathological reflexes. There is no tremor of the limbs. Hearing is within normal limits. There is no visible enlargement of the thyroid gland. Upon palpation, its isthmus is determined in the form of a soft, mobile, painless roller. Dermographism is pink and appears quickly
Preliminary diagnosis Based on the patient's complaints: pain in the hip joints, pain on the outer surface of the right thigh; tingling sensation in right thigh; restriction of movement in the right hip joint. Based on the medical history: she has been ill since 2002, when pain in the right hip joint first appeared. She did not seek medical help. Gradually the pain intensified, and limited mobility in the joint appeared. She took ortofen on her own, after which she noted a decrease in pain. Since September 2005, he has noticed increased pain and limited mobility in the right hip joint. On March 27, 2006, she was hospitalized in the 17th department of the regional clinical hospital in Ryazan, where examinations were carried out and the diagnosis was made: Bilateral coxarthrosis on the right, stage III, on the left, stage I. Mixed contracture of the right hip joint. An operation was performed: primary total arthroplasty of the right hip joint, cement fixation of the components. Based on objective examination data: Movement in the left hip joint is limited and moderately painful; movement in the right hip joint is limited and painful. The area of the hip joints is painful on palpation. Movement in the right hip joint is limited by pain. Movements in the hip joint: Right Left Flexion/extension 30°/30° 80°/0° Abduction/adduction 0°/0° 0°/0° Internal/external rotation 0°/0° 0°/0°
Right Left Thigh volume 51 cm 50 cm Shin volume 35 cm 35 cm
You can make a preliminary diagnosis: Main diagnosis: Bilateral coxarthrosis on the right, stage III, on the left, stage I. Mixed contracture of the right hip joint. Concomitant diseases: Osteochondrosis. Spondylosis of the thoracic and lumbar spine, osteoporosis. Coronary heart disease, aortic atherosclerosis, combined aortic disease. Chronic heart failure stage I Hypertension, stage II. III Art. risk IV. Gastric ulcer in the acute stage, duodenal ulcer in remission. Cholelithiasis. Chronic calculous cholecystitis in remission.
Examination plan:
1. General blood test 2. Biochemical blood test: total protein, bilirubin (total, direct, indirect), AST, ALT, urea, residual nitrogen, creatinine. 3. Blood test for RW 4. Blood glucose. 5. Coagulogram 6. Blood test for group and Rh factor 7. General urine test 8. Feces for worm eggs 9. Chest X-ray 10. X-ray of the hip joints. 11. X-ray of the thoracic and lumbar spine in 2 projections. 12. X-ray of the knee joints in 2 projections 13. Ultrasound examination of the abdominal organs 14. Ultrasound examination of the heart 15. Fibrogastroduodenoscopy 16. Consultation with a therapist 17. Consultation with a neurologist 18. Consultation with a gastroenterologist 19. Ultrasound examination of the vessels of the lower extremities 20. Ultrasound examination of the shield ovary gland
Data from laboratory and instrumental research methods, as well as consultations with specialists.
General blood test Erythrocytes, x1012/l Hemoglobin, g/l Ht Color indicator Leukocytes, x109/l Eosinophils, % P/I, % S/I, % Lymphocytes, % Mono- citations, % ESR 03/28/06 4.6 144 0.94 6.9 — — 58 33 9 28 04/25/06 4.5 144 04/26/06 4.5 146 0.42 0.95 8.9 1 3 63 31 2 27 04/27/06 4.3 136 0.41 04/28/06 4.0 128 0.38 04/29/06 4.3 130 0.41
General urine analysis Specific weight Reaction Color Transparency Protein, g/l Flat epithelium in the subfield Leukocytes in the subsection Erythrocytes in the subsection Oxalates Mucus 03/28/06 1020 acidic Yellow. transparent 0 3-4 5-6 0-1 04/25/06 1020 acidic S/w transparent 0 2-4 Unit. 1-2 04/27/06 1025 sour Yellow. transparent 0.033 1-2 35-40 04/29/06 1024 acidic n/t 0.033 Unit. 1-2 15-20 + +++
03/28/2006 Blood test for group and Rh factor Conclusion: 0(I) Rh+
03/28/2006 Blood glucose Conclusion: 4.6 mmol/l
03/28/2006 Biochemical blood test Protein: 76 g/l Total bilirubin - 12.4 µmol/l direct - 2.4 µmol/l indirect - 10.0 µmol/l Urea: 4.8 mmol/l AST: 1.40 µmol/l ALT: 1.37 µmol/l Residual nitrogen: 17.4 mmol/l Creatinine: 0.05 µmol/l
03/28/2006 Coagulogram Fibrinogen - 3.77 g/l Fibrinolytic activity 12' Plasma tolerance to hepatitis - 7' Thrombin time - 16' Fibrinase activity 60% Prothrombin index 0.76 03/28/2006 Blood test for RW Conclusion: RW negative
03/27/2006 Feces for worm eggs Conclusion: I/g – “negative”, parasites – “negative”.
03/27/2006 Ultrasound examination of the thyroid gland No. 533 The thyroid gland is located low. The structure is heterogeneous, echogenicity is moderately reduced. Right lobe: 23x21x57 mm Left lobe: 24x21x62 mm Isthmus: 9 mm
03/29/2006 X-ray of the spine, knee joints, hip joints No. 1259. On the X-ray of the pelvis in the right hip joint, the gap is significantly narrowed, subchondral sclerosis and marginal bone growths are noted. On the left there is moderate subchondral sclerosis of the articular cavity. Conclusion: Deforming arthrosis of the hip joints: on the right, stage III, on the left, stage I. An x-ray of the lumbar spine reveals diffuse osteoporosis and pronounced manifestations of spondylosis deformans in the form of osteophytes on the lateral and anterior surfaces of the vertebral bodies. An x-ray of the knee joints shows bone ankylosis on the left, and moderately pronounced manifestations of deforming arthrosis in the form of narrowing of the joint space on the right.
03/30/2006 Ultrasound examination of the heart No. 1184 Left ventricle: cavity of normal dimensions EDC 5.1 cm, ESR 3.3 cm Thickness of IVS 11 mm, LVSD 11 mm Global contractility: satisfactory Ejection fraction 64%, FS 35%, VA>VE, IVRT – 0.12 s Local contractility: no violations were detected. Right ventricle: normal size. PPV 1.6 cm Left atrium: moderately enlarged to 3.7x5.1x4.1 cm Right atrium: not enlarged. Aorta: normal size. AO - 3.2 cm. Features: the walls are unevenly thickened in the ascending section; there are areas of calcification. Pulmonary artery: normal size. Mitral valve: no changes, no signs of stenosis. Regurgitation stage I Aortic valve: three leaflets. The amplitude of expansion is 1.2 cm, there are signs of stenosis. Maximum gradient 24 mmHg. Regurgitation stage I Pulmonary valve: no changes Tricuspid valve: no changes. Other: no pathological shunts or pulmonary hypertension were detected. Conclusion: combined aortic defect, moderate stenosis, aortic valve insufficiency. Signs of atherosclerosis of the aorta, aortic valve. Enlargement of the left atrium. Type I disorder of left ventricular diastolic function.
03/28/2006 Fibrogastroduodenoscopy No. 1692. The esophagus is freely passable, the mucous membrane of the abdominal region is hyperemic. The cardia does not close completely. The stomach contains a moderate amount of cloudy liquid, which expands well with air. The folds are moderately pronounced and convoluted. Peristalsis can be observed. The mucous membrane is swollen and hyperemic. In the antrum along the lesser curvature there is a mucosal defect with a depth of 0.1-0.2 cm. Biopsy and smear. We pass the gatekeeper. The bulb is deformed. The mucous membrane is swollen and hyperemic. Conclusion: Ulcer of the antrum of the stomach. Deformation of the duodenal bulb. Cardia failure. Bulbitis. Reflux esophagitis. 03/28/2006 No. 7029 Microscopically: Stomach ulcer in the acute stage 03/29/2006 No. 1692 In the smear: integumentary pitted epithelium with areas of moderate and severe dysplasia.
03/27/2006 Electrocardiogram Sinus rhythm, normal position of the EOS. Heart rate 85/min.
04/19/2006 Electrocardiogram Sinus rhythm. In comparison with the ECG dated March 27, 2006, the QRST shape is without dynamics. Heart rate 75/min.
03/28/2006 Ultrasound examination of the veins of the lower extremities The deep veins of the sapheno-femoral anastomosis and the trunk of the great saphenous vein are passable in all sections and are completely compressible under compression. Blood flow through the deep veins is spontaneous, synchronous with breathing. Retrograde discharge with proximal compression along the popliteal and posterolateral veins on the left are signs of postthrombotic recanalization. On both sides of the lower leg there are incompetent subcutaneous tributaries of the great saphenous vein. Conclusion: Echo signs of post-thrombophlebic disease of a recanalized form (popliteus-tibial segment) on the left. Small manifestations of varicose veins in the basin of the great saphenous vein on both sides.
03/28/2006 Ultrasound examination of the abdominal organs No. 1239 The liver is homogeneous. Echogenicity is increased. Edge along the costal arch. Gallbladder 85x37 mm. Wall thickness 3 mm. The lumen of the stone is 24 mm. The ducts are not dilated. Common bile duct 5 mm. The pancreas is compacted, not enlarged, without focality. RD 109x49 mm TSP 16 mm RS 114x52 TSP 17 mm The contours of the kidneys are even, the pelvis on the left is expanded to 20 mm. There are no additional formations in the kidneys. The spleen is without features.
03/29/2006. Consultation with a gastroenterologist Diagnosis: Gastric ulcer, first identified in the acute stage, NSAID-associated. Duodenal ulcer, remission. Gallstone disease, chronic calculous cholecystitis without exacerbation. Recommended: Diet No. 5 No-spa 0.04 2 tablets 2 times a day for pain Pancreatin 2 tablets 3 times a day as needed Omez 0.02 1 capsule 2 times a day 30 minutes before meals, 14 days, then 1 capsule in the morning when taking NSAIDs Amoxicillin 0.5 1 capsule 4 times a day, 7 days Clarithromycin 0.5 1 capsule 2 times a day, 7 days.
03/30/2006 Consultation with a neurologist Diagnosis: Spondylosis of the thoracic and lumbar spine, osteoporosis with chronic pain syndrome. Recommended: Calcemin 1 tablet 2 times a day Trental 2.0 No. 10 IV drip Mexidol 2.0 No. 10 IV jet Actovegin 5.0 No. 10 IV jet Milgamma 2.0 No. 10 IM every other day .
03/31/2006 Consultation with a therapist
Diagnosis: ischemic heart disease, aortic atherosclerosis, combined aortic disease. CHF stage I Hypertension II stage. II Art. risk IV. Damage to blood vessels of the heart and brain. Stomach ulcer. Obesity III degree. Recommended: Table No. 10 Enap 0.01 1 tablet 2 times a day Atenolol 0.05 1 tablet 2 times a day Indapamide 0.0025 1 tablet in the morning.
The final diagnosis and its rationale.
Based on the patient’s complaints, on the basis of the medical history, on the basis of objective examination data, as well as data from laboratory and instrumental research methods, as well as consultations with specialists: 03/29/2006 X-ray of the spine, knee joints, hip joints No. 1259. Conclusion: Deforming arthrosis of the hip joints : right III art., left I art. An x-ray of the lumbar spine reveals diffuse osteoporosis and pronounced manifestations of spondylosis deformans in the form of osteophytes on the lateral and anterior surfaces of the vertebral bodies. An x-ray of the knee joints shows bone ankylosis on the left, and moderately pronounced manifestations of deforming arthrosis in the form of narrowing of the joint space on the right. 03/29/2006. Consultation with a gastroenterologist Diagnosis: Gastric ulcer, first identified in the acute stage, NSAID-associated. Duodenal ulcer, remission. Gallstone disease, chronic calculous cholecystitis without exacerbation. 03/30/2006 Consultation with a neurologist Diagnosis: Spondylosis of the thoracic and lumbar spine, osteoporosis with chronic pain syndrome. 03/31/2006 Consultation with a therapist Diagnosis: IHD, aortic atherosclerosis, combined aortic disease. CHF stage I Hypertension II stage. II Art. risk IV. Damage to blood vessels of the heart and brain. Stomach ulcer. Obesity III degree. A final diagnosis can be made: Main diagnosis: Bilateral coxarthrosis on the right, stage III, on the left, stage I. Mixed contracture of the right hip joint. Concomitant diseases: Osteochondrosis. Spondylosis of the thoracic and lumbar spine, osteoporosis with chronic pain syndrome. Coronary heart disease, aortic atherosclerosis, combined aortic disease. Chronic heart failure stage I Hypertension II stage. II Art. risk IV. Gastric ulcer in the acute stage, duodenal ulcer in remission. Cholelithiasis. Chronic calculous cholecystitis in remission. Obesity III degree. Treatment plan
Endoprosthetics of the right hip joint was performed. In order to prevent a postoperative infectious process, it is necessary to prescribe antibiotics - Cefazolin 1.0 IM 3 times a day. — Metronidazole 100.0 IV drip (prevention of anaerobic infection) — 5NOK 0.05 2 tablets 3 times a day To relieve pain analgesics: — analgin 50% — 2 ml IM — baralgin 5 ml IM For no effect from non-narcotic drugs: - Promedol 2% 1 ml IM To correct metabolic processes, energy-producing drugs are administered: - Glucose 5% - 400 ml Insulin 4 units Vitamin C 6.0 To improve cartilage regeneration, use: - Rumalon 1 ml 3 times in Week. A course of 25 injections, the course is repeated 2 times a year. For the treatment of concomitant pathologies: For pain in the abdominal area: - No-spa 0.04 1 tablet 3 times a day. Enzyme preparations: - Pancreatin 2 tablets 3 times a day. For the treatment of peptic ulcers: - Omeprazole - 0.02 1 capsule 2 times a day. — Clarithromycin 0.25 2 capsules 2 times a day. — Metronidazole 0.5 1 tablet 2 times a day. For the treatment of hypertension: - Indapamide 0.0025 1 tablet in the morning. — Enap 0.01 1 tablet 2 times a day. To improve microcirculation in the vessels: - Trental 2.0 No. 10 IV drip - Mexidol 2.0 No. 10 IV jet - Actovegin 5.0 No. 10 IV jet
Preoperative epicrisis Patient Solomatina L.P. was admitted to the 17th trauma department with complaints of pain in the hip joints, pain on the outer surface of the right thigh; pain in the right knee joint; tingling sensation in right thigh; restriction of movement in the right hip joint. Diagnosis: Bilateral coxarthrosis on the right, stage III, on the left, stage I. Mixed contracture of the right hip joint. Studies were carried out: General blood test Erythrocytes, x1012/l Hemoglobin, g/l Ht Color indicator Leukocytes, x109/l Eosinophils, % P/I, % S/I, % Lymphocytes, % Monocytes, % ESR 03/28/06 4.6 144 0.94 6.9 — — 58 33 9 28 04/25/06 4.5 144 General urine analysis Specific weight Reaction Color Transparency Protein, g/l Flat epithelium in the p/z Leukocytes in the p/z Erythrocytes in the p/z Oxalates Mucus 03/28/06 1020 acidic Yellow. transparent 0 3-4 5-6 0-1 04/25/06 1020 acidic S/w transparent 0 2-4 Unit. 1-2 Blood test for group and Rh factor: Conclusion: 0(I) Rh+ Blood glucose 4.6 mmol/l 03/28/2006 Biochemical blood test Protein: 76 g/l Total bilirubin - 12.4 µmol/l direct - 2.4 µmol/l indirect – 10.0 µmol/l Urea: 4.8 mmol/l AST: 1.40 µmol/l ALT: 1.37 µmol/l Residual nitrogen: 17.4 mmol/l Creatinine: 0 .05 µmol/l 03/28/2006 Coagulogram Fibrinogen - 3.77 g/l Fibrinolytic activity 12' Plasma tolerance to hepatitis - 7' Thrombin time - 16' Fibrinase activity 60% Prothrombin index 0.76 03/28/2006 Blood test for RW Conclusion : RW negative 03/29/2006 X-ray of the spine, knee joints, hip joints No. 1259. Conclusion: Deforming arthrosis of the hip joints: on the right, stage III, on the left, stage I. The patient was consulted by a neurologist, therapist, and gastroenterologist. Treatment was carried out: No-spa 0.04 2 tablets 2 times a day for pain Pancreatin 2 tablets 3 times a day as needed Omez 0.02 1 capsule 2 times a day 30 minutes before meals, 14 days, then 1 capsule in the morning for taking NSAIDs Amoxicillin 0.5 1 capsule 4 times a day, 7 days Clarithromycin 0.5 1 capsule 2 times a day, 7 days. Calcemin 1 tablet 2 times a day Trental 2.0 No. 10 IV drip Mexidol 2.0 No. 10 IV jet Actovegin 5.0 No. 10 IV jet Milgamma 2.0 No. 10 IM every other day. Enap 0.01 1 tablet 2 times a day Atenolol 0.05 1 tablet 2 times a day Indapamide 0.0025 1 tablet in the morning. Positive dynamics were noted against the background of the treatment. It is planned to perform endoprosthesis replacement of the right hip joint with the SFEN endoprosthesis. Cement fixation of components.
Progress of the operation
Operation No. 248. Primary total arthroplasty of the right hip joint with the SFEN endoprosthesis, cemented fixation of the components. In the position on the left side under spinal anesthesia, after treating the surgical field with antiseptics, a direct lateral skin incision was made along the outer surface of the thigh in the projection of the hip joint 14 cm. The edges of the wound were covered with material. Soft tissues and the capsule are dissected using the Harding approach. After mobilization of the proximal femur, the femoral head is dislocated from the socket. The head is sharply deformed, articular cartilage is practically absent. The femoral medullary canal was opened through the pyriform fossa, the canal was processed using a reamer, and a template for resection was installed. The head is reserved according to the template. The proximal part is retracted posteriorly and the edges of the acetabulum are excised. They are deformed. The cavity is processed with mushroom-shaped cutters to the bleeding bone to size No. 54. test cup No. 52, satisfactory standing, complete coverage. Severe osteoporosis of the acetabulum, several cysts were opened, curettage of the cyst cavity. 6 milling recesses were formed in the acetabulum, and a cup No. 5 with cement fixation was implanted. The proximal femur is sequentially processed with a figured rasp to size No. 7. Standing No. 7M is satisfactory. Try-in head XL. Test reduction - full movement, no tendency to dislocation. There is no impingement syndrome, the offset is sufficient. Installed SFEN leg No. 7M size, cement fixation, head CoCr 28 No. XL. The head is set into the acetabulum. X-ray control - the position is correct. The wound was washed twice with antiseptics, dried, active drainage. It is sutured in layers. Aseptic dressing. Elastic bandages for both limbs. The leg is placed in a derotation splint. Blood loss 250 ml.
Prescriptions Local cold # Metrogyl 100 ml IV drip # Cephabol 1.0 2 times a day IM # 5NOK 2 tablets 3 times a day # Vitamin E 2.0 IM # Glucose 5% -400.0 Insulin 4 units Vitamin C 6.0 IV drip. # Glucose 5% -400.0 Insulin 4 units Vitamin C 6.0 IV drip. # Promedol 2% - 1 ml IM # No-Spa 0.04 2 tablets 2 times a day # Pancreatin 2 tablets 3 times a day as needed
Diaries: 04/27/2006 Complaints of severe pain in the area of the right hip joint. Blood pressure 13/70 mmHg. Pulse 75/min. Vesicular breathing. There is 250 ml of bloody discharge through the drainage. The drainage was removed and an aseptic dressing was applied. A reaction to glucose developed—convulsive syndrome, hyperthermia. Calcium chloride, prednisolone 60 mg, dibazol 1%-10 ml were administered intravenously; IM analga 50% -2 ml, diphenhydramine 1 ml. The reaction was stopped. 04/28/2006 Complaints of moderate pain in the area of the right hip joint. Blood pressure 150/85 mmHg. Pulse 82. Vesicular breathing. The belly is rounded and symmetrical. On superficial palpation the abdomen is soft and painless. 05/2/2006 No complaints. The condition is satisfactory. Vesicular breathing. Heart sounds are muffled. Blood pressure 130/80. Pulse 76. The abdomen is round, symmetrical. On superficial palpation the abdomen is soft and painless. 05.3-5.2006 state without significant dynamics. 6.05.2006 No complaints. The condition is satisfactory. Vesicular breathing. Heart sounds are muffled. Blood pressure 140/90. Pulse 82. The abdomen is round, symmetrical. On superficial palpation the abdomen is soft and painless. Walking for 10 minutes 7 times a day was prescribed.
Rehabilitation after endoprosthetics
In articles devoted to modern studies of the dependence of quality of life indicators on the volume of rehabilitation, doctors insist on the use of a wide range of restorative measures immediately after endoprosthetics.
After endoprosthetics, it is important to use auxiliary devices during the rehabilitation period
Rehabilitation of the patient starts on the second day after the intervention under the supervision of a physical therapy methodologist. Doctors provide the patient with physical activity as early as possible (teach him how to get out of bed correctly, move around the bed with assistive devices).
After discharge home, a period of adaptation to the foreign body begins (4–6 weeks). This period is necessary for final scarring of the joint capsule and resorption of the postoperative hematoma.
General recommendations
At home, the patient should follow the following recommendations:
- Walk on crutches without stepping on the operated limb.
- Perform at least three from the proposed list of exercises aimed at strengthening the thigh muscles (in particular the quadriceps).
- Wear compression stockings to prevent thromboembolism for one month.
- Stick to a diet that prevents weight gain.
- Systematically take prescribed medication.
Exercises
Exercises should be performed 6–8 times a day, starting with 10–20 repetitions and gradually increasing them to 50–70. Regular and systematic exercise therapy classes guarantee a quick return to work capacity.
Exercises must be performed under the guidance of an instructor
Types of exercises:
- bending the leg at the knee up to 80% while lying on the bed and straightening it to a straight position, without lifting the heel from the bed;
- extension at the knee joint to a level position by raising the foot (there should be a roller 25–40 cm high under the knee);
- knee extension while sitting on the edge of the bed (imitation of hitting a ball).
Massage
The massage procedure for DOA of the hip joint provides:
- decreased tone of tense muscles;
- increased contractility of weakened muscles;
- improvement of blood circulation, nutrition and regeneration in the joint;
- weakening of neurological manifestations.
At home, the patient can massage the area of the joint and adjacent muscles independently (avoiding the incision area) or seek the help of a professional. It is optimal to start with procedures lasting 10–15 minutes 2–3 times a day. The massage should be stopped immediately if discomfort occurs.
The question of the possibility of doing without crutches and full weight-bearing of the operated limb is decided at a follow-up consultation with an orthopedic surgeon after 8–10 weeks.
Gymnastics for pathology
Gymnastics plays a key role in treatment. improving the well-being and rehabilitation of a patient with coxarthrosis of the hip joint. The procedures strengthen muscles, improve movement and relieve pain. The doctor recommends specific types of classes, and he also prescribes the frequency and duration of the procedures.
The following exercises are recommended:
- bending the body straight and towards each leg;
- swing your legs;
- alternately bending the leg and lifting it at a right angle;
- abducting movements of the leg;
- swing your leg from a position lying on your side;
- lifting bent legs while lying on your back;
- bend straight towards each leg while sitting on the floor.
It is advisable to do these exercises in combination with others to generally strengthen the body.