m2s
m2s
Rating: -,-
Rating: -,-
m2s
Other items
Disable advertising
Osteology and arthrology
The bones of the forearm are represented by the ulna, located medially, and the radius, located laterally. This article presents the anatomy of the radius and ulna.
Connection of the bones of the forearm
The head of the radius and the radial notch of the ulna form the articulatio radioulnaris proximalis, which is described with the elbow joint because it is part of it, and is functionally combined with a second similar joint located at the distal end of the forearm.
The distal radioulnar joint (articulatio radioulnaris distalis) is formed by the articular circumference of the head of the ulna and the radial notch. The shape of the joint is cylindrical, movements are possible only along the vertical axis (Fig. 127). Triangular-shaped fibrous cartilage extends from the ulnar notch of the radius to the styloid process of the ulna, which functions as an articular disc (discus articularis). The upper side of the disc limits the cavity of the articulatio radioulnaris distalis, and the lower side - the articulatio radiocarréa.
127. Axes of the upper limb (according to V. P. Vorobyov, G. F. Ivanov). Oo—longitudinal axis of the humerus; eo - longitudinal axis of the ulna; ab - axis of the elbow joint; cd - axis of the wrist joint; ofe - the common axis around which pronation and supination of the entire arm occur; fe is the axis around which pronation and supination of the forearm occur; n — center of rotation in the wrist joint; A - shoulder angle; B - elbow angle
The joint capsule is very loose and much thicker on the dorsal side, attached along the edges of the articular surfaces. Between the radius and ulna bones there is a synovial bursa. There are no ligaments in this joint.
The joints between the forearm bones allow the radius to rotate around the ulna. These movements have already been described - outward rotation (supinatio) and inward rotation (pronatio) (Fig. 128). Both joints always function together, forming a combined joint. A single axis passes through the head and neck of the radius and continues onto the head of the ulna. The radius bone, moving, describes an arc of 140° near the ulna, and the hand moves along with the forearm. If we add the rotation of the humerus to this, we get a total range of movements of about 220-360°, which is very important for performing diverse movements of the upper limb (Fig. 129). The ability of the radius to rotate around the ulna with the help of special muscles, the presence of ligaments that strengthen the proximal radioulnar joint, and the articular disc in the distal radioulnar joint are characteristic only of humans and are associated with his work activity.
128 A. Diagram of the location of the bones of the forearm during pronation and supination (according to Tittel). 1 - ulna; 2 - radius; 3 - m. pronator; 4 - m. supinator
128 B. Diagram of the location of the bones of the forearm during pronation and supination (according to Tittel). 1 - ulna; 2 - radius; 3 - m. pronator; 4 - m. supinator
129. The range of movements of the hand possible during the period of pronation, supination (A, B) and rotation along the longitudinal axis in the shoulder joint (C, D) (according to Lanz-Wachsmuth)
In connecting the bones of the forearm, the interosseous membrane (membrana interossea), consisting of collagen fibers, is of primary importance (Fig. 130). This membrane, stretched between the crests of the ulna and radius, holds them in place without restricting the movements of the radius. In the upper part of the forearm in the interosseous membrane there is a hole for the passage of the posterior interosseous artery. From above, this hole is limited not by a membrane, but by a thickened fibrous bundle called chorda obliqua.
130. Connection of the bones of the forearm. 1 - ulna; 2 - processus styloideus medialis; 3 - discus articularis; 4 - processus styloideus lateralis; 5 - membrana interossea antebrachii; 6 - radius; 7 - chorda obliqua; 8 - tendo m. bicipitis brachii; 9 - lig. anulare radii
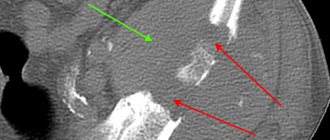
X-rays of the elbow joint
Photographs of the elbow joint are taken in posterior and lateral projections. These images reveal three joint spaces: the humeroulnar, humeroradial, and proximal radioulnar joints. The contours of the articular surfaces are clear and the joint space has the same thickness. In children, ossification nuclei are visible in the humerus, ulna and radius.
Surgery
Sometimes chronic bursitis or septic bursitis may require surgery. In a traditional bunionectomy, an incision is made in the elbow and the inflamed bursa is removed. Since the bursa is located under the skin, the elbow joint is not affected during the operation.
Complications of surgical removal of the bursa may include problems with healing of the skin at the incision site and pain. A few months after the operation, a new bursa usually grows at the site of the removed bursa.
After surgery, patients are recommended to fix their elbow for some time with a special bandage, holding the arm at an angle of 90 degrees.
Exercise therapy. After the symptoms of bursitis subside, it is quite effective to prescribe exercise therapy to strengthen muscle tone.
Fracture of the olecranon
Surgery for olecranon fractures is indicated in the following cases:
- Displacement of bone fragments (displaced fractures)
- Perforations with bone fragments of skin (open fractures)
The operation usually consists of eliminating the displacement of the fragments and creating conditions so that they do not move until fusion occurs.
Due to the high risk of infectious complications with open fractures, surgery should be performed as soon as possible, usually in the first hours after the injury. In the emergency department, such patients are prescribed antibiotic prophylaxis (intravenously) and tetanus prophylaxis. During the operation, the wound and bone fragments are carefully treated. Reduction and fixation of bone fragments are usually performed simultaneously with treatment of the fracture.
Surgical Treatment Options
Open reduction and internal fixation. This is the most common treatment for olecranon fractures. During such an operation, bone fragments are compared with each other and fixed in their normal position with screws, wires, knitting needles or metal plates.
Below are some of the most commonly used methods of olecranon fixation.
Fixation of an olecranon fracture with knitting needles and a tightening wire loop
( Left ) A single screw that is inserted into the medullary canal can be used to fix an olecranon fracture. ( Right ) Fracture fixation with plate and screws.
Bone grafting . In cases of open fractures, some bone fragments may be lost or they may be significantly fragmented. In such cases, bone grafting is necessary to fill the bone defects. Donor bone or the patient's own bone (most often from the pelvic bone) can be used as a plastic material. In some cases, artificial bone substitutes may be used.
Removal of a bone fragment . If the bone fragment is too small and cannot be fixed, sometimes it has to be removed. In this case, the triceps tendon attached to the fragment is refixed to the remaining part of the ulna.
Results of the operation
Most patients return to normal life within approximately 2-3 months after injury, but full recovery may take more than half a year. Restoring strength to the hand often takes longer than expected.
Despite the presence of radiological evidence of fracture healing, many patients still report limited elbow function. Over time, elbow function usually improves in these patients.
Useful information about fractures of the shoulder and forearm bones
What are the types of shoulder fractures?
There are fractures of the proximal and distal epiphysis, as well as the diaphysis. A fracture of the proximal epiphysis of the humerus occurs when falling on the elbow or on an outstretched arm. There are fractures of the head, anatomical neck (intra-articular), transtubercular fractures, fractures of the surgical neck (extra-articular) and avulsions of the greater tubercle of the humerus.
Symptoms of a shoulder fracture
The shoulder joint is enlarged due to swelling and hemorrhage. Movement is limited or impossible due to pain. Tapping the elbow causes pain in the shoulder joint. At the fracture site, pathological mobility and crepitus are determined. Clinical manifestations are less pronounced with an impacted fracture. A diaphysis fracture is the most common fracture of the humerus and accounts for more than 50% of all shoulder fractures. It occurs either from a direct blow to the shoulder or from a fall on the elbow or a sudden movement (throwing a grenade, etc.). In adults, the fracture of the diaphysis of the humerus is always complete (transverse, oblique, helical, comminuted), in children it is subperiosteal. Fractures are most often observed in the middle third of the shoulder, where the diameter of the bone is narrowest.
Symptoms of a shoulder fracture.
Pain, pathological mobility, severe deformation. On palpation, bone fragments can be clearly felt. The radial nerve is often injured, resulting in impaired skin sensitivity and the inability to straighten the fingers. Deformation of the lower third of the shoulder and elbow joint. The forearm is bent, movements in the elbow joint are sharply painful. In transcondylar fractures, the relationship between the lines connecting the condyles and the olecranon is disrupted (compare with the healthy side).
Fracture of forearm bones.
There are fractures of the proximal epiphysis, diaphysis and distal epiphysis. A fracture of the proximal epiphysis is divided into a fracture of the ulnar and coronoid processes of the ulna and a fracture of the head and neck of the radius. These fractures occur mainly when falling on the elbow (blow to the elbow) or an outstretched arm.
Symptoms of a fracture of the forearm bones.
Pain and swelling at the fracture site, impaired limb function. When the olecranon is fractured, the arm is in a semi-bent position (the arm hangs down), the victim supports it with his healthy arm. When the coronoid process is fractured, swelling in the elbow area and pain on palpation is determined. When the head or neck of the radius is fractured, there is sharp pain in the area of the outer elbow and impaired rotational movements of the forearm. Sometimes a bone crunch is felt. The forearm is in a pronated position and bent at the elbow joint.
Fractures of the diaphysis of the forearm bones.
They arise from a direct blow. Fractures of both one and two bones are observed at the same (more often) or at different levels. Sometimes fractures are accompanied by dislocation of the radius. In children, fractures of the forearm diaphysis are usually subperiosteal (“green stick”).
Symptoms of a fracture of the diaphysis of the bones of the forearm.
Pain with axial and frontal load, swelling (when fragments are displaced - deformation), pathological mobility.
Fracture of the distal epiphysis of the forearm bones.
The most common fracture of the forearm bones. It is also called a fracture of the forearm (radius bone) in a typical location. Occurs when a fall lands on an extended (extensor fracture) or bent (flexion fracture) hand. Often accompanied by a separation of the styloid process of the ulna, which leads to the formation of a bayonet-like deformity.
Symptoms of a fracture of the distal epiphysis of the forearm bones.
The presence of a bayonet-like deformity and convexity on the palmar surface, swelling, local pain on palpation and axial load, a sharp limitation of movement in the wrist joint indicates a fracture of the forearm bones at the distal end.
Causes
- Moderate but repetitive trauma is the most common cause. For example, people who lean on their elbows cause friction and mild trauma to the tissue over the olecranon. For example, there are terms such as “student’s elbow,” plumber’s elbow or miner’s elbow, and these terms are based on prolonged support on the elbows.
- Single injuries, such as a blow to the back of the elbow, can cause inflammation.
- Arthritis. One or more bursae may become inflamed as a result of polyarthritis (but most cases of olecranon bursitis are not associated with arthritis).
- Bursa infection. This can happen if there is a cut in the skin over the bursa that allows bacteria to enter.
- Idiopathic. In many cases, bursitis occurs for no apparent reason. However, it is possible that in some cases, bursitis is associated with a minor injury that has been forgotten.
Preolecular bursitis of the elbow joint
This is such a painful lump on the olecranon process, directly on the part of the elbow on which we rest. The size resembles a quail egg or a small plum. The cause is most often long-term compression of the olecranon process as a result of leaning on a table or handrail. As a result of such pressure, the skin on the elbow can be punctured by crumbs of some material, which leads to inflammation. Overstrain of the extensor muscles that attach to the elbow can also lead to such inflammation.
Under the skin of the olecranon there is a sliding bursa - this is a bag with synovial fluid that allows the skin to glide over the bone to avoid injury when resting on the elbow. When it becomes involved in the process of inflammation, excess fluid production occurs in it, which leads to deformation and swelling. If the skin is damaged by a foreign body, the bursa becomes infected, and as a result, purulent inflammation of the sliding bursa occurs. This disease is called purulent bursitis.
Serous bursitis is treated by puncture and administration of glucocorticoids. The necessary goal of treatment is to stop excess inflammation with fluid production; single injections of hormonal drugs in this case are most preferable. There is still insufficient data on the use of PRP therapy in the treatment of preolecular bursitis. There are several questions here: the injection volume with prp is 6.5 ml, which will fill the bursa and neutralize the result of treatment - the bursa will remain the same size, synovitis is a contraindication for PRP therapy. But the question remains open; it is very likely that the use of small volumes of prp and infiltration of the peri-bursal space will have a beneficial effect on completing the inflammation process. In addition, practice shows that prp therapy “dries out the joint” and small amounts of synovitis are stopped. So in the process of practicing the treatment of preolecranial bursitis prp, the advantage of plasma therapy over the administration of glucocorticoids is manifested. As an addition to treatment, compresses based on dimexide with the addition of anesthetics and non-steroidal anti-inflammatory drugs can be used.
Purulent bursitis with arthrosis of the elbow joint requires a course of treatment with antibacterial drugs and washing the bursa cavity with antiseptics. If surrounding tissues - subcutaneous tissue and fascia - are involved in inflammation, the abscess is opened and bandaged until the wound heals. Against the background of elbow arthrosis, if treatment with conservative methods of chronic bursitis is unsuccessful, the preolecular bursa is excised in an orthopedic hospital. Other pathologies of the elbow joint, excluding injuries, are much less common, including arthrosis of the elbow joint.
Bones and their connections
Musculoskeletal system
We are opening a new chapter of anatomy dedicated to the musculoskeletal system. It is he who provides support for the body, maintains body parts in the required position, serves as protection for internal organs and provides locomotor function - movement.
Bones are the basis of the musculoskeletal system, which we are beginning to study. Osteology (from the Greek osteon - bone) is a branch of anatomy devoted to the study of bone tissue, individual bones and the skeleton as a whole.
In addition to what you learned about the structure of bones in the “connective tissues” section, there are a number of important points that I will draw attention to in this article.
The skeleton and joints are the passive part of the musculoskeletal system, the muscles are the active part. By contracting, the muscles change the positions of the bones - various movements occur.
Bone structure
Bone consists of organic and inorganic substances. Organic substances are represented by ossein (from the Latin os - bone), inorganic substances - calcium phosphate. The elasticity of bones is due to ossein, and the hardness is due to calcium salts. Normally, this ratio represents balance.
In children, bones are more elastic and resilient than in adults: organic substances predominate in them. In the bones of older people, the content of both the organic component and the inorganic component—calcium salts—is reduced, which is why the bones of the elderly are fragile and susceptible to fractures.
The compact substance of the bone is formed by bone plates that fit tightly to each other and form osteons (structural units of the compact substance of bone tissue). The compact substance gives bone strength.
The substantia spongiosum also contains bony plates, but they do not form osteons, making the substantia spongiosum less strong than the substantia compacta. In the spongy substance between the bone crossbars (bone beams) there is red bone marrow.
In the red bone marrow, the initial stages of development of the formed elements of blood take place: red blood cells, leukocytes, and platelets appear here.
Yellow bone marrow (adipose tissue) performs a nutritional function: nutrients - fats (lipids) - accumulate here. In case of large blood loss, yellow bone marrow can be replaced by red bone marrow cells.
Yellow bone marrow is localized in the bone marrow cavities (medullary canal) of tubular bones (in the diaphysis).
So, let's summarize. The spongy substance is the location of the red bone marrow, the central hematopoietic organ. The cavities of the tubular bones contain yellow bone marrow, which performs a nutritional function and can be replaced by red bone marrow cells in case of large blood losses.
The structural unit of the compact bone substance is the osteon, or Haversian system. The osteon canal (Haversian canal) contains blood vessels and nerves. Osteons are located in the direction of the force, which determines the mechanical strength of the bone.
The main cells of bone tissue that we studied in the section “connective tissues”: osteoblasts, osteocytes and osteoclasts. Osteocytes have a process form and are located around the Haversian canal.
Classification of bones
Bones are divided into:
- Tubular
- Spongy
- Mixed
- Flat (wide)
The bones are cylindrical in shape, most often their length is greater than their width. The cavity of the long bones contains yellow bone marrow.
The long tubular bones include the femur, fibula and tibia, humerus, radius and ulna. The short ones include the metatarsal and metacarpal bones, the phalanges of the fingers. When moving, the tubular bones perform functions like levers that move muscles.
The width of the spongy bones is approximately equal to the length. Spongy bones are covered on the outside with a layer of compact substance and consist of spongy substance, which contains red bone marrow.
Spongy bones: sternum ( flat
spongy bone), ribs (
flat
spongy bones), carpal and tarsal bones. The clavicle is a spongy bone in structure, but in shape it is a tubular bone.
These bones are characterized by a complex shape, and during development they are usually formed from several parts. These include the vertebrae (a vertebra is a mixed spongy bone), the sacrum, and the hyoid bone. By origin, the clavicle also belongs to mixed bones.
The area of flat bones significantly prevails over the width. Flat bones are similar in structure to spongy bones.
The flat bones are: parietal, frontal, temporal and occipital (bones of the cranial vault), scapula, sternum, ribs, pelvic bone.
The structure of the tubular bone
Using the example of a tubular bone, we will analyze the parts into which the bone is divided. The surface of the bone is covered with periosteum - tissue that surrounds the bone and firmly fuses with it. In the thickness of the periosteum lie blood vessels and nerves that give branches inward.
Remember that bone growth in thickness occurs precisely thanks to the periosteum: its inner layer of cells divides, and the thickness of the bone increases. Thus, the periosteum performs a number of important functions:
- Protective - the outer layer is dense, protects the bone from damage
- Nutritional (trophic; Greek trophe - food, nutrition) - vessels pass through the thickness of the periosteum to the bone
- Nervoregulatory - nerves pass through the thickness of the periosteum
- Bone formation - bone growth in thickness
Let's move directly to the structure of the bone. The diaphysis (Greek diaphýomai - to grow between) is the body of the bone, usually the diaphysis is cylindrical or triangular. The epiphysis (from the Greek epiphysis - growth, lump) is the thickened end of a long tubular bone. The area of bone between the epiphysis and diaphysis is the metaphysis (Greek meta - after, after, through).
In the diaphyses, compact bone substance predominates, in the epiphyses - spongy. These terms are easy to explain and remember with a picture, so make a diagram and you'll learn them quickly 
Pay special attention to the fact that bone growth in length is due to the epiphyseal plate. It is due to this plate, located between the metaphysis and epiphysis, that the bone grows in length. The epiphyseal plate is well supplied with blood.
Bone connections
Bones can be fixedly connected to each other: pelvic bones (ilium, pubis, ischium), skull bones (except for the lower jaw), sacral vertebrae, coccyx.
Semi-movable ones include: connections of the cervical, thoracic and lumbar vertebrae, connections of the ribs with the sternum. Intervertebral discs perform a shock-absorbing function (French amortir - to weaken, soften) - they evenly distribute the load on the vertebrae, ensuring flexibility and mobility of the spine. Pay special attention to the fact that the pubic bones are semi-movably connected to each other: they form the pubic symphysis.
Joint (synovial joint - Greek sýn - together + Latin ovum - egg) is a movable connection of the bones of the skeleton. The science of joints is arthrology (Greek arthron - joint + logos - study). Ligaments - dense formations of connective tissue - strengthen the joint from the inside and outside (ligaments are intra-articular and extra-articular).
The surfaces of the bones in the joint (called articular surfaces) are covered with hyaline cartilage, which reduces friction between the bones and performs a shock-absorbing function - evenly distributing pressure.
The joint capsule (capsule) is attached to the articular surfaces or in their vicinity, surrounding the articular cavity (cleft-like space). The inside of the joint capsule is covered with a synovial membrane, which secretes synovial fluid. Synovial fluid fills the joint cavity, nourishes the joint, moisturizes it, and eliminates friction of the articular surfaces.
Movably connected in the human skeleton are: lower jaw + temporal bone, clavicle + scapula (the joint is inactive), femur + pelvic bone (hip joint), humerus + ulna + radius (elbow joint), femur + tibia + patella (knee joint) , lower leg and foot (ankle joint = tibia + fibula + talus), phalanges.
Normally, the bones can shift relative to each other in the joint, but with an injury or too sudden and strong movement, this displacement can be too strong: as a result, the contact of the articular surfaces is disrupted. In this case, they talk about the occurrence of a dislocation.
Dislocation is a displacement of the articular ends of bones, either with or without disruption of the integrity of the articular capsule.
Techniques for providing medical care for dislocations:
- Immobilization (lat. immobilis - motionless) of the injured limb using scarves, splints (supporting fastenings), by bandaging the limb to a healthy part of the body
- Apply cold to the affected area, give painkillers (after making sure there is no allergy)
- Take the victim to a doctor or call an ambulance
Before reducing a dislocation, an x-ray should be taken to ensure there are no bone fractures, which sometimes accompany a dislocation.
Bone fractures
A bone fracture is a partial or complete disruption of the integrity of a bone resulting from a load that exceeds the strength of the injured area.
Fractures are divided into:
- Open - a wound is localized above the fracture, penetrating or not penetrating to bone fragments
- Closed - a fracture without damage to the skin above it
Techniques for providing medical care for fractures:
- Call an ambulance
- If there is bleeding, it must be stopped immediately by applying a tourniquet.
- In case of damage to the skin, apply an aseptic bandage using a bandage or clean cloth.
- Give the victim a painkiller, making sure he does not have allergies
- Immobilize (immobilize) the injured limb with special splints, fix the joints above and below the fracture site. For immobilization, you can use available means (sticks, boards, rods, etc.)
© Bellevich Yuri Sergeevich 2018-2021
This article was written by Yuri Sergeevich Bellevich and is his intellectual property. Copying, distribution (including by copying to other sites and resources on the Internet) or any other use of information and objects without the prior consent of the copyright holder is punishable by law. To obtain article materials and permission to use them, please contact Yuri Bellevich
.
Publications in the media
Fractures of the forearm bones account for 11.5–30.5% of the total number of closed injuries. Classification • Fracture of the olecranon process • Fracture of the coronoid process • Fracture of the head and neck of the radius • Isolated fracture of the ulna • Isolated fracture of the radial shaft • Fracture of both bones of the forearm • Fracture of the ulna with dislocation of the head of the radius • Fracture of the radius with dislocation of the head of the ulna • Fracture of the radius “in a typical location.”
Fracture of the olecranon • Causes: direct trauma, sudden contraction of the triceps brachii muscle • Clinical picture : swelling of the elbow joint, the arm is straightened, hanging; passive movements cause pain, active extension in a displaced fracture is impossible, Huether's triangle is deformed, the apex of the olecranon is above the line connecting the epicondyles of the shoulder • Treatment •• Non-displaced fractures: plaster cast for 3-4 weeks in the position of flexion of the forearm at the elbow joint 90–110°, in the middle position between pronation and supination •• Fracture with a displacement of more than 5 mm - osteosynthesis •• Exercise therapy. Fracture of the coronoid process • Cause : fall on a bent elbow • Clinical picture : swelling and hematoma on the anterior surface of the elbow joint, limited maximum flexion of the forearm, local pain on the inner surface of the cubital fossa • Treatment. Plaster splint in the position of bending at a right angle for 3–4 weeks, for large fragments - osteosynthesis. Fracture of the head and neck of the radius • Cause : fall on an outstretched arm • Clinical picture : swelling and pain over the humeroradial joint, limited extension, severe pain during outward rotation of the forearm and axial load • Treatment. For non-displaced fractures, use a plaster splint with the forearm flexed at 90–100° for 3 weeks. In case of displacement - osteosynthesis or removal of the head of the radial bone (if reposition is ineffective, fragmentation of the head).
Isolated fracture of the ulna diaphysis • Cause : direct trauma • Clinical picture . Deformation, swelling, local pain, pathological mobility, severe pain with axial load and compression from the lateral surfaces of the forearm, active movements in the elbow joint are limited • Treatment. Plaster cast for 4-6 weeks in the position of flexion of the forearm at a right angle in the middle position between supination and pronation. If fragments are displaced - preliminary reposition, fixation for up to 6 weeks. Isolated fracture of the radial diaphysis • Cause : direct trauma • Clinical picture . Deformation, swelling, local pain, pathological mobility, severe pain with axial load, rotation and compression from the lateral surfaces of the forearm, lack of active pronation and supination • Treatment . For fractures in the upper and middle thirds - a plaster cast in the position of flexion of the forearm at a right angle and in the position of supination. For fractures in the lower third, a plaster cast is placed in the middle position between pronation and supination. Immobilization for 4–5 weeks. If fragments are displaced - preliminary reposition, fixation for up to 6 weeks. Fracture of both bones of the forearm • Frequency - 53% of all fractures of the bones of the upper limb • Cause: direct and indirect injuries • Pathomorphology. Characteristic is the convergence of fragments of the radius and ulna due to contraction of the interosseous membrane • Clinical picture . The patient fixes the injured arm with his healthy hand. Characterized by deformation and shortening of the limb, sharp pain on palpation, axial load, compression of the forearm at a distance from the fracture, pathological mobility • Treatment •• For fractures without displacement - a splint-circular plaster cast in the middle position of the forearm between supination and pronation, dorsal flexion of the hand under at an angle of 25–35° for up to 8 weeks •• For displaced fractures - immediate reduction manually or using a distraction device, fixation with a plaster cast for 8–10 weeks, transosseous compression-distraction osteosynthesis •• For fractures in the upper third, the arm is immobilized in position maximum supination, in the middle third - in the semi-pronation position, in the lower third - reduction in the pronation position, then transferred to the semi-pronation position •• Surgical treatment (osteosynthesis) is indicated for interposition of soft tissues, displacement of fragments by more than half the diameter, secondary and angular displacement bones. Immobilization in the postoperative period in the position of flexion of the forearm at a right angle for a period of up to 10–12 weeks.
Fracture of the ulna with dislocation of the head of the radius (Montagia fracture) • Causes: falling on the hand, reflecting a blow with the forearm bent forward and upward • Pathomorphology. There are flexion (the head of the radius is displaced anteriorly, fragments of the ulna are displaced posteriorly; an angle open anteriorly is formed) and extension (the head of the radius is dislocated posteriorly and outward, fragments of the ulna are displaced anteriorly; an angle open posteriorly is formed) fractures • Clinical picture . Characteristic deformity (retraction on the side of the ulna and bulging on the side of the radius), shortening of the limb, detection of a fracture of the ulna and dislocated head of the radius on palpation, lack of active movements, pain and spring resistance during passive flexion. Possible damage to the radial nerve. Mandatory radiography is required, including the elbow joint and the area of the fracture • Treatment •• Flexion fracture - reposition and reduction of the dislocation in the extension position, fixation of the limb in the position of extension of the arm and supination of the forearm for 6–8 weeks. If immediate reposition is not possible - surgical reduction of the dislocation and osteosynthesis •• Extensor fracture - reposition and reduction of the dislocation in the supination position, plaster cast (4-5 weeks in the supination position, 4-6 weeks in the middle position between supination and pronation). Surgical treatment when immediate reposition is impossible (rupture of the annular ligament, interposition of soft tissues). Fracture of the radius with dislocation of the head of the ulna (Galeazzi fracture) • Causes: fall on an outstretched arm, blows to the forearm • Pathomorphology: the radius breaks in the lower third, its fragments are displaced anteriorly (the distal fragment additionally takes a pronation position due to muscle contraction) , forming an angle open posteriorly; the head of the ulna moves to the palmar or dorsal side • Clinical picture : characteristic deformation (recession on the dorsum of the forearm on the radial side and protrusion on the palmar side), curvature of the axis of the radial bone, the head of the radial bone is palpated on the ulnar side of the wrist joint, pain on palpation and axial load. Pressure on the head of the radius causes reduction; when the pressure stops, the head dislocates again. It is mandatory to carry out radiography with capture of the wrist joint • Treatment: reposition, plaster cast for 8–10 weeks, if conservative treatment is ineffective - open reduction and osteosynthesis of the radius, open reduction of the head of the ulna.
A “typical location” radius fracture is a fracture of the radius 2–3 cm proximal to the articular surface • Frequency. 15–20% of all fractures. In elderly women, it occurs 2–3 times more often than in men • Causes: falling on an outstretched arm with a bent hand • Pathomorphology •• When falling on the hand in extension, an extensor Collis fracture occurs - the distal fragment is displaced to the dorsal and radial side and supinates , the central one is displaced to the palmar-ulnar side •• When falling on the hand in a position of palmar flexion, a flexion Smith fracture occurs - the distal fragment is displaced to the palmar side and pronates, the central fragment is displaced to the dorsal side and supinates • Clinical picture : fork-shaped or bayonet-shaped deformity, with a fracture In Collis's fracture, the distal fragment is palpated on the dorsal surface, the proximal fragment is palpated on the palmar surface; with a Smith fracture, the distal fragment is palpated on the palmar surface, and the proximal fragment is palpated on the dorsal surface; sharp pain on palpation of the radius and styloid process, axial load. The median nerve, interosseous branches of the median and radial nerves are often damaged (Turner's neuritis) - sharp pain, paresthesia, zones of anesthesia, osteoporosis of the hand bones, restriction of movement of the fourth finger • Treatment •• Fracture without displacement - plaster splint (forearm in the middle position between supination and pronation, hand - slight dorsiflexion) for 3-4 weeks •• Displaced fractures - manual or hardware reduction, plaster cast for 4-5 weeks •• Turner's neuritis - B vitamins, neostigmine methyl sulfate, anabolic hormones, thyrocalcitonin, intraosseous procaine .
ICD-10 • S52 Fracture of the bones of the forearm
Treatment
In most cases, elbow bursitis can heal on its own by reducing the stress on the elbow. But in some cases, medical intervention, including surgery, is required.
Conservative treatment of elbow bursitis includes:
- Rest and change in activity. Patients with elbow bursitis should avoid activities that put pressure on the elbow. Wearing elbow pads can also help protect the elbow bursa from pressure or additional irritation.
- Cold. Applying a cold compress to a swollen elbow for 20 minutes two or three times a day can help relieve symptoms and reduce swelling.
- Compression. Using an elastic bandage wrapped around the affected joint can help reduce swelling.
- Elevation. Elevating the elbow to or above heart level reduces blood flow and thereby reduces inflammation.
Drug treatment. Nonsteroidal anti-inflammatory drugs such as aspirin, ibuprofen (such as Advil), naproxen (such as Aleve), and COX-2 inhibitors (such as Celebrex) can reduce swelling and inflammation and relieve pain associated with elbow bursitis.
Aspiration. Aspiration of the swollen bursa using a needle and syringe relieves the pressure immediately. Aspiration is also done to test the fluid for microbes. (A positive test would indicate septic bursitis).
Corticosteroid injections. Symptoms of bursitis can be significantly reduced with corticosteroid injections. Corticosteroids are powerful anti-inflammatory drugs, and injecting them directly into the inflamed bursa usually significantly reduces pain and swelling. However, corticosteroid injections have potential side effects such as infections and degeneration of the skin on the elbow. Thus, these injections are usually prescribed for persistent bursitis and other treatment is not effective.
Antibiotics. Septic olecranon bursitis requires antibiotics. The choice of antibiotic depends on the microorganism that is causing the infection (most often Staphylococcus aureus). For most people with septic bursitis, treatment with antibiotics is quite effective, with some requiring hospitalization and intravenous antibiotics.