A forearm fracture is a common traumatic injury to the hand caused by intense force on the bone. The appearance of the disorder may be associated with a blow from a heavy object or a fall on the forearm. The risk of fractures increases with the presence of systemic diseases.
Anatomy of the forearm.
The forearm consists of two bones - the ulna and the radius.
If you stretch your arms forward with your palms up, the ulna will be on the little finger side, and the radius will be on the thumb side. The ulna widens at the elbow, and the radius widens towards the wrist. The main movement performed by the forearm is rotation. In this case, the ulna is rigidly fixed in a block with the humerus, and the radius rotates around it. This movement occurs, for example, when screwing in a light bulb or opening a door with a key.
In some cases, significant displacement of the fragments occurs, as a result of which they perforate the skin. This type of fracture is called open, and it requires immediate surgical intervention, as it is characterized by a high risk of infectious complications.
First aid for fractured forearm bones
The algorithm of actions when a fracture of the forearm bones is detected involves:
- Immobilization (immobilization) of a limb using a splint. You can make a retainer from scrap materials if you have a solid piece of box, a board or stick, a bandage or a long piece of cloth. Help consists of applying a splint to the shoulder, elbow and wrist joints. The splint will immobilize the arm and relieve additional stress from the injured limb;
- Taking painkillers. It is forbidden to take alcohol to relieve pain, since its influence can aggravate the condition of the victim;
- Application of a hemostatic bandage for an open fracture. If a person is bleeding, it should be stopped using a pressure bandage. The wound must be bandaged tightly. If arterial bleeding is observed, a tourniquet is applied to the shoulder.
Symptoms of a forearm fracture in the middle third.
Symptoms of a forearm fracture in the middle third are standard for any fracture - pain, swelling, bruising, bone crepitus, deformity, impaired hand function.
With open injuries, a violation of the integrity of the skin also occurs. With very severe soft tissue damage, the fracture can be complicated by the occurrence of compartment syndrome, in which high interstitial pressure leads to irreversible damage to muscle tissue. In any case, if you have the above symptoms, you should immediately consult a traumatologist.
Fracture of the forearm with and without displacement
A forearm fracture is a common hand injury that occurs as a result of strong physical impact on the bone, when hit by a heavy object, or falling on the forearm from an incorrect body position.
There is also a pathological fracture, in which a strong mechanical load is not needed to break the integrity of the bone of the forearm.
Due to weakened bone tissue as a result of the development of such serious diseases as osteochondrosis, osteomyelitis, rickets, a sudden movement of the hand is enough for a fracture.
Types of injury
A fracture of the forearm bones may differ in the nature of the symptomatic picture, depending on the location of the fracture, the presence or absence of displacement. Fractures of the forearm bones are divided into several types, depending on their nature:
- Depending on the degree of damage to the skin, the injury can be open or closed. The most difficult clinical case is an open form, accompanied by rupture of tissue and skin. Accompanied by external bleeding.
- Depending on the complexity, the injury can be displaced or non-displaced. Injury to the forearm with displacement causes complications, since bone fragments can damage nerve roots or blood vessels.
- Based on the number of injured bones and the nature of their fracture, the injury can be splintered, zigzag, or multiple.
Treatment of fractures of the middle third of the forearm.
Fractures of both forearm bones in the middle third in adults should almost always be treated surgically. In a cast it is impossible to adequately compare bone fragments in a fracture of the forearm in the middle third, and even if it is possible, secondary displacement always occurs. This subsequently leads to dysfunction of the limb. Plaster immobilization is almost always used as a temporary measure to prevent secondary displacement, perforation of the skin with bone fragments, damage to the neurovascular bundles, and reduce pain. Surgical treatment is currently most often represented by open reduction and osteosynthesis with plates. In some cases, closed osteosynthesis with locking pins, wires, or flexible rods can be used, and in open fractures, it is preferable to apply an external fixation device. In children, this group of fractures can be treated conservatively if adequate reduction can be achieved in a plaster cast.
Below is a clinical example of the treatment of a patient with a forearm fracture.
Patient X. Trauma at home, fell on a curb, received a closed fracture of both bones of the right forearm with displacement, rupture of the distal radio-ulnar joint. I contacted the RTP and x-rays were taken. A plaster cast was applied.
The patient contacted K+31; given the nature of the fracture, the patient was offered surgical intervention.
Intraoperative assessment of the stability of the distal radioulnar joint.
Osteosynthesis of both bones of the right forearm was performed with 3.5 mm metaphyseal plates, and the distal radioulnar joint was fixed with a screw.
Appearance of the limb after surgery, angular deformity eliminated. The limb segment is stable, movements in the elbow and wrist joints are not limited, rotation of the forearm is limited due to the presence of a positioning screw, which will be removed after 6 weeks.
X-rays after surgery.
This osteosynthesis is very stable and allows you to begin rehabilitation within a day after surgery. Forced loads on the forearm are naturally limited until x-ray confirmation of consolidation. It is advisable to perform X-ray control after 6 and 12 weeks. If signs of fusion are well expressed, full weight bearing is possible 12 weeks after surgery.
Forearm fracture - symptoms, treatment and rehabilitation
A forearm fracture is one of the most common types of damage to the integrity of bone tissue. Statistics show that it accounts for about 30% of all closed fractures and 53% of all injuries to the upper extremities. This type of injury can occur in anyone: a child, an adult, or an elderly person.
The complexity of the fracture is largely determined by the nature and location of the lesion. Such a fracture requires a long recovery period and often causes negative consequences.
Classification
When diagnosing a forearm fracture, doctors use a fairly broad classification. It allows you to accurately determine all the features of the damage. At the moment, experts adhere to the following system.
| Type of fracture | Peculiarities |
| Radius in typical location | The most common injury most often encountered by older women. Usually appears after a fall with a straight arm on the palm. Causes severe pain, recovery takes 3-4 weeks. |
| Diaphysis of both bones | The most common injury occurs from a fall on the hand or a blow to the forearm. Accompanied by displacement of fragments, the limb is shortened, and severe pain occurs. |
| The middle part of the ulna | Occurs after being hit by an elbow or falling on it. You can recognize it by the sharp pain with any attempt to move. The average duration of immobilization is 4-5 weeks. |
| Radius in the middle part | Occurs after a blow to the forearm. Swelling and visible deformation occur, the fragments remain mobile. For treatment, it is necessary to apply plaster tape for 4-5 weeks. |
| Necks or heads of the radius | A dangerous fracture that requires a long recovery period. Usually occurs after unsuccessful training or a fall on the shoulder. The plaster is applied for 3-4 weeks. |
| Monteggia | Combined damage: includes a fracture of the elbow, dislocation of the radius and damage to the branch of the ulnar nerve. Usually occurs when parrying a blow with a bent or raised forearm. The recovery time after such a fracture is 6-8 weeks. |
| Galeazzi | Combined injury, including a fracture of the radius, dislocation of the head of the ulna. Occurs when falling or hitting a straight arm. Recovery time is at least 8-10 weeks and surgery may be required. |
| Olecranon process | Occurs after a blow to the forearm. Causes swelling, sharp pain, and limited movement. |
| coronoid process | Occurs after a fall on a bent elbow. Causes swelling and hematoma near the cubital fossa. There is movement, but it is limited. |
Causes of damage
A forearm fracture is a fairly common problem that requires immediate attention from a qualified physician.
Many people, due to the nature of their work, have a high probability of such injury.
Among the reasons that can lead to a forearm fracture are:
- Falling with your whole body on your hand;
- Effect of compressive force;
- Road traffic accidents;
- Consequences of certain diseases;
- A strong blow to the shoulder;
- Unnatural rotation;
- Accident;
- Gunshot wound.
In children, a fracture of the forearm most often occurs due to domestic injuries or falls from a height.
In rare cases, they occur as a result of violent acts or beatings. If the fracture is accompanied by displacement of fragments, then the cause is a strong blow. When the diaphyseal area is damaged, the cause of the fracture is muscle tension.
Possible complications after osteosynthesis of the middle third of the forearm.
Infection. There are certain risks of infectious complications with any surgical intervention, forearm osteosynthesis is no exception.
Damage to nerves and blood vessels. There is a small risk of damage to the nerves and blood vessels at the level of the forearm during surgery. If after surgery there is weakness and numbness in the hand area, or persistent limitation of movements appears, this is a reason to consult a doctor, since such neuropathy may not resolve without emergency intervention.
Synostosis. In some cases, after a fracture of both bones of the forearm, a bone bridge may arise between them, which will limit the rotational movements of the forearm.
Nonunion. The operation does not guarantee healing of the fracture. Sometimes the bone does not heal, and in such cases a repeat, more complex operation is required.
Smoking and drinking alcohol slow down the healing process and may lead to delayed fracture consolidation.
Fractures of the head and neck of the radius
This type of fracture makes up about 2% of the total number of fractures and occurs due to indirect trauma - a fall on a straight arm with a radial deviation of the forearm, when the head hits the head of the condyle of the humerus. Depending on the force and angle of the impact, there are different types of fracture: chipping off the edge or half of the head, crushing the head, fracture of the neck, and in children - epiphysiolysis or osteoepiphysiolysis.
The head or its fragment is displaced at an angle outward and downward by the force of the impact; The degree of tilt of the head may vary.
Symptoms and diagnosis . The patient supports the arm in a forced half-extended position. The elbow joint is swollen with significant valgus deformity of the forearm. Palpation - sharp pain from the olecranon. Active and passive flexion-extension movements in the elbow are limited, and supination and pronation through pain are impossible. The nature of the fracture and the degree of displacement of the fragments are clarified radiographically.
Treatment . For fractures of the head and neck of the radius without displacement of the fragments, a posterior plaster splint is applied from the shoulder joint to the heads of the metacarpal bones in a mid-physiological position with the forearm bent. The period of immobilization in children is 10-14 days, in adults - 3 weeks.
When choosing treatment tactics, the degree of displacement of fragments is assessed. In adults with a fracture of the neck of the radius, a head tilt of up to 15° is considered an acceptable displacement, since it does not affect the function of the limb. In children, displacement of fragments left uncorrected threatens to increase deformity as the bones grow. Therefore, ideal reduction of the radial head is necessary.
If the head is significantly displaced, an attempt is made to straighten it conservatively. Under local anesthesia in adults and anesthesia in children, the arm at the elbow is straightened with full supination and maximum adduction of the forearm. This creates space for the head, which is pressed into its bed with your fingers.
The most effective way to realign the head of the radial bone, which is displaced at an angle, is to perform repeated rotational movements of the straightened forearm (supination-pronation) under anesthesia. With the forearm flexed to 160°, a posterior plaster splint is applied and X-ray control is performed. After 10 days, the forearm is bent to 90°. Subsequent treatment is carried out in the same way as for fractures without displacement of the fragments.
If closed reduction is unsuccessful, surgical treatment is indicated. Under anesthesia, the joint is opened using a posterolateral approach and the head of the radial bone is exposed. All manipulations are carried out so as not to injure even the hooks of the deep branch of the radial nerve, which lies in front, directly at the joint capsule. The dislocated head is removed with a spatula and visually reduced. With the forearm bent to 80° and supinated, the head is fixed with a Kirschner wire passed through the skin from the back of the elbow through the head of the condyle of the humerus, the joint space and the head, immersing the wire (5-7 cm) into the proximal end of the radius. The wound is sutured and a posterior plaster splint is applied for the same period as in previous cases.
Surgeons who do not fix the heads with pins flex the forearm at a more acute angle to press the head of the radius into the head of the humeral condyle and prevent the possibility of re-displacement. In case of comminuted fractures of the head of the radius, when there is practically no possibility of reducing them, or there is a threat of deforming arthrosis, contractures, the head is thrown out and the fracture area is leveled, so that exostoses and ossifications do not occur.
After removal of the head, forearm movements in all planes are quite satisfactory, although the overall strength of the limb is somewhat reduced. Removal of the head of the radial bone in children is unacceptable, since this risks significant deformities (clubhandedness) due to removal or damage to the epiphyseal cartilage.
With fractures of the head and neck of the radius, contracture quickly develops in the elbow, and rotational movements of the forearm are especially limited.
After removing the plaster cast, complex restorative treatment is carried out, which requires endurance and patience of both the patient and the doctor.
Rehabilitation after osteosynthesis surgery of the middle third of the forearm.
After osteosynthesis surgery, it will take a short period of time for swelling and pain to subside before you begin active rehabilitation. In the early postoperative period, it is possible to use a scarf bandage to reduce pain and for disciplinary purposes. Topical use of ice or cryotherapy gel bags, which are sold at any pharmacy, can effectively combat pain and swelling. Their use is also possible at a later date from the operation.
For the first 2-3 weeks, physical therapy is limited to performing movements in adjacent joints - the elbow and wrist; starting from the 3rd week, a gradual onset of rotational movements is possible. Full amplitude is restored by 6 weeks after the intervention. Physical activity is not allowed before there is a clear x-ray picture of fusion, which usually occurs by 3 months. The decision to remove metal fixators is made no earlier than 2 years from the date of surgery.
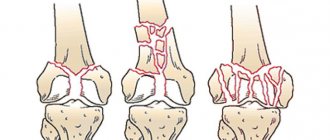
Olecranon fractures
Fractures of the olecranon process are intra-articular and account for 1-1.5% of all skeletal fractures. They most often occur as a result of direct trauma (impact from a fall); avulsion fractures and epiphysiolysis from a sharp contraction of the triceps brachii muscle, which is attached to the process, are less common.
The fracture plane is transverse or oblique. In case of direct injury, it is located, of course, in the middle of the semilunar notch or at the base of the process, and in case of indirect injury, it is closer to its apex. The degree to which the fragments differ from each other depends on the force of the impact and the contraction of the triceps muscle. If during an injury the fibrous fibers of the tendon are not too damaged, which cover the process along the entire length and maintain their integrity, then a fracture without displacement occurs. In most cases, as a result of direct trauma, the fibrous fibers are torn, and the fragments diverge from each other by 1-2 cm.
Symptoms and diagnosis . Upon examination, the arm is half extended, and the patient supports it with his healthy arm. The elbow joint is swollen as a result of hemarthrosis, with a bruise from hemorrhage in the tissue, its contours are smoothed. In case of a fracture without displacement of the fragments, only local pain is determined by palpation; in case of displacement, the fracture gap is determined, as well as the degree of difference between the fragments. Passive movements sharply increase pain, and active extension is limited and painful, since it is carried out under the weight of the forearm and hand.
To check the degree of possible active extension of the forearm, you need to abduct the shoulder to 90 ° and rotate it inward, then the forearm will hang at an angle of 90 ° at the elbow.
X-rays determine the nature of the fracture, the presence of small fragments and the degree of difference between the fragments.
In children, the diagnosis of a fracture is based mainly on clinical symptoms, since the ossification nucleus of the olecranon appears only at 10-12 years of age, and its fusion - at 18-20 years. Therefore, for fractures in adolescents, comparative radiography with a healthy arm is used.
Treatment . If there are fractures of the olecranon process without displacement of the fragments, apply a posterior plaster splint from the shoulder joint to the heads of the metacarpal bones in the forearm bent to 100° and in its average position between supination and pronation. The fixation period is 2-3 weeks, then restorative therapy. The period of incapacity for work is 6-8 weeks.
It is believed that conservative treatment is advisable to use when the fragments diverge, but not more than 0.3-0.5 cm, that is, in the absence of a rupture on a par with a fracture of the aponeurosis of the triceps brachii muscle containing fragments among themselves. In such cases, when the forearm is extended, the fragments come closer to each other, and the triceps muscle relaxes, thereby creating conditions for their fusion.
Under local anesthesia with 10 ml of 1% novocaine solution, the forearms are extended to an angle of 140-150 ° and at the same time the tip of the process is pressed to its bed. A posterior plaster splint is applied for 3-4 weeks.
With conservative treatment of patients with olecranon fractures and the forearm extended at the elbow, extension contracture develops very quickly, which is more difficult to eliminate than flexion contracture.
To prevent extension contracture, after 10 days it is recommended to bend the forearms slightly (up to 110-120°), replacing the plaster splint, but always with subsequent x-ray control. Since with such a withdrawal the forearm fragments often diverge again, it was abandoned and a closed percutaneous compression method of repositioning and fixing the olecranon process was used according to the method of A. Edinak or A.P. Oleksa.
Fixation technique using the method of A. P. Oleksa
Under local anesthesia with a 1% novocaine solution, a Kirschner wire is passed through the upper third of the ulna diaphysis perpendicular to its axis. Then, using a screw-shaped nail with a supporting plane, the broken olecranon process is pricked from the top along its axis. Deflecting the suture axis and straightening the forearm, the fragments are reduced and the nail is tightened so that part of it enters the ulna bone and rests the supporting plane against the tip of the process. Then an arch is placed, the ends of which are attached to a Kirschner wire passed through the ulna, and the center of the arch is attached to a nail. A special screw is used to tighten the device.
With this method of fixation, a plaster splint is used and after 2-3 days it is recommended to perform movements in the elbow.
In case of unsuccessful closed reposition of fragments and diastasis between them, open reduction and fixation of fragments is used. Under anesthesia or local anesthesia, a transverse or longitudinal semicircular incision is made - from the apex of the process downward, moving laterally 1 cm from the crest of the ulna. In children, the fragments are fixed with a circular suture, in adults - with a screw, rod or tie wire through the bone. After osteosynthesis, the fibrous aponeurosis is sutured over the fracture and the wound is sutured.
In case of comminuted fractures, when composing the fragments, it is important to restore the congruence of the articular surface of the process in order to ensure the function of the joint. Loose small debris along the ulnar surface can be removed.
After the operation, the patient is treated in the same way as for fractures of the olecranon without displacement of the fragments. Performance is restored after 6-8 weeks.
Fractures of the coronoid process are extremely rare (0.2-0.3%), accompany posterior dislocation of the forearm and arise as a result of direct trauma. The diagnosis of a fracture of the coronoid process is established according to an x-ray taken in a lateral projection, since the clinical symptoms overlap with the symptoms of hemarthrosis, dislocation, etc.
If there is a fracture of the coronoid process, then in order to press it and adapt it to the fracture site, the forearm is bent with full supination to an angle of 60-70 ° and in this position is fixed with a posterior plaster splint for a period of 2-3 weeks.
After removing the splint, movements in the elbow joint are developed. The period of incapacity for work is 4-5 weeks. In cases where the fragment is displaced or the ossification formed in it limits the range of movements in the joint, the obstacle is removed promptly.
About the forearm
The forearm (Latin - ossa Antebrachii) is a segment of the free upper limb, consisting of two paired bones - the radius and ulna.
The forearm is an extension of the shoulder, and is connected to it through the elbow joint. The continuation of the forearm is the hand, which is connected to the forearm using the carpal joint. The forearm plays an important role in the function of the upper limb and has a complex structure. The bones of the forearm form 6 joints, thanks to which a person can perform complex hand movements in his life.
The bones of the forearm serve as the attachment point for many muscles of the flexors and extensors of the fingers and hand, etc. The complex structure and function of the forearm is of great importance in the treatment of damage to the bones that form this segment.
Treatment methods
A fracture of the forearm bones requires mandatory first aid measures. First of all, it is necessary to immobilize the limb by applying a splint or other similar object that is at hand. If the person is in severe pain, pain medication should be given and then quickly taken to the emergency room.
In case of damage without displacement, a plaster splint is applied and the arm is fixed in a bent position. You will need to wear it for about two weeks. Then, until the limb is completely restored, a removable splint is applied, and only after the doctor’s permission is it removed completely.
Complex displacement injuries or cases where both bones are broken are treated with surgery. It is quite difficult to cure such damage using a conservative method. The displacement can be corrected, but surgical intervention is required to restore rotation function.
Performing osteosynthesis surgery
The operation takes place in 5 stages, which allow you to install, secure the plate and process the incision. Below is a description of the intervention.
Cutting skin
The incision is made relative to the course of the median nerve, located next to the palmaris longus muscle, which serves as a guide for its execution. The location of the nerve is between the passage of the palmaris longus muscle and the flexor carpi radialis muscle. When making a cut, it is necessary to deviate towards the flexor radialis from the tendon being palpated and continue in deeper layers, avoiding damage to the superficial branch of the radial nerve.
Providing access
After exposing the intermuscular space, it is necessary to develop the layer between the location of the flexor radialis tendon and the tendon of the palmaris longus muscle. The layer is designed taking into account the length required for high-quality treatment of the fracture. It is possible to increase the development before placing the flexor tendon stretch to completely expose the radial styloid.
Intersection of the pronator quadratus.
The pronator quadratus is transected along the radius. Using blunt hooks, the surgeon picks up and moves aside the median nerve and flexor fingers. The radial artery and flexor carpi muscle are drawn in the other direction.
Identification of the fracture site.
Full abduction of the pronator quadratus muscle exposes the fracture site. To facilitate work and gain full access to the injury site, the flexor tendon sprain should be separated as distally as possible.
Contouring the T-plate.
At the site of the exposed fracture, a plate for osteosynthesis of the forearm in the shape of the letter “T” is installed. It is applied and installed so that it fixes all separated elements. Once secured to the styloid process, the placement of the plate can be adjusted. An oval hole is used for this. Final fixation is performed with the remaining screws.
Rehabilitation period
After proper treatment of a patient with a fracture of the forearm bones, restoration of motor activity of the limb and the whole body will depend on the nature and severity of the injury. To quickly restore working capacity, it is necessary to carry out the following procedures:
Read also: What to do if you sprain your shoulder joint
- therapeutic gymnastics, which helps to develop the limb, restore normal mobility,
- massage of the limbs with kneading of the hands to improve blood circulation,
- physiotherapeutic procedures (baths, electrophoresis, exposure to an electromagnetic field).
If you follow the recommendations of a rehabilitation doctor and perform the appropriate procedures, rehabilitation after a fracture proceeds quickly and without complications.