A dislocation is an injury in which a limb is misaligned, making even the smallest movements impossible, and attempts are accompanied by severe pain. A dislocated arm is also often characterized by rupture of the ligaments or joint capsule. The affected area swells, hemorrhages appear, and the joint shape changes. Finger injuries, dislocation of the hand, elbow or collarbone are the most common.
If such situations arise, you should immediately go to the hospital, since it is not recommended to straighten the hand yourself due to the risk of complications. How to diagnose a dislocation, what to do in case of a dislocated arm and how will the treatment be carried out?
Classification
When classifying arm dislocations, it is customary to focus on the following factors.
- According to origin: pathological, congenital, habitual traumatic and acute;
- According to the volume, it is customary to distinguish between partial and complete dislocations;
- Considering the location, the injured area can be a finger, forearm, elbow joint or shoulder. Often in the practice of traumatologists, dislocation of the hand is also encountered;
- The type of injury determines closed and open dislocations;
- According to the duration, they can be old, stale and fresh. With chronic arm dislocations, they are more than a month old. For stale ones - over 3 weeks, for fresh ones - no more than 3 days.
Classification of dislocations
Upper limb dislocations are classified as follows:
- By origin: Arm dislocations occur:
- acute traumatic;
- habitual traumatic;
- congenital;
- pathological.
- By volume: Dislocations of the upper extremities are:
- full;
- partial.
- By location: Arm dislocations can be:
- shoulder dislocation;
- dislocation of the elbow joint;
- forearm dislocation;
- dislocation of the hand;
- dislocated finger.
- By type of injury: Dislocations of the upper extremities are:
- open;
- closed.
- By duration: Arm dislocations occur:
- fresh (no more than 3 days have passed since the injury);
- stale (3 to 4 weeks have passed since the injury to the upper limb);
- old (more than 30 days have passed since the dislocation occurred).
Causes and predisposing factors
Among the key reasons are the following factors:
- Non-professional massage;
- Lifting weights;
- Fall or strong blow.
The progression of existing pathologies also increases the likelihood of injury:
- Arthritis and arthropathy;
- Bone tuberculosis;
- Arthrosis.
A separate category includes people with a congenital predisposition. Their key feature is that the depth of the pits in the joint is insufficient, and the ligaments themselves are weak. That is why the heads of the bones that enter them are very easily injured due to loose fixation.
Causes of arm dislocation in children
The main risk group is active children, who often experience falls and injuries. An additional seasonal factor that increases the risk of injury is winter ice, when a fall can happen even to a calmly walking child or adult. Experts consider regular participation in certain sports, heavy lifting and strong impacts as risk factors.
Trauma is not the only cause of a dislocated arm in a child, but congenital causes and pathological destructive processes are still much less common.
Symptoms
General signs of a dislocated arm with a closed injury are as follows:
- Severe pain is the main symptom of a dislocated wrist or any other part of the upper limb;
- The mobility of the joint decreases sharply, flexion and extension are accompanied by severe pain. It is impossible to fully straighten the limb; it can also spring. The latter sign is most often considered as a symptom of a dislocation of the hand or a fracture of the radius in a typical location;
- Swelling and swelling appear some time after the injury. The affected arm may appear visually shorter. Palpation of the damaged joint allows you to feel the protrusion of the head of the bone from the joint sac.
These symptoms of a dislocated arm are considered general and may differ depending on the location of the injury.
Causes and symptoms of a dislocated arm
The main causes of a dislocated arm include the following:
- a fall;
- lifting weights;
- swipe;
- massage performed by an amateur, etc.
Sometimes (pathological) dislocations can occur due to the progression of various diseases:
- arthrosis;
- bone tuberculosis;
- arthropathy (of various origins);
- arthritis and other diseases in which changes in the joint capsule occur.
When an arm is dislocated, regardless of the location of the injury, a person experiences severe pain. He may completely or partially lose the mobility of his arm. Almost immediately after receiving an injury, swelling forms in the area of the injured joint. Some patients lose sensation in the lower part of the limb (this is due to the fact that the median nerve was compressed during the dislocation). When palpating the pulse, victims may experience both a rapid and slow rhythm. Another indicator of a dislocated hand is the “springy fixation symptom.” Confirming the presence of this symptom is quite simple by making a passive movement of the lower arm.
Most often, dislocation occurs in the shoulder joint of the upper extremities. When this joint is injured, the risk of damage to nerves and arteries increases, so patients with such a dislocation must be rushed to the hospital.
This category of patients may exhibit the following symptoms:
- severe pain;
- bruising;
- swelling;
- impaired motor function in the damaged upper limb, etc.
First aid
First of all, it is necessary to determine what type of injury the dislocation is; the treatment of a dislocation of the hand and the speed of further recovery depend on this stage. The sequence of actions is as follows:
- Determination of the severity of pain symptoms;
- Comparison of joints on both hands to visually determine displacement;
- Assessment of localization of edema. In case of a fracture, it is located in the area of the bone, and in case of dislocation - in the area of the joint;
- Assessment of the ability to move fingers and the presence of sensitivity in the fingers and the hand itself;
- Using a splint and fabric to fix the damaged area relative to the body;
- Apply a cold compress and urgently visit a traumatologist.
Diagnosis of a dislocated arm
After the patient is taken to the hospital, the traumatologist will conduct an examination, palpation and questioning.
- Palpation allows not only to determine the sensitivity of the damaged area, but also to assess motor function, assess the rhythm of arterial pulsation and detect pathologies of the neurovascular bundle. Palpation also allows you to determine the nature of the change in the shape of the joint and detect retraction in the area where the articular endings are localized;
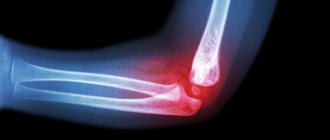
- At the next stage, the patient will undergo an x-ray, which allows identifying associated damage in the form of cracks or fractures. Traditionally, a 2D or 3D x-ray is taken and the results are provided to the patient upon request;
- Referral to the surgical department will be relevant if serious deformities of the limbs are detected that need to be corrected through emergency surgery. If a dislocation of the same joint is diagnosed more than 3 times, surgical intervention will be mandatory, after which the patient will receive a disability group.
Prevention of arm dislocation in children
Parents need to have a preventive conversation with their child and try to explain to the child that excessive activity can lead to injury and painful consequences.
For children who engage in contact sports, care should be taken to purchase appropriate protective equipment (elbow pads, knee pads). It is also recommended to choose sports that promote the development and strengthening of the musculoskeletal system.
An important preventive method is a proper balanced diet, including foods that provide the growing body with nutrients, vitamins and microelements necessary for the normal development of the musculoskeletal system.
Features of treatment
Pain relief is the first stage of treatment for a dislocated arm, since acute pain is the first thing that will bother the patient. It is advisable to do general anesthesia for severe damage. Since damaged segments must be reduced after anesthesia, the analgesic must be potent.
Reduction can begin only after complete muscle relaxation.
After reduction, a plaster cast must be used. It will not be possible to remove it for 3-4 weeks.
Treatment of a dislocated arm
Since a dislocation, like any other injury, is accompanied by severe pain, treatment of the patient begins with pain relief (for severe injuries, general anesthesia is given). In most cases, this category of patients is prescribed strong painkillers, since after the pain is relieved, the dislocated segments of the upper limbs are realigned. After complete relaxation of the muscles, the traumatologist begins the reduction procedure, which is carried out very carefully, without sudden or rough movements. The reduced limb is fixed in the correct position using a plaster cast, which must be worn for a certain time (for several weeks).
Once the plaster cast has been removed, the patient needs to undergo a rehabilitation course that will help restore mobility and functionality of the arm.
For these purposes the following may be prescribed:
- physiotherapeutic procedures;
- physiotherapy;
- hydrotherapy;
- magnetic therapy;
- massage;
- mud therapy;
- mechanotherapy, etc.
Each of the rehabilitation methods is aimed at normalizing blood circulation in the injured limb, relieving pain, etc. Thanks to a properly selected complex of physical therapy, patients are able to quickly increase the elasticity of muscle tissue.
Some patients, self-medicating, lose valuable time for dislocation of the joints of the upper extremities without surgical reduction. They often present to a medical facility several weeks after their injury.
In such a situation, specialists are forced to carry out treatment in several stages:
- First of all, the patient is given a distraction device, the functions of which are to stretch the wrist joint.
- After the wrist joint has been stretched, surgeons perform open reduction of the dislocation and remove the distraction device. This procedure may take 8-10 days, depending on the complexity of the dislocation.
- The damaged wrist joint is fixed using Kirschner wires.
- After surgery, this category of patients will need to undergo physiotherapeutic treatment.
When performing surgical treatment of an old dislocation in which deforming arthrosis has developed, specialists perform arthrodesis of the wrist joint. Patients who have undergone such an operation require a long course of rehabilitation therapy.
Fresh hand dislocations
For fresh wrist dislocation, anesthesia is used. The reduction is carried out by a surgeon and an assistant, since only two people can correct the hand. An assistant is needed to keep the shoulder immobilized, while the surgeon stretches the wrist joint by stretching along the axis of the forearm. One hand of the specialist should pull one finger of the hand, and the other hand should pull the others.
To correct a dorsal dislocation, the surgeon must apply pressure to the bulging area at the wrist joint using his or her thumbs. Next, fixation at an angle of 40 degrees relative to the neutral position of 90 degrees is relevant. The area from the elbow to the metacarpophalangeal joint is fixed. At the final stage, a control x-ray is performed.
After a couple of weeks, the hand must be removed from the specified position and fixed again with a plaster splint for 2 weeks.
Dislocations of the hand
True hand dislocations
Rarely observed. With true dislocations of the hand, the articular surfaces of the upper row of carpal bones, together with the hand, are completely displaced in relation to the articular surface of the radius. More common is complete dorsal dislocation of the hand, less common is complete palmar dislocation. Complete dislocations of the hand can be combined with a fracture of the radius and styloid processes.
Perilunate dislocations of the hand
They make up about 90% of the total number of hand dislocations. Occurs when falling with emphasis on the hand or sudden forced extension of the hand. With a perilunar dislocation of the hand, the contact between the lunate and radius bones is maintained, and the remaining bones of the wrist are displaced to the rear and to the center. Perilunar dislocation of the hand is sometimes accompanied by fractures of the triquetrum, scaphoid bones and styloid processes.
Perilano-lunar dislocations of the hand
The lunate and scaphoid bones remain in place. The remaining bones of the wrist move toward the back and center.
Peritriquetral-lunar dislocations of the hand
It is extremely rare. The triquetrum and scaphoid bones remain in place. The remaining bones of the wrist move toward the back and center.
Transscaphoid-perilunar dislocations of the hand
Must be combined with a fracture of the scaphoid. With this dislocation, the lunate bone and the central fragment of the scaphoid maintain their position. The remaining bones of the wrist, together with the distal (located further from the center) fragment of the scaphoid bone, are displaced towards the rear.
Transscaphoid-translunate dislocations of the hand
Accompanied by a fracture of the lunate and scaphoid bones. The proximal (central) bone fragments remain in place, while the distal ones, together with the rest of the bones of the wrist, are shifted to the rear and to the center.
Metacarpal dislocations
The metacarpals are short, tubular bones that connect the wrist to the bones of the fingers. The metacarpal bones are held tightly by ligaments, so they dislocate very rarely. Dislocations of the metacarpal bones are almost always combined with their fractures. Reduction of the metacarpal bones is performed under local anesthesia. If conservative reduction is impossible, surgical techniques are used, and if there is instability, fixation with Kirschner wires is used.
Dislocations of fingers
Dislocations in the interphalangeal joints and dislocations in the joint between the metacarpal bone and the bone of the main phalanx of the finger are possible. The most common dislocation of the first finger occurs. The cause of injury is excessive extension, and less commonly, excessive flexion of the finger. A dislocated finger is accompanied by deformation, swelling and severe pain. Movement in the injured joint is impossible. The dislocation is reduced by traction on the finger. The impossibility of reduction is usually due to soft tissue entrapment. In this case, surgical reduction is performed.
Joint instability
The use of Kirschner wires is important when dislocation occurs again immediately after reduction. After inserting the needles, the wound is sutured in layers, and the joint is fixed for a month or a month and a half. If we are talking about transscaphoid-perilunar dislocation, the period increases to 4 months. It is permissible to use distraction devices in the following situations:
- Late visit to a traumatologist;
- No compressive symptoms;
- Closed reduction is not possible.
If the median nerve is compressed in the carpal tunnel, the dislocation must be reduced through surgery or the risk of nerve degeneration increases.
Old dislocations
Treating a dislocated hand at home and ignoring the need to visit a traumatologist often leads to complications that cannot be corrected without surgery. When asking for help late, be prepared for the following procedures.
- Application of a distraction device to stretch the joint;
- Open reduction of the dislocation followed by removal of the device. The duration of such a procedure can be up to 10 days;
- Using Kirschner wires to fix the joint;
- Rehabilitation physiotherapy.
Treatment of a dislocated arm in children
If a child has severe pain, then in the absence of contraindications, anesthesia is performed. Local anesthesia is also required to perform joint reduction. Anesthesia helps the muscles relax, which makes the doctor's job easier. The reduction process itself proceeds slowly and smoothly, without jerks or sudden movements. Only a specialist can perform joint realignment. Parents' attempts to straighten the arm themselves can cause additional harm.
Depending on the severity of the lesion, a plaster splint may be placed on the arm, which the child will have to wear for one to several weeks. The splint keeps the arm in the correct position and reduces pain. After removing the splint, restorative therapy is prescribed, which includes a set of measures - massage, gymnastics, physiotherapeutic procedures. Rehabilitation procedures are aimed at restoring mobility to the arm, restoring blood circulation and strengthening joint tissue.
If the treatment was not timely and attempts were made to self-medicate, then serious risks to the child’s health arise. Old dislocations are often treated surgically.
One of the methods of treating long-standing severe cases involves the installation of Kirschner wires. The entire procedure includes the following steps:
- to stretch the wrist joint, a distraction device is applied;
- open reduction of joints is performed using the surgical method;
- removal of the distraction device;
- joint fixation using Kirschner wires;
- long-term restorative physiotherapy.
Complications that threaten untimely or incomplete treatment of a dislocated arm in a child:
- the risk of re-injury increases;
- unreduced dislocation can cause rupture of tendons, ligaments, muscle tissue, and blood vessels;
- Pathologies and joint damage may develop in adulthood.
In order for the treatment to be effective, so that the dislocation does not make itself felt in the future, it is very important that the patient follows all the doctor’s instructions. Otherwise, therapy may be delayed and may not give the desired result.
Rehabilitation
A rehabilitation course is a mandatory measure to restore the functionality of the arm after removing the cast. The recovery stage consists of the following techniques:
- Therapeutic exercises and a set of physiotherapeutic procedures recommended by a specialist;
- Magnetic therapy, mud treatment and hydrotherapy;
- Massage;
- Mechanotherapy – physiotherapeutic procedures using exercise machines.
Child's arm dislocation
In children, dislocation of the wrist or other part of the hand occurs much less frequently than in adults, since at a young age the elasticity of the joints and cartilage tissue is higher. There is also an increased volume of soft tissue in the form of subcutaneous tissue and muscles, since nature has provided for the restlessness and curiosity of children's nature.
The only exception is a common injury called “nanny's elbow.” We are talking about a dislocation of the radius due to a sharp pull on the arm in an extended position, for example, when a child falls and an adult sharply pulls his arm, trying to prevent a bruise.
At the time of injury, you can hear a characteristic crunch; after a while, the affected area swells slightly, the child does not move his arm and behaves restlessly. An orthopedist-traumatologist can correct the situation. On the way to the doctor, be sure to immobilize your injured arm.
It is enough to simply set the head of the radial bone; there is no need to even apply a bandage for fixation (except for repeated dislocations). After an injury, you cannot lead a child by the injured arm. By age 5, the radius bone will be stronger and the risk of such injury will be minimized.
To summarize, it is worth emphasizing once again the need to consult a doctor immediately after an injury to reduce the dislocation. Otherwise, you risk aggravating the situation, which cannot be corrected without surgery. In advanced cases, it will be difficult not only to reduce it, but also to further restore the functions of the upper limb.
Symptoms of a dislocated arm in children
How to detect a dislocated arm in a child? It is not always possible for adults without special medical education to immediately accurately determine the type of injury in a child - a dislocation, a severe bruise, or even a fracture. Symptoms of a dislocated arm in a child are similar to the signs of a fracture and at the same time can also resemble a reaction to a severe bruise, so timely contact with a specialist becomes especially important.
The main signs of a dislocated arm in a child:
- unnatural hand position and low mobility or complete immobility;
- presence of hematoma and slight swelling;
- severe pain that sharply intensifies when you try to move your arm, hand, or fingers;
- rapid or, conversely, slow pulse.
A hematoma usually does not form immediately; it appears later, sometimes after several hours. The formation of severe swelling and severe hematoma is most often observed if there is additional spraining of the ligaments, rupture of articular tissues and capsules.