Orthopedic traumatologist > Articles > Review of characteristics of shoulder dislocation and treatment methods
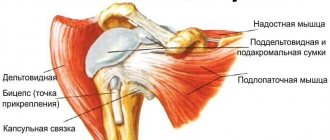
The slightest wrong movement, road accident, or other situations provoke the appearance of problems with the musculoskeletal system. Moreover, a dislocation of the shoulder joint can become an unpleasant companion not only for older people. According to doctors, the shoulder joint is one of the most mobile and at the same time a vulnerable part of the body. How to recognize this problem is a question that is clear to many.
Dislocation
Dislocation During injury, damage to the ligamentous apparatus occurs.
It is because of this that swelling and swelling occur in the area of the damaged area, and stiffness of movement is noted. A dislocation always causes a leg deformity. This is a clear sign by which you can identify an injury even before visiting a specialist. The knee is made up of two separate joints, each of which can be everted. The patella experiences peak loads during the transfer of muscle mass during movement and during flexion and extension of the limb. Correct functioning of the patella is ensured by centering. When this function is lost, a dislocation of the cup, or, more correctly, the patella, occurs.
Secrets of diagnostic procedures for shoulder dislocation
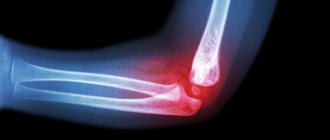
At the first examination, the doctor prescribes an x-ray. The method is performed in two projections. In this case, radiologists use anterior and axial projections. The first method helps to see the dislocation of the shoulder joint in downward and inward displacements. When examining using the second technique, the doctor sees anterior and posterior displacements. A more complex case is when there is a dislocation with a fracture of the head or neck of the bone. In some situations, they resort to RCT. Moreover, sometimes diagnostics show an old problem with the shoulder joint. These include a dislocation 3-4 weeks ago. Correction is considered quite difficult due to tissue degeneration. Once the problem is confirmed, treatment is prescribed.
An old recipe for successful treatment of shoulder dislocations
Thanks to the Soviet surgeon Justin Jalanidze, many patients go home 20 minutes after visiting the doctor. What is the essence of healing? There is no magic, but professionalism and accuracy are required from the doctor.
- The patient is placed on his side on the couch. At the same time, an anesthetic injection is given.
- The hand hangs towards the floor; the person will be required to completely relax the muscles. After 20 minutes the patient can go home.
Sometimes the joint moves back into place on its own. A characteristic click when the bone head approaches the glenoid cavity helps to understand that a dislocation of the shoulder joint has occurred. The doctor selects the most appropriate technique based on the individual characteristics of the limb. It is important to provide the patient with 3 weeks of rest after treatment! What other methods do doctors use in practice?
About progressive healing methods
More progressive medicine does not stand still, offering multifaceted treatment options.
Features of arthroscopic surgery
A full hospital stay is not required. After surgery, the patient is usually sent home. The intervention is carried out using a special instrument - an arthroscope. The doctor makes small incisions on the shoulder and inserts an instrument. The procedure is performed under general anesthesia or local anesthesia.
After surgery, the patient must take antibacterial medications, painkillers, and non-steroidal drugs. The most important stage is exercise therapy, but more on that later.
Plastic surgery of muscle tissue for habitual shoulder dislocation
Doctors call the intervention “Operation Latarget.” In 96% of cases this is exactly what they do. To do this, the lost bone lobe is fixed with bolts. How to properly prepare for surgery?
Formula for proper preparation
In order for a dislocation of the shoulder joint to no longer remind you of itself, it is important to prepare well.
- The patient will be required to undergo tests.
- Next you need to perform an X-ray examination and an ECG.
- You should not eat food 12 hours before surgery.
- You should not drink alcohol 2 weeks before surgery.
After surgery, the person will have to undergo a rehabilitation course.
Basics of rehabilitation recommendations
Correct rehabilitation will help him quickly forget that a person has suffered a dislocation of the shoulder joint. It happens in several stages.
At first, nurses apply an immobilizing bandage to the patient. In the old days, plaster was used, but today a sling is an excellent alternative. In addition, the types of immobilization include a bandage option, when the arm is slightly removed from the body. The method is considered the most convenient in terms of minimizing the risk of recurrent dislocation by 40%.
Immobilization usually lasts up to 4 weeks, but depends on the immune system, characteristics of the body, and the type of work the person does. For example, rehabilitation of athletes lasts about six months!
In this case, the patient takes anti-inflammatory drugs. Moreover, exercise therapy exercises are effective as prevention.
Reasons for the development of the disease
There can be several reasons for a dislocation. Most often, the injury is provoked by a sharp mechanical force in the area of the patella (impact). Less commonly, pathology is caused by a sharp contraction of a muscle, for example, during a fall from a height, an accident, or during sports training. In addition, specialists from Dr. Glazkov’s clinics emphasize that there are other factors whose presence predisposes to the development of the disease. This is a congenital or acquired anomaly that provokes a violation of the structure of the musculoskeletal system. If we are talking about a congenital defect, it should be noted that the defect manifests itself differently in boys and girls, therefore the therapeutic methods prescribed by specialists are also different.
Causes of joint dislocations
Dislocations are divided into:
- traumatic;
- pathological (habitual).
A traumatic dislocation occurs if a force is applied to a joint that significantly exceeds the endurance threshold of its structures, and the vector of this force is directed at an angle (usually 90 ̊) relative to the axis of the joint. The supporting structures cannot withstand such a load and shift relative to the applied force that occurs when there is a strong blow to the joint area, a jerky movement of the limb, or a fall on an outstretched limb.
Pathological dislocation occurs in a joint with congenital structural pathologies. Displacement of bone heads occurs even with a slight impact on an immature or incompletely formed joint.
The causes of such conditions:
- pathological changes in articular structures of an inflammatory or degenerative nature;
- age-related physiological changes in the joint;
- previous injuries: intra-articular fracture, dislocation;
- insufficient bone density associated with low calcium levels in the body;
- pathology of the nervous system, leading to paresis or paralysis of the muscle fibers fixing the joint;
- damage to articular structures due to tuberculosis or tumor-like formations.
swelling on the knee
swelling on the knee
If, after a fall or other injury, a person notices one or several symptoms of a dislocation, you should immediately contact a specialized clinic for help. The sooner therapeutic measures are taken, the higher the chance of a positive treatment outcome. You can also determine a dislocation yourself due to the loss of sensitivity in the foot area and its pallor. Such symptoms manifest themselves as a result of impaired blood flow.
Symptoms of dislocation
Fortunately, damage can be diagnosed immediately after it appears. One of the very first signs of injury will be the appearance of a characteristic crunch at the moment of dislocation. Minor symptoms that indicate the need to see a doctor include:
- Acute pain. Pain may vary depending on the degree of dislocation. Grade 1-2 injuries cause discomfort when trying to move the leg or lean on it. Dislocations accompanied by bone fractures cause severe pain even at rest.
- Hematomas and swelling. Swelling usually appears in the ankle area and increases within 24 hours after the injury. The more severe the damage, the more pronounced the swelling and discoloration of the skin will be.
- Changing the position of the foot. Most often, a leg frozen in an unnatural position with no way to change it signals a ligament rupture.
- Crunch. When trying to move the leg, the patient may hear clicking sounds indicating ankle displacement.
If at least one of the above symptoms occurs, you should immediately consult a doctor. After all, only an experienced specialist can determine the nature of the injury and prescribe appropriate treatment methods.
Dislocation of damage
Most often, knee dislocation occurs in the cap area. This can be determined by its characteristic jumping out of the riverbed. Such symptoms provoke not only pain, but can also cause such a serious disease as arthrosis. Children and women wearing high-heeled shoes most often suffer from injury. Often, traumatologists have to diagnose bilateral dislocations. The pathology is accompanied by:
- the occurrence of severe pain;
- leg deformity;
- swelling;
- bent leg position in a relaxed state;
- development of hemorthrosis.
Without qualified medical assistance, it is difficult to cope with an injury on your own. At Dr. Glazkov’s clinic, the patient will undergo a detailed diagnosis, during which the complexity of the situation will be revealed, after which they will be able to prescribe the necessary therapy. After providing first aid, the patient can be treated on an outpatient basis, visiting his doctor only on designated days.
reduction of the joint
realignment of the joint
Dislocation is considered a serious, dangerous injury that must be treated exclusively in a medical facility. Independent action in resolving this issue is excluded. The most common method of restoration is to realign the joint, after which it returns to its normal position. The specialist must take the time to eliminate concomitant symptoms, in particular hemorthrosis. To do this, a puncture is made, cold compresses or a splint are applied.
In the most serious cases, the patient may require surgery, followed by a long rehabilitation process, accompanied by the supervision of the attending physician. Surgery is prescribed only in case of complete rupture of tendons or ligaments. The modern equipment that Dr. Glazkov’s clinic has allows us to consider the surgical intervention minimally invasive, so the recovery period is also minimal.
Treatment of joint dislocations and reduction
Treatment of traumatic dislocations consists of reduction (relocation) and fixation of the articular elements. This procedure should be carried out immediately if the patient is in satisfactory condition.
If the dislocation is not corrected as soon as possible, this can lead to a number of complications:
- development of contracture due to contraction of muscle fibers;
- the formation of scar tissue in the joint cavity - usually at the site of a dense blood clot (fibrin).
There are two options for joint realignment:
- open;
- closed.
The open method is used if the closed method is contraindicated for medical reasons. Its essence lies in joint arthroscopy. Through surgery, the doctor removes from the joint cavity coagulated blood and articular elements destroyed due to injury. He then returns the displaced parts to their original position using lever-like movements. This is a painful procedure, so it is performed under general anesthesia. Anesthesia allows not only to achieve pain relief, but also has a relaxing effect on muscle fibers, facilitating the operation.
The closed method involves returning the articular heads to their place without surgical intervention. After reduction, the joint must be immobilized. To do this, a plaster fixing bandage is applied to it for 14–20 days. After reduction, a control x-ray is taken, which shows whether the displaced structures are in the correct position.