Habitual shoulder dislocation is a pathological condition in which dislocation of the humeral head occurs frequently, and this does not necessarily require any strong traumatic force.
Patients with this pathology quite often seek help from CELT traumatologists, since our clinic performs operations that relieve this problem.
The shoulder joint is one of the most mobile in the human body. But because of this feature, shoulder dislocations are the most common.
At CELT you can get a consultation with a traumatologist-orthopedic specialist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
shoulder dislocation
shoulder dislocation
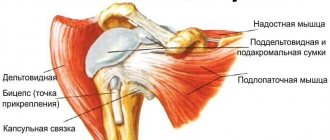
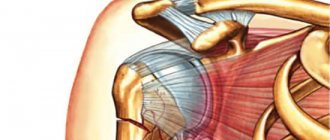
The shoulder is a complex anatomical structure. The joint has a spherical shape. The cavity is formed by the articular surfaces of the clavicle and scapula, and houses the head of the humerus. Stability is ensured by strong connective tissue ligaments.
If their anatomical integrity is violated, the strength of the fibers decreases due to injury or a pathological process, the head of the humerus comes out of the glenoid cavity and this pathological condition occurs.
Alternative Methods
- CT scan of the shoulder joint - allows you to evaluate bone changes, identify the presence of foreign bodies in the joint, a highly accurate method, but with a significant radiation exposure.
- MRI is a study of the structure of periarticular soft tissues, ligaments, tendons and cartilaginous surfaces, but the study is expensive.
- Ultrasound is a safe and accessible method for studying cartilage and soft tissue elements of the joint - synovial membrane, ligaments, periarticular structures (muscles, tendons). Detects inflammatory changes (including rheumatoid arthritis), blood, inflammatory exudate in the joint cavity.
Causes
Chronic shoulder dislocation is a polyetiological disease, the development of which can be caused by the influence of several provoking factors. These include:
- Traumatic or pathological damage to the soft structures of the shoulder that increases the depth of the glenoid cavity.
- Sprain of ligaments with a congenital decrease in their strength.
- Incorrect treatment of acute dislocation, accompanied by insufficient duration of immobilization (immobilization) of the joint or incorrect, insufficient reduction.
Acute shoulder dislocation, often leading to instability of the joint, occurs when the upper limb is sharply abducted posteriorly or is excessively rotated outward. As a result, habitual shoulder dislocation may develop. Rehabilitation and therapy necessarily take into account the causes of the pathology.
Habitual shoulder dislocation - types
In modern medicine, there are several types of this pathological condition. These include:
- Primary recurrent dislocation, often resulting from congenital ligament weakness. It usually occurs when exposed to minor functional loads.
- Secondary release of the humeral head is the result of significant traumatic damage to the joint structures, leading to its instability, as well as improper treatment of the dislocation.
Based on the frequency of development of the pathology and the strength of the mechanical impact required to remove the head of the humerus, compensated, subcompensated and decompensated habitual dislocation of the shoulder is distinguished. Surgery or conservative therapy is prescribed by a doctor after an objective diagnosis with determination of the type of pathological condition.
Habitual shoulder dislocation - symptoms
At the moment when the head of the humerus emerges from the socket, it is determined:
- joint deformity;
- deterioration of mobility in it in the form of spring resistance;
- the appearance of pain (their severity depends on the duration and frequency of development of the pathological condition);
- atypical position of the upper limb in relation to the body - a person usually holds it with his healthy hand.
Without treatment, these manifestations become more frequent. They appear when a minimal functional load is applied to the joint.
The long course of the pathological condition is characterized by the development in a person of motor stereotypes aimed at reducing movements in the area of the upper limbs.
The frequency of dislocations can reach several times a day. In this case, a person can adjust them independently or with the help of others. Painful sensations after each independent reduction are less intense and last longer.
Exercises after immobilization
When the fixation bandage is removed, you can begin to use safe exercises that eliminate sudden movements with your hands.
- Raising and lowering the shoulder.
- Gentle circular movements with minimal amplitude.
- Reduction and dilation of the shoulder blades.
- Forearm flexion.
These exercises must be performed with mandatory monitoring of the patient's condition. If any pain occurs, you should temporarily stop or reduce the intensity of exercise.
In the later stages of rehabilitation, it is necessary to perform more intense exercises, which are carried out 2-3 times a day. At this stage, weights in the form of dumbbells can be used. All exercises are aimed at strengthening the small muscles of the shoulder girdle, which are responsible for stabilizing the joint.
Diagnostics
Diagnostics
- examines the joint;
- pays attention to its configuration, the presence of an inflammatory reaction (redness of the skin, swelling of soft tissues);
- determines the possibility of performing active and passive movements, as well as their volume.
- if necessary, prescribe an additional objective study, which makes it possible to determine the nature and severity of possible damage to the joint structures.
For objective diagnosis, visualization methods are used, which include radiography (the study is carried out in frontal and lateral projection), computed or magnetic resonance imaging, which is a layer-by-layer scanning of tissues with high separation power, as well as ultrasound.
In modern medical clinics, diagnostic arthroscopy is performed to examine internal structures, which is their visualization using a small tube inserted with a camera and lighting. It can be used as a curative operation (habitual shoulder dislocation). Diagnostic prices depend on its volume and the methods used.
X-ray diagnosis of changes in the shoulder joint
A.V.Smirnov
Institute of Rheumatology, Russian Academy of Medical Sciences, Moscow
Pain in the shoulder joint is one of the most common reasons for which patients consult doctors of various specialties. Physicians must differentiate between damage to the shoulder joint itself or periarticular soft tissues and other extra-articular lesions that cause radiating pain in the shoulder joint. Such diseases include changes in the chest organs, neurological and vascular diseases, metastatic lesions of bones and soft tissues. The shoulder joints may be the site of initial manifestations of many systemic inflammatory rheumatic diseases. Pathological changes in the shoulder joints can be divided into diseases that affect the osteochondral structures of the joint, and diseases that manifest themselves as changes in the ligaments and periarticular soft tissues. The most common diseases of the shoulder joint include systemic inflammatory arthritis, arthrosis, aseptic necrosis of the humeral heads, septic arthritis, and subluxation of the shoulder joints. Diseases associated with damage to periarticular soft tissues include glenohumeral periarthritis (SLP), various types of tendonitis, including calcified tendinitis and bursitis, tears of the rotator cuff of the humerus, damage to the acromioclavicular and coracoclavicular joints.
X-ray diagnosis of PLP
X-ray diagnosis of PLP consists of signs of damage to the proximal humerus and periarticular soft tissues surrounding the shoulder joint. Radiological symptoms of damage to the humerus include osteosclerosis, unevenness and/or blurred bone contour, deformation, osteophytes at the sites of attachment of the ligaments to the greater tubercle (Fig. 1). Local, in the area of the greater tubercle, or periarticular osteoporosis, single or multiple cyst-like clearings of bone tissue in the area of the greater tuberosity and humeral head can complement the overall picture of bone damage. According to R.A. Zulkarneev [1], osteoporosis and cysts are combined in 75% of patients with PLP. Osteoporosis of the bone area adjacent to the greater tubercle refers to local pathological processes that characterize local changes in the area of the greater tubercle. Periarticular osteoporosis of the humeral head or widespread osteoporosis of the humerus and scapula can be regarded as a manifestation of systemic changes in the skeleton associated with PLP or other diseases. These diseases include osteochondrosis of the cervical spine with signs of cervical radiculitis and damage to the autonomic nervous system and persistent limitation of mobility of the shoulder joint - “frozen shoulder”. Cyst-like clearings of bone tissue can vary in shape and size, with a sclerotic rim separating the cyst from the surrounding bone tissue. Cysts against the background of osteoporosis are most clearly defined.
The second type of pathological changes in PLP is the deposition of calcium salts into the soft tissues of the shoulder joint. Most often, calcifications are determined in the thickness of the supraspinatus tendon. On a radiograph, calcifications will be visible next to the greater tubercle or slightly above it (Fig. 2). When the infraspinatus tendon is affected, the shadow of the calcification is located slightly below the greater tubercle, and if it is outward from it, then we can talk about damage to the mucous membrane of the shoulder joint bursa. In addition to these main places where calcifications are detected, calcium salts are also deposited in the muscles, in the coracoacromial and coracoclavicular ligaments. Calcium salts are most often deposited in the thickness of the tendons of the external rotators of the shoulder. Calcifications can migrate in the thickness of the soft tissues of the shoulder from the tendons of the external rotators of the shoulder outward, towards the subacromial bursa or inward, into the cavity of the shoulder joint. A characteristic feature is the lack of parallelism between clinical symptoms and the X-ray picture of PLP. Large calcifications in soft tissues, detected on radiographs, can be asymptomatic, while small and mild calcifications occur with severe pain and a sharp limitation of mobility in the joint. Calcification can be bilateral, with pain and limitation of movement detected in only one joint. Calcifications in soft tissues have a variety of shapes and sizes. They can be in the form of fuzzy linear shadows or small rounded formations in the area of the greater tubercle or reach large sizes (up to 3–4 cm in length and 1–2 cm in width), with clear, even or uneven contours, a homogeneous structure and high density , comparable to cortical bone density. Often calcium deposits do not represent a homogeneous mass, where both areas of increased and decreased density are combined.
Rice. 1. Patient Ya., 68 years old. Diagnosis: humeroscapular periatritis. Multiple osteophytes at the site of attachment of the ligaments to the greater tubercle of the humerus. Linear soft tissue calcification under the acromion process of the scapula. Linear calcification below the articular process of the scapula. Large cyst-like lucidity in the area of the greater tubercle. Osteophytes on the edges of the articular surfaces in the acromioclavicular joint.
Rice. 2. Patient P., 45 years old. Diagnosis: humeroscapular periarthritis. “Stone” bursitis. In the soft tissues above the greater tubercle of the humeral head, an oval-shaped calcification of homogeneous bone density is determined.
Rice. 3. Patient V., 31 years old. Diagnosis: rheumatoid arthritis. The joint gap is sharply narrowed. Multiple cysts in the humeral head. Erosion of articular surfaces. Subchondral osteosclerosis. Subluxation of the humerus upward. Osteophytes on the edges of the articular surfaces.
Rice. 4. The same patient as in Fig. 3. Negative dynamics of radiological changes after 9 months.
Rice. 5. Patient K., 23 years old. Diagnosis: systemic lupus erythematosus. Aseptic necrosis of the left humeral head. The gap of the shoulder joint is not narrowed. Flattening and unevenness of the contour of the articular surface, a decrease in the volume of the humeral head. Severe subchondral osteosclerosis. Calcifications in soft tissues. Osteophytes on the edges of the articular surfaces.
Rice. 6. Patient N., 38 years old. Diagnosis: systemic lupus erythematosus. Aseptic necrosis of the left humeral head. The gap of the shoulder joint is not narrowed. The articular surface of the humeral head is uneven. Deformation of the humeral head. Subchondral osteosclerosis. Cyst-like restructuring of the bone structure. Calcifications in the soft tissues under the acromion process of the scapula.
When describing radiographs of the shoulder joints in patients with PLP, attention is paid mainly to bone changes in the area of the greater tubercle and often do not notice pathological changes in the area of the apex of the acromial process of the scapula, along the lower surface of which one can see bone lesions similar to tubercles: osteosclerosis, unevenness of the bone surface, osteophytes. It is proposed to consider these changes as a whole in PLP and use the terms “acromiotubercular arthrosis” or “arthrosis of the subacromial joint” [2].
X-ray manifestations of PLP are often combined with signs of deforming arthrosis of the acromioclavicular joint, the main symptoms of which are narrowing of the joint space, osteophytes at the edges of the articular surfaces, unevenness of the articular surfaces and subchondral osteosclerosis. Small calcifications in the soft tissue may be found in the area of the upper or lower edge of the joint space.
The complex of x-ray examination for PLP must include x-ray of the cervical spine in two standard projections. Osteochondrosis of the cervical spine is often combined with PLP, but radiating pain in the shoulder joint is no less often found with the development of cervical plexitis. The absence of radiological changes in pain in the shoulder joints is a direct indication for examination of the cervical spine.
Standard AP X-rays of the shoulder joints may not detect calcareous shadows in the soft tissues, as calcifications may be located behind the greater tuberosity. In this case, it is necessary to perform a multi-view examination of the joint in the position of internal and external rotation of the shoulder joint. If you have a frozen shoulder, you can change the position of the X-ray tube relative to the shoulder joint. In the most complex cases of PLP, it is necessary to expand diagnostic methods, including computed tomography and magnetic resonance imaging of the shoulder joint.
X-ray diagnosis of arthritis of the shoulder joint Arthritis of the shoulder joint is quite often found in patients with rheumatic diseases. Arthritis of the shoulder joint most often develops in patients with rheumatoid arthritis (RA). A plain radiograph of the shoulder joint at the onset of the disease reveals periarticular osteoporosis, single or multiple cyst-like clearings of bone tissue located in the subchondral part of the humeral head and humeral process of the scapula or in the central parts of the humeral head (Fig. 3). Cyst-like clearings may alternate with areas of osteosclerosis. In later stages of shoulder arthritis, progressive destruction of the articular cartilage of the humeral head and articular process of the scapula leads to widespread and severe narrowing of the joint space (Fig. 4). This stage of arthritis is combined with the formation of large cyst-like clearings of bone tissue and the appearance of small subchondral osteosclerosis on the articulating surfaces of the bones. Erosion of the articular surfaces can be single or multiple, spreading throughout the entire articular surfaces of the humeral head and the articular surface of the humeral process of the scapula. Typical of RA is large erosion at the superior edge of the articular surface of the humeral head at the border with the greater tuberosity, which can cause a fracture with anterior displacement of the humerus. Further destruction of the bones and articular surfaces of the shoulder joint leads to the expansion and deepening of existing erosions and the appearance of new erosions over a significant area of the bone surface. Against this background, pronounced bone deformations with subluxations and dislocations of the humeral heads appear.
Arthritis of the shoulder joint occurs without the formation of pronounced osteosclerotic changes in the area of the articulating articular surfaces and without the formation of large osteophytes at the edges of the articular surfaces. Small osteophytes on the edges of the joints are detected in patients with long-term arthritis of the shoulder joints and indicate the development of secondary osteoarthritis in this joint.
RA of the shoulder joint is often combined with damage to the periarticular soft tissues. These include subacromial bursitis, tendonitis, and rotator cuff tears. Atrophy of the rotator cuff or their tears are often detected changes in long-term RA due to damage to the ligamentous apparatus of the shoulder joints by pannus. These changes on radiographs are manifested by a significant displacement of the humeral head relative to the articular process of the scapula, narrowing of the space between the upper part of the humeral head and the lower part of the acromial process of the scapula, osteosclerosis and the formation of cysts. These radiographic changes can also be found in patients with other inflammatory and non-inflammatory diseases, but the combination of anterior subluxation of the humeral head in relation to the articular process of the scapula and diffuse narrowing of the joint space of the shoulder joint is typical for RA. In some cases of shoulder RA, one or more synovial cysts may form in the surrounding soft tissues, which are better diagnosed by ultrasound examination of the joint or magnetic resonance imaging (MRI).
Along with damage to the shoulder joint, arthritis can be detected in the acromioclavicular joint, radiological changes in which will be similar to changes in the shoulder joint, while changes in these joints are interrelated. In RA, both unilateral and bilateral changes can be detected in the acromioclavicular joints. Soft tissue thickening at the anterior joint, periarticular osteoporosis, and erosions of the articular surfaces that first appear in the articular surface of the clavicle are early symptoms of arthritis. Subsequently, large erosions of the articular surface of the clavicle and, less often, in the acromion process of the scapula may appear. The eroded surface of the clavicle has uneven contours and can be evenly narrowed in the area of the articular end. The articular surface of the acromion process is more often susceptible to osteolytic changes in the bones. Along the lower edge of the acromial process of the scapula, periostitis and unevenness of the bone contour can be detected, which is the influence of the inflamed synovial membrane in the subacromial (subdeltoid) mucous membrane of the bursa. Changes in the synovial membrane in the joints and their inversions can be detected with MRI and arthrography of the shoulder joint. Arthritis in the acromioclavicular joint can be accompanied by rupture of the ligaments, capsule and subluxation in the joint, while the joint space widens.
In RA, erosions may be found along the inferior surface of the distal clavicle. Typically, these changes are detected 2–4 cm from the articular surface of the clavicle and are associated with changes in the area of the coracoid process of the scapula.
The shoulder joint is the second most important peripheral joint, most often involved in the pathological process in ankylosing spondylitis (AS) [3]. Bilateral damage to the shoulder joints is also a common manifestation of AS. The main radiological symptoms of arthritis of the shoulder joint in AS are bone porosis, narrowing of the joint space, erosion of the articular surfaces of the articulating bones, and tears of the rotator cuff. Multiple destructive changes in the articular surface of the humeral head, especially in the upper outer part, in combination with periarticular changes and slight upward subluxation of the humerus lead to the appearance of the “hatchet” symptom of the proximal humerus. Atrophy or tear of the rotator cuff leads to superior subluxation of the humerus.
Lesions of the acromioclavicular joints in ankylosing spondylitis (BD) are often bilateral and are similar in their pathological manifestations to changes in RA. In BD, resorption of the distal end of the clavicle may be detected. Damage to the coracoclavicular joint is associated with enthesopathy at the site of attachment of the ligament, inflammation in the synovial bursa, or damage to the joint itself. A distinctive property of radiological changes in BD is a combination of erosive and proliferative changes in the joints and places of attachment of ligaments, which makes it possible to carry out a differential diagnosis with other inflammatory and non-inflammatory diseases and make the correct diagnosis.
X-ray diagnosis of arthrosis of the shoulder joint The shoulder joint is not a typical joint for the development of primary osteoarthritis (OA). The presence of radiological symptoms of arthrosis in the joint indicates the secondary nature of the changes, which are primarily the result of traumatic injuries both in the osteochondral part of the joint and in cases of damage to periarticular soft tissues (microtraumatization of tissues during prolonged heavy physical load on the joint, some occupational diseases, sports injury, posterior subluxation of the humerus), after surgical interventions, as well as inflammatory and non-inflammatory changes in the shoulder joint. The latter include RA, BD, a group of microcrystalline arthritis, ochronosis, dysplasia of the bones of the shoulder joint, changes in certain neurological and hematological diseases. The main radiological symptoms of OA include osteophytes at the edges of the articular surfaces, slight narrowing of the joint space, single cyst-like clearings of bone tissue with a sclerotic rim, and osteosclerosis of the subchondral bones to varying degrees. Thinning of the articular cartilage primarily occurs in the central part of the humeral head, at the point of greatest contact with the articular surface of the scapula. Cyst-like clearings of bone tissue are found in the subchondral part of the articulating surfaces of bones. Marginal osteophytes are most often found on the lower edge of the articular surface of the humeral head. Intra-articular inclusions are not typical for OA of the shoulder joints. Degenerative changes in the shoulder joint may be associated with a subacromial spur or osteophyte.
Shoulder OA develops when the rotator cuff of the shoulder is torn. The main radiological symptoms are upward displacement of the humeral head relative to the articular surface of the articular process of the scapula, while the distance between the humeral head and the acromial process of the scapula decreases, osteosclerosis and cystic clearing of the bone tissue of the articulating surfaces of the bones develop.
OA of the acromioclavicular joint is most often found in older people and can be the cause of vague shoulder pain. X-ray changes are characterized by narrowing of the joint space, compaction of bone tissue in the subchondral bones, and the formation of osteophytes at the edges of the articular surfaces of the clavicle and acromion process of the scapula. Bone hypertrophy, downward displacement of the acromial end of the scapula, bone proliferation on the upper edge of the acromion, and involvement of the ligaments surrounding the acromioclavicular joint in the pathological process may also be detected.
X-ray diagnosis of aseptic necrosis (osteonecrosis) of the humeral head Osteonecrosis mainly develops in the humeral head and is a consequence of various diseases. The most common cause of avascular necrosis (AN) of the humeral head is avascular necrosis of the bone due to a fracture in the area of the anatomical neck of the humeral head [4]. A fracture of the humerus in this area ruptures the intraosseous vessels and vessels of the capsule of the shoulder joint, which supply the humeral head, which is the cause of the development of AN.
Another cause of AN is therapy with glucocorticoid hormones (GCs), which are taken for a long time and in large doses by patients with systemic lupus erythematosus, dermatomyositis and some other diseases. The mechanism of development of AN during the use of GCs remains not fully understood to date. At the same time, hypotheses are considered regarding the relationship of AN with vasculitis, which is characteristic of many rheumatic diseases [5–7], as well as with osteoporosis, which accompanies chronic inflammation and GC intake, leading to bone microfractures, which leads to vascular compression and microcirculation impairment. The congenital predisposition to the development of osteonecrosis in this group of patients is also discussed. In some cases, AN appears early, at the very beginning of taking GC, although symptoms of the disease may appear in more distant periods of the disease. The pathogenesis of AN during GC intake, according to R. Ficat and J. Arect [8], is explained by an increased content of free fatty acids, which thrombose intraosseous vessels against the background of systemic vasculitis associated with the underlying disease. Blockage of the supply vessels increases intraosseous pressure in the humeral head, leading first to ischemia of the bone area and subsequently to AN of the humeral head.
The stages of AN are resorption, sequestration, repair, sclerosis and remodeling of the humeral head. In the initial stage of AN, radiological changes in bone tissue may be absent, so early diagnosis of pathological changes requires the use of MRI. If there is a history of risk factors for the development of AN (for example, trauma), timely identified symptoms of AN contribute to an earlier start of therapeutic measures aimed at eliminating the causes and the choice of the correct treatment tactics for patients.
The initial radiological manifestations of AN of the humeral head at the stage of bone tissue resorption should be considered an increase in radiolucency and rarefaction of the trabecular bone structure in the subchondral bone with the formation of either a linear zone of clearing of bone tissue running along the articular surface of the humeral head, or this may be an area of cyst-like clearing of bone tissue or multiple small cysts, alternating with small areas of compaction of bone tissue of a round or linear shape, as in the first case, located subchondral. At this stage of the disease, the humeral head can retain its round, spherical shape, clear, even contours of the articular surface and the normal width of the joint space.
At the stage of sequestration in the AN zone, a necrotic area of bone and a zone of preserved healthy bone tissue are clearly visualized on an x-ray of the shoulder joint. The area of necrosis is defined as a round, oval or irregularly shaped dense shadow. It is often localized in the central part of the humeral head. The focus of necrosis may be surrounded by a linear zone of clearing. At the base of the necrosis zone, an area of osteosclerosis is found, which is a compensatory reaction of the bone, delimiting the affected area from healthy bone [9]. The joint space at this stage of the disease can be widened to the greatest extent over the area of necrosis. The articular surface of the humeral head loses its regular rounded shape, becomes flattened, and the humeral head as a whole becomes deformed (Fig. 5, 6).
Subsequently, as the resorption of necrotic bone tissue increases, reparative processes on the part of healthy bone tissue begin to increase. X-ray changes at this stage are characterized by the appearance of secondary deforming arthrosis of the shoulder joint in the form of the formation of osteophytes on the edges of the articular surfaces of the humeral head and the articular process of the scapula, narrowing of the joint space throughout, non-growth of osteosclerotic changes in the humeral head, pronounced deformation changes in the bones, in some cases, subluxation of the humerus bones up.
The stages of AN of the humeral head are similar in their radiological manifestations to the changes found in AN of the femoral head in patients with rheumatic diseases. Radiological stages of AN of the femoral heads can be used to describe AN of the humeral heads [10].
Computed tomography and MRI Standard computed tomography (CT) or in combination with arthrography is one of the main diagnostic methods for assessing the musculoskeletal system of the shoulder joint. CT is the method of choice for various traumatic injuries of the shoulder joint; it allows one to evaluate bone, cartilage and soft tissue post-traumatic changes, and determines loose bodies in the joint cavity M. Rafii et al. [11] report high accuracy (up to 95%) in identifying injuries to the proximal humerus, articular surfaces of the humeral head, and articular process of the scapula. CT is also a unique diagnostic tool for the study of subluxations, dislocations and for determining the thickness of the rotator cuff of the humerus, which is necessary for decisions regarding surgical intervention on the shoulder joint.
MRI is a unique research method that allows for complete visualization of all joint structures and includes assessment of bone tissue and bone marrow, articular cartilage, menisci, joint synovium and intra-articular fluid, intra-articular ligaments, adipose tissue, joint capsule, periarticular muscles and ligaments.
MRI is used to examine the structure of the periarticular soft tissues to diagnose partial or complete tears of the rotator cuff of the shoulder joint, synovitis, damage to the articular cartilage and cartilaginous labrum of the scapula, as well as in subluxations or dislocations of the humeral head [12, 13]. In RA, MRI is a more sensitive diagnostic method than direct radiography of the shoulder joint in detecting soft tissue changes and bony changes in the humeral head and articular process of the scapula.
References 1. Zulkarneev R.A. “Painful shoulder”, glenohumeral periarthritis and “shoulder-hand” syndrome. Kazan: Kazan University, 1979; 309 p. 2. Tretyakova G.A. Author's abstract. diss. ...cand. honey. Sci. L., 1967. 3. Resnick D. Radiology 1977; 110: 523. 4. Neer CS. In: Rockwoods C. and Green D. (eds). Fractures. Philadelphia, JBLippincott Company, 1975. 5. Olyunin Yu.A. Ischemic bone necrosis. Rheumatic diseases. Ed. V.A.Nasonova, N.V.Bunchuk. M.: Medicine, 1997. 6. Klippel J, Dieppe P. Rheumatology 1997; 2:6–8. 7. Stinberg M, Stinberg D. Osteonecrosis. Textbook of Rheumatology. 1993; P. 1628–50. 8. Ficat RP, Arlet J. Ischemia and Necrosis of the Bone. Baltimore, Williams and Wilkins, 1980. 9. Mikhailova N.M., Malova M.N. Idiopathic aseptic necrosis of the femoral head in adults. M.: Medicine, 1982; 134 p. 10. Smirnov A.V. Consilium medicum 2003; 5 (8): 442–6. 11. Rafii M, Minkoff J, Bonano J et al. Am J Sport Med 1988; 16 (4): 352. 12. Zlatkin M, Reicher M, Kellerhouse L et al. J Comput Assist Tomogr 1988; 12 (6): 995. 13. Seeger L, Gold R, Bassett L. Radiology 1988; 168(3):696.
Source: https://www.consilium-medicum.com
Habitual shoulder dislocation - treatment
Treatment of this pathological condition, which involves repeated emergence of the head of the humerus from the socket, is complex. It includes conservative measures and surgical intervention followed by rehabilitation.
All events are carried out in stages and follow each other. Usually, conservative therapy is first prescribed at the stage of preoperative preparation. Then surgery is performed. It is aimed at restoring the stability of the joint, which was disrupted by habitual shoulder dislocation. After the operation, rehabilitation measures are carried out.
Conservative therapy
Treatment with medications is usually prescribed as preoperative preparation. In case of an inflammatory reaction, non-steroidal anti-inflammatory drugs are used. Also, if necessary, drugs are used to improve blood clotting and antibiotics to prevent secondary bacterial infection.
To improve the condition of the ligamentous apparatus and increase the strength of connective tissue fibers, physiotherapeutic procedures are performed, including electrophoresis with anti-inflammatory drugs, magnetic therapy, mud baths, and ozokerite. The scope of conservative measures is usually greater when planning open access surgery.
operations
operations
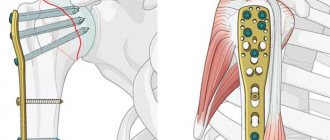
These types of surgical intervention can be performed using arthroscopy or open access. The choice of technique is determined by the doctor based on objective research data, as well as the technical capabilities of the medical clinic.
Arthroscopic operations
In modern medical clinics, whenever possible, arthroscopy is used, which makes it possible to correct habitual shoulder dislocations using small incisions. The cost of the operation and the overall course of treatment is lower, since the duration of the postoperative and rehabilitation period is noticeably reduced.
Arthroscopy is the method of choice, with which it is possible to effectively treat habitual shoulder dislocation. Video on the monitor allows the doctor to visually monitor the manipulations performed using special micro-instruments.
Open access operations
In case of significant violation of the anatomical integrity, leading to instability of the joint, plastic surgical interventions are performed using an open approach. To do this, wide incisions are made in the skin, subcutaneous tissue and capsule, allowing wide access to the structures being restored.
This type of surgical intervention can be used if it is necessary to perform osteoplastic surgery with implantation.
When surgical intervention is performed using an open approach to restore stability in such a pathological condition as a habitual dislocation of the shoulder, the prices are higher. This is due to the peculiarities of the operation, the need for a longer preoperative and rehabilitation period, and the frequent use of a significant number of drugs of various pharmacological groups.
treatment without surgery
treatment without surgery
Treatment without surgery is possible with a compensated course of the pathological process. It includes physiotherapeutic procedures and physical therapy with the limitation of certain movements in the shoulder joint. Such therapeutic results are rather low in effectiveness.
Habitual shoulder dislocation – recovery after surgery
Rehabilitation after a habitual shoulder dislocation involves applying a plaster cast for a long period of time (several months). Then physical therapy is prescribed with a gradual increase in the load and range of motion in the joint.
Orthopedics and traumatology services at CELT
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a surgical doctor (primary, for complex programs) | 3 000 |
| Ultrasound of two symmetrical joints (except hip) | 4 000 |
| X-ray of bones and joints of the limbs | 2 200 |
| MRI of the shoulder joint (1 joint) | 7 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions