Definition
Tooth displacement of the axial vertebra is one of the malformations in the upper cervical region, which consists of backward deviation of the axis, which leads to displacement and compression of nearby nerve structures. The axis tooth extends beyond the imaginary line between the sphenoid process and the angle of the posterior wall of the C2 vertebra. Often accompanied by platybasia and basilar impression.
Fig. 1 Displacement of an axial vertebral tooth on a CT image.
Symptoms
Symptoms of malformation of tooth displacement of the axial vertebra form part of the clinical picture of basilar impression and platybasia, as a consequence of axis pressure on the spinal cord trunk and nearby vessels. Neurological manifestations are associated with compression of the spinal cord in the upper cervical region: neck pain, contractures (limited mobility), loss of strength, spasticity, paresis, unsteady gait, gradual loss of sensation. May also affect chronic increases in intracranial pressure.
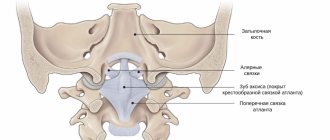
Anatomy of the human Atlanto-occipital joint - information:
Atlanto-occipital joint, art. atlantooccipitdlis , belongs to the condylar; it is formed by two condyles of the occipital bone, condyli occipitales, and the concave superior articular fossae of the atlas, foveae articulares superiors atlantis. Both pairs of articular surfaces are enclosed in separate articular capsules, but move simultaneously, forming a single combined joint.
Auxiliary ligaments:
- anterior, membrana atlantooccipitalis anterior, stretched between the anterior arch of the atlas and the occipital bone;
- the posterior one, membrana atlantooccipitalis posterior, is located between the posterior arch of the atlas and the posterior circumference of the foramen magnum.
In the atlanto-occipital joint, movement occurs around two axes: frontal and sagittal. Around the first of them, nodding movements are made, i.e., bending and extending the head forward and backward (expressing agreement), and around the second axis, tilting the head to the right and left. The sagittal axis is slightly higher at its anterior end than at its posterior end. Due to this oblique position of the axis, simultaneously with the lateral tilt of the head, a slight rotation in the opposite direction usually occurs.
Joints between the atlas and axial vertebra
There are three joints here. Two lateral joints, artt. atlantoaxiales laterales , formed by the lower articular fossae of the atlas and the upper articular fossae of the axial vertebra in contact with them, forming a combined articulation. The tooth located in the middle, dens axis, is connected to the anterior arch of the atlas and the transverse ligament, lig. transversum atlantis, stretched between the inner surfaces of the lateral masses of the atlas. The tooth is covered by an osteofibrous ring formed by the anterior arch of the atlas and the transverse ligament, resulting in a cylindrical rotatory joint, art. atlantoaxidlis medna.
Two fibrous bundles extend from the edges of the transverse ligament: one upward, to the anterior circumference of the large foramen of the occipital bone, and the other downward, to the posterior surface of the body of the axial vertebra. These two bundles, together with the transverse ligament, form the cruciate ligament, lig. cruciforme atlantis. This ligament is of great functional importance: as already noted, on the one hand, it is the articular surface for the tooth and directs its movements, and on the other hand, it keeps it from dislocation, which could damage the spinal cord and the medulla oblongata nearby near the large foramen of the occipital bone, which leads to death.
The auxiliary ligaments are lig. apicis dentis, coming from the apex of the tooth, and ligg. alaria - from its lateral surfaces to the occipital bone. The entire described ligamentous apparatus is covered from behind, from the side of the spinal canal, by a membrane, membrana tectoria (continuation of the lig. longitudinale posterius, spinal column), coming from the slope of the occipital bone.
In artt. atlantoaxiales, the only kind of movement occurs - rotation of the head around a vertical axis (turn to the right and left, an expression of disagreement) passing through the tooth of the axial vertebra, and the head moves around the process along with the atlas (cylindrical joint). At the same time, movements occur in the joints between the atlas and the axial vertebra. The apex of the tooth during the rotational movement is held in its position by the above-mentioned ligg. alaria, which regulate movement and thus protect the adjacent spinal cord from shocks.
Movements in the connections of the skull with the two cervical vertebrae are small. More extensive movements of the head usually occur with the participation of the entire cervical part of the spinal column. The cranial-vertebral joints are most developed in humans due to upright posture and head elevation.
Computed tomography or MRI
The diagnosis of axial vertebral displacement can be made using a CT scan of the skull (Fig. 1) or an MRI of the brain or cervical spine (Fig. 2).
Rice. 2.- MRI of the brain and cervical spine. There is a displacement of the tooth of the axial vertebra. In addition, the following are visible: basilar impression, angular bending of the brain stem, prolapse of the cerebellar tonsils. There is also enlargement of the supracerebellar space, a finding that favors the spinal cord traction theory and contradicts the malformation/foramen magnum theory.
Connection of the I and II cervical vertebrae between themselves and the skull
The connections of the condyle in the occipital bone with the superior articular fossae of the atlas form a combined ellipsoidal atlantooccipital joint (articulatio atlantooccipitalis). In the joint, movements around the sagittal axis are possible - tilting the head to the sides and around the frontal axis - flexion and extension.
The connection of the atlas and the axial vertebra forms 3 joints: a paired combined flat lateral atlantoaxial joint (articulatio atlantoaxial lateralis), located between the lower articular surfaces of the atlas and the upper articular surfaces of the axial vertebra; unpaired cylindrical median atlantoaxial joint (articulatio atlantoaxialis medialis), between the tooth of the axial vertebra and the glenoid fossa of the atlas. The joints are strengthened by strong ligaments.
Between the anterior and posterior arches of the atlas and the edge of the foramen magnum, the anterior and posterior atlantooccipital membranes (membranae atlantooccipitales anterior et posterior) are stretched. The transverse ligament of the atlas (lig. trasversum atlantis) spans between the lateral masses of the atlas.
A fibrous cord runs from the upper free edge of the transverse ligament to the anterior semicircle of the foramen magnum. A fibrous bundle runs from the lower edge of the same ligament down to the body of the axial vertebra. The upper and lower bundles of fibers together with the transverse ligament form the cruciate ligament of the atlas (lig. cruciforme atlantis). Two pterygoid ligaments (ligg. alaria) extend from the upper part of the lateral surfaces of the odontoid process, heading to the condyles of the occipital bone.{banner_st-d-1}
The connection of the cervical vertebrae with each other and with the skull: a - cervical spine, view from the right side: 1 - interspinous ligament; 2 - yellow ligaments; 3 - nuchal ligament; 4 - posterior atlanto-occipital membrane; 5 - anterior atlanto-occipital membrane; 6 - anterior longitudinal ligament;
b — upper part of the spinal canal, posterior view. The vertebral arches and spinous processes were removed: 1 - lateral atlantoaxial joint; 2 - atlanto-occipital joint; 3 - occipital bone; 4 - covering membrane; 5 - posterior longitudinal ligament;
c — in comparison with the previous figure, the integumentary membrane has been removed: 1 — transverse ligament of the atlas; 2 - pterygoid ligaments; 3 - cruciate ligament of the atlas;
d - in comparison with the previous figure, the cruciate ligament of the atlas was removed: 1 - ligament of the apex of the tooth; 2 - pterygoid ligament; 3 - atlanto-occipital joint; 4 - lateral atlantoaxial joint;
e — median atlantoaxial joint, top view: 1 — transverse atlas ligament; 2 - pterygoid ligament
Causes
– According to traditional theories:
Like all anomalies at the junction of the skull and neck, tooth displacement of the axial vertebra is usually attributed to congenital (structural or general) or acquired disorders.
– According to the Filum System ® sanitary method:
The deformation observed when a tooth in an axial vertebra is displaced is associated with the asynchronous growth of the spinal cord (and with it the central nervous system) and the spine during the developmental phase of the embryo. This provokes the appearance of abnormal tension in the spinal cord, which is transmitted by a tense and short filum terminale from the coccyx to the skull. The stronger and earlier the abnormal tension of the filum terminale manifests itself, the more manifestations in bone malformations can occur, the more severe the displacement can be. Displacement of the axial vertebral tooth occurs for the same reason as Arnold Chiari I syndrome, idiopathic syringomyelia and scoliosis, and other bone deformities in the foramen magnum area associated with tension in the filum terminale. The earlier and more intense the tension of the spinal cord manifests itself, coinciding with the stage of formation and growth of bones, the more pronounced the displacement of the tooth of the axial vertebra, basilar impression and platybasia manifest themselves.
Complications
Complications from displacement of an axial vertebral tooth may depend on the degree of tension or mechanical conflict in the occipital region.
- Deterioration in quality of life: torticollis, limited neck mobility, pain in the back of the head and neck, loss of strength in the limbs, spasticity, unsteadiness when walking and loss of sensation can become chronic, increasing in intensity, each time worsening the patient’s condition, limiting his normal lifestyle.
- Chronic pain: Patients, especially those with axial tooth displacement combined with Arnold Chiari syndrome and/or basilar impaction, may require treatment in a pain management department because conventional anti-inflammatory and pain medications may not be effective in treating headache attacks and other symptoms.
- Sudden death: May be associated with damage to the spinal cord, where cardiorespiratory control is located. Breathing disorders during sleep can be part of the pathology: apnea, respiratory arrest and even sudden death of the patient. That is why timely diagnosis and early treatment are so important.
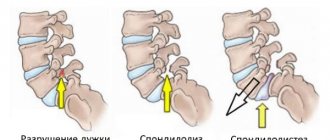
Vertebral body hemangioma
The news of a vertebral body hemangioma very often causes anxiety and concern about one’s health. And this is not surprising, since hemangioma is a vascular tumor. However, in most cases, these worries are in vain, because not everyone and not always need to treat such a tumor.
How are hemangiomas detected?
In most cases, hemangiomas do not manifest themselves in any way and are found in every tenth person as an accidental finding during examination. Most often, these benign tumors are found in the thoracic and lumbar spine and are located inside the vertebral body.
Typically, hemangiomas are detected when visiting a neurologist for back pain. An examination is prescribed - x-ray, MRI or CT. In conclusion, many changes in the vertebrae are often described (for example, osteochondrosis, osteophytes, hernias), which can indeed be the cause of pain. And often in the conclusion to the study a small vertebral body hemangioma is described.
Treatment
O tratamento convencionalmente aceito para a Retroflexão do Odontóide é neurocirúrgico. Typically, when a tooth in an axial vertebra is displaced, neurosurgical treatment is used. Currently, decompression or trepanation of the foramen magnum is the standard treatment for this diagnosis in most medical centers in the world. It is usually prescribed in cases where the symptoms cause more damage and mortality than the natural progression of the pathology. However, since 1993, after the publication of the doctoral dissertation of Dr. Royo Salvador, who linked the tension of the entire nervous system with the filum terminale, the tension of which provokes, among other diseases, prolapse of the cerebellar tonsils, a new treatment , etiological, that is, eliminating the cause of the disease with surgical dissection of the filum terminale , which removes the pathological tension mechanism. Our technique of filum terminale dissection is minimally invasive and is prescribed in all cases of filum terminale disease, both symptomatic and asymptomatic, and as early as possible, since the risks are minimal and much lower than from the pathology itself, in addition, this treatment stops further development of the disease.
Minimally invasive dissection of the filum terminale using the Filum Sistem® method:
Advantages
1. Eliminates the cause of tooth displacement of the axial vertebra and associated pathologies.
2. Eliminates the mechanism that causes pressure in the foramen magnum, and with it the risk of sudden death.
3. 0% mortality, without consequences in more than 1500 patients operated on using the Filum System® method.
4. Using the minimally invasive surgical technique of the Chiari Institute of Barcelona, the surgical time is 45 minutes. Stay in the hospital for about a day. The post-operative period is short and without serious restrictions.
5. Improves symptoms, stops the development of the pathological tension mechanism.
6. Eliminates the risk of hydrocephalus due to the descent of the tonsils into the foramen magnum, which is often associated with basilar impression.
7. Improves blood supply to the entire nervous system and, at the same time, cognitive capabilities, which may suffer due to spinal cord tension.
Flaws
1. A small suture in the coccyx area; complications such as suture infection and hematoma in the operation area are possible.
2. Decreased spasticity is sometimes mistaken for loss of strength in the limbs.
3. During the process of restoration and improvement of sensitivity, unpleasant sensations may appear, which are usually mistaken for undesirable consequences.
4. With improved blood supply to the brain, brain activity may increase and mood swings may occur during the initial post-operative period.
Occipital craniotomy:
(Decompression of the foramen magnum)
Advantages
1. Avoiding the risk of sudden death.
2. The condition of some patients improves.
Flaws
1. Does not eliminate the cause of the disease.
2. Mortality from 0.7 to 12%, a higher percentage than sudden death with spontaneous development of the disease.
3. Aggressive surgery, crippling and with possible consequences.
4. Small percentage of improvement and for a short period (on average, about ten years).
5. Neurological deficit: depends on the location of the injury: Emiparesia (paralysis of half the body from 0.5 to 2.1%. Changes in visual space from 0.2 to 1.4%. Changes in speech from 0.4 to 1%. Lack of sensitivity from 0.3 to 1%. Lack of balance, difficulty walking from 10 to 30%.
6. Postoperative intracerebral hemorrhage in the operated area, epidural hematoma, intra-axial hemorrhage, which can cause neurological deficit or worsening of a pre-existing deficit (0.1 to 5%).
7. Brain edema, depending on the process and situation, the risk reaches 5%.
8. Superficial, deep or intracranial infection, risk from 0.1 to 6.8%, with the formation of a brain abscess, aseptic-septic meningitis.
9. Hemodynamic changes due to manipulation of disorders in the brain stem.
10. Gas embolism (in patients in a sitting position).
11. Cerebrospinal fluid output is from 3 to 14% (cerebrospinal fluid fistula).
12. Postoperative hydrocephalus.
13. Pneumoencephaly.
14. Tetraparesis (loss of strength in all limbs).
To the joints of the occipital bone, atlas and axial vertebra
include the following.
Atlanto-occipital joint, arliculatio atlantooccipitalis,
paired;
it is formed by the articular surface of the occipital condyles, condyli occipilales, and the superior articular fossa of the atlas, fovea articularis superior. The articular capsule is attached along the edge of the articular cartilage. Based on the shape of the articular surfaces, this joint belongs to the group of ellipsoidal joints, articulatio ellipsoidea. In both, right and left, joints that have separate articular capsules, movements occur simultaneously, i.e. they form one combined joint; Nodding (bending forward and backward) and slight lateral movements of the head are possible. The anterior atlanto-occipital membrane, tetbrapa atlantooccipitalis anterior,
stretches along the entire gap between the anterior edge of the foramen magnum and the upper edge of the anterior arch of the atlas; fused with the upper end of the lig. longitudinale anterius.
Posterior atlantooccipital membrane, membrana atlantooccipitalis posterior,
located between the posterior edge of the foramen magnum and the upper edge of the posterior arch of the atlas. This membrane is a modified ligamentum flavum. When the atlas and axial vertebra articulate, three joints are formed: two paired and one unpaired:
Lateral atlantoaxial joint, articulatio atlantoaxialis lateralis, -
a paired combined joint, formed by the upper articular surfaces of the axial vertebra and the lower articular surfaces of the atlas. It belongs to the type of low-moving joints, since its articular surfaces are flat and even. In this joint, sliding occurs in all directions of the articular surfaces of the atlas in relation to the axial vertebra.
Median atlantoaxial joint, articulatio atlantoaxialis mediana,
is formed between the posterior surface of the anterior arch of the atlas { fovea
the tooth of the axial vertebra.
In addition, the posterior articular surface of the tooth forms a joint with the transverse atlas ligament. The joints of the tooth belong to the group of cylindrical ones and in them it is possible to rotate the atlas together with the head around the vertical axis of the tooth along the axial vertebra, i.e., rotation of the head to the right and left. The ligamentous apparatus of the two joints described includes:
• the integumentary membrane, membrana tectoria.
This membrane is called the integumentary membrane because it covers the back (from the side of the spinal canal) of the tooth, the transverse ligament of the atlas and other formations of this joint. It is considered as part of the posterior longitudinal ligament of the spinal column;
• cruciate ligament of the atlas, lig. cruciforme atlantis,
consisting of longitudinal and transverse beams.
Transverse beam
called the transverse
transversum atlantis,
and is a dense connective tissue cord stretched between the internal parts of the massa lateralis atlantis.
It is adjacent to the posterior articular surface of the tooth of the axial vertebra and strengthens it. The longitudinal fasciculus, fasciculus iongitudinalis, consists of two legs:
• superior leg
comes from the middle part of the transverse ligament of the atlas and reaches the anterior surface of the foramen magnum;
• lower leg
also starts from the middle part of the transverse ligament, goes down and is attached to the posterior surface of the body of the axial vertebra.
Ligament of the apex of the tooth, lig. apicis dentis,
extends between the apex of the tooth of the axial vertebra and the middle part of the anterior edge of the foramen magnum. This ligament is considered a rudiment of the dorsal string, chorda dorsalis.
Pterygoid ligaments, ligg. alaria,
formed by bundles of connective tissue fibers stretched between the lateral surfaces of the tooth of the axial vertebra and the internal surfaces of the occipital condyles, condyli occipilales.
3. The long ligaments of the spinal column include the following elements.
Anterior longitudinal ligament, lig. longitudinale anterius,
runs along the anterior and partly lateral surfaces of the vertebral bodies from the anterior tubercle of the atlas to the sacrum, where it is lost in the periosteum of the I and II sacral vertebrae. Limits excessive extension of the spinal column. The anterior longitudinal ligament in the lower parts of the spinal column is much wider and stronger; it connects loosely with the vertebral bodies and tightly with the intervertebral cartilage, as it is woven into the perichondrium covering them; on the sides of the vertebrae it continues into their periosteum. The deep layers of the bundles of this ligament are somewhat shorter than the superficial ones, due to which they connect adjacent vertebrae with each other, and the superficial, longer bundles lie over 4-5 vertebrae.
Posterior longitudinal ligament, lig. longitudinale posterius,
located on the posterior surface of the vertebral bodies in the spinal canal, canal is vertebralis.
The posterior longitudinal ligament, in contrast to the anterior one, is wider in the upper part of the spinal column than in the lower part.
The superficial bundles of this ligament, as in the anterior longitudinal ligament, are longer than the deep ones.
Yellow ligaments, ligg. flaves,
fill the spaces between the vertebral arches from the axial vertebra to the sacrum. They are directed from the inner surface and lower edge of the arch of the overlying vertebra to the outer surface and upper edge of the arch of the underlying vertebra and, with their anterior edges, limit the intervertebral foramina from behind. They reach their greatest development in the lumbar region. The yellow ligaments are very elastic, consisting of vertically running elastic bundles, giving them a yellow color. When the torso is extended, they shorten and act like muscles, keeping the torso in a state of extension and reducing muscle tension. When flexed, they stretch and thereby also reduce the tension of the rectus abdominis.
There are no yellow ligaments between the arches of the atlas and the axial vertebra. The connective tissue atlanto-axial membrane is stretched here
which, with its anterior edge, limits behind the intervertebral foramen, foramen intervertebrale, through which the second cervical nerve exits.
Interspinous ligaments, ligg. interspinalia
- thin plates that fill the spaces between the spinous processes of two adjacent vertebrae. At the front they are connected to the ligg. flava; and behind, at the apex of the spinous process, they merge with the supraspinous ligament.
Supraspinous ligament, lig. supraspinale,
It is a continuous cord running along the tops of the spinous processes of the vertebrae in the lumbar and thoracic regions. Below, it is lost on the spinous processes of the sacral vertebrae, at the top, at the level of the protruding vertebra, it passes into the rudimentary nuchal ligament.
Nuchal ligament, lig. nuchae, -
a thin plate consisting of elastic and connective tissue bundles; is directed from the spinous process of the protruding vertebra along the spinous processes of the cervical vertebrae upward and, expanding slightly, is attached to the external occipital crest and external occipital protrusion (it has the shape of a triangular plate).
Intertransverse ligaments, ligg. intertransversaria,
They are thin bundles, weakly expressed in the cervical and partly thoracic regions and more developed in the lumbar region; paired ligaments connecting the tops of the transverse processes of adjacent vertebrae limit lateral movements of the spine in the opposite direction.
Bibliography:
- Dr. Miguel B. Royo Salvador (1996), Siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas, etiología común (PDF). REV NEUROL (Barc); 24 (132): 937-959.
- Dr. Miguel B. Royo Salvador (1996), Platibasia , impresión basilar, retroceso odontoideo y kinking del tronco cerebral, etiología común con la siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas (PDF). REV NEUROL (Barc); 24 (134): 1241-1250
- Dr. Miguel B. Royo Salvador (1997), Nuevo tratamiento quirúrgico para la siringomielia , la escoliosis , la malformación de Arnold-Chiari , el kinking del tronco cerebral, el retroceso odontoideo, la impresión basilar y la platibasia idiopáticas (PDF). REV NEUROL; 25 (140): 523-530
- M. B. Royo-Salvador, J. Solé-Llenas, J. M. Doménech, and R. González-Adrio, (2005) “Results of the section of the filum terminale in 20 patients with syringomyelia , scoliosis and Chiari malformation .” (PDF). Acta Neurochir (Wien) 147:515–523.
- M. B. Royo-Salvador (2014), “Filum System® Bibliography” (PDF).
- M. B. Royo-Salvador (2014), “Filum System® Guía Breve.”
Filum terminale disease
After the research of Dr. Royo Salvador and his doctoral dissertation (1992), it was found that several diseases whose cause was previously unknown, such as: Arnold Chiari I syndrome, idiopathic Syringomyelia and Scoliosis, Platybasia, Basilar Impression, Axial vertebral tooth displacement, An angular bend at the level of the arch of the atlas is part of a new pathology - Diseases of the filum terminale - and arises for the same reason: tension in the spinal cord and the entire nervous system. The tension force of the entire nervous system during filum terminale disease is present during the formation of all human embryos; to a greater or lesser extent, everyone suffers from its consequences and various forms of manifestation and intensity. The following diseases may be associated with filum terminale disease: intervertebral hernias, some cerebrovascular insufficiency syndromes, facet syndrome, Bostrup syndrome, fibromyalgia, chronic fatigue, nocturnal enuresis, urinary incontinence and acute paraparesis. For accurate diagnosis, selection of treatment and monitoring of a patient with filum terminale disease, the Filum System® method was created.