28 February 2020
91948
1
3.7 out of 5
The intervertebral disc of the lumbar region is a fibrocartilaginous formation, the shape of which is close to an oval. It is formed by an elastic nucleus pulposus and a strong fibrous membrane and acts as a shock absorber between the vertebral bodies.
The intervertebral discs of the lumbar spine are the largest and most often susceptible to degenerative changes due to the highest level of mobility and the load received.
What is lumbar disc protrusion?
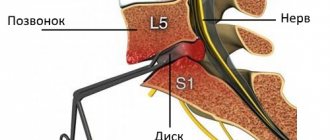
The lumbar spine is formed by 5, sometimes 6 vertebrae. Between them are intervertebral discs, which are designated depending on which vertebral bodies they are located between: L1–L2, L2–L3, L3–L4, L4–L5. Their nutrition is carried out through the circulatory system of the vertebrae and diffusely through the upper and lower surfaces of the disc (endplates).
They are natural gaskets between the bone elements of the spine and ensure the preservation of their integrity, stability of position, as well as mobility and flexibility of the ridge.
Protrusions of the lumbar spine account for about 90% of all cases of their formation. They most often occur in the L5–S1 and L4–L5 discs.
Age-related changes, the negative effects of external factors, a sedentary lifestyle and a number of other reasons lead to disruption of blood circulation and disk nutrition. The consequence is degenerative-dystrophic processes in the disc, i.e. osteochondrosis develops.
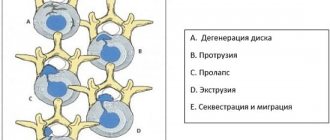
If left untreated, degenerative changes progress, spreading to the marginal plates and causing them to become sclerotic. This prevents the flow of nutrients into the nucleus pulposus, which provokes a decrease in the moisture content in it and the occurrence of nutritional deficiency. This subsequently leads to the formation of protrusion. In such situations, the disc is already so damaged that its shape is deformed, the fibrous ring becomes thinner and a slight protrusion forms.
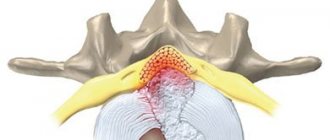
After all, a lack of water and nutrients leads to the separation of collagen fibers, from which the fibrous ring is formed, as well as their microtears. This creates the preconditions for the nucleus pulposus to move towards the area of thinning, which puts increased pressure on the already deformed annulus fibrosus. Gradually, it ceases to cope with the increased load, an even greater number of collagen fibers are torn, which leads to the bulging of the disc into the spinal canal.
As long as the integrity of the fibrous ring is preserved, they speak of the presence of protrusion. But in the absence of therapy, the pressure of the nucleus pulposus on the fibrous membrane does not disappear, so more and more collagen fibers are destroyed. As a result, the fibrous ring ruptures, and the internal contents of the disc are able to come out into the spinal canal. This is how a hernia is formed.
Thus, protrusion is a manifestation of osteochondrosis, manifested by the formation of a slight protrusion of the intervertebral disc beyond the physiological boundaries, but while maintaining the integrity of the fibrous ring.
Today, osteochondrosis occurs in people of all ages and is extremely rarely diagnosed in the early stages. Usually the disease is detected when it has already led to protrusion, since even minor changes in the condition of the lumbar intervertebral discs lead to pain and other disorders.
Danger of thoracic protrusion
Protrusion of the thoracic region occurs in only 1% of cases of patients diagnosed with this disease, but this does not make it less dangerous to health than other types of disc protrusion. Lack of proper treatment can cause progression of the disease and serious complications:
- cardiac disorders;
- disruption of the gastrointestinal tract (gastritis, inflammation of the pancreas, colitis, etc.);
- obstruction of cerebral circulation and risk of stroke.
The most dangerous situation is when compression of the spinal nerve fibers in the sternum occurs. This can cause loss of sensation in the limbs, dysfunction of the pelvic organs, and paralysis.
For successful treatment, it is necessary to seek professional help in a timely manner. The earlier the disease is detected, the higher the chance of therapy being effective.
Come to the IntegraMed CDC (formerly NDC) for diagnostics and treatment. Make an appointment with a neurologist at the clinic for FREE. For details, please contact our call center operators.
Stages and types
Depending on the severity of the situation, there are 3 stages of development of lumbar protrusion:
- Mild - the protrusion is barely noticeable, so even with the use of modern high-precision examination methods, not every specialist will be able to notice it. The dimensions of the protrusion do not exceed 1 mm.
- Moderate – the protrusion increases and already reaches 1–3 mm.
- Severe – the formation of a bulging intervertebral disc is no longer in doubt. It is clearly visualized beyond the boundaries of the vertebral bodies and has dimensions from 3 to 6 mm. But the annulus fibrosus still maintains its integrity.
The third stage of development of protrusion borders on extrusion, i.e. the formation of a hernia. Therefore, when such a protrusion is detected, the fibrous ring, thinned to the limit, may not withstand the load at any moment and burst. As a result, the nucleus pulposus gradually comes out, i.e., an intervertebral hernia is formed.
But the size of the protrusion is not the only sign by which pathology is classified. Its position relative to the central axis of the spinal canal is of great importance for determining treatment tactics. Therefore, protrusions are distinguished:
- dorsal – the protrusion is directed posteriorly;
- lateral – formed on the right or left side of the spine;
- foraminal - the bulge “leaks” into the foraminal openings of the spine, through which the nerve plexuses pass;
- median - the protrusion is localized clearly in the center of the spinal canal, where there is a large nerve plexus, the so-called cauda equina;
- circular - the fibrous ring becomes thinner over the entire surface area and more or less evenly protrudes into the spinal canal along its entire width.
Types of circular protrusions
Circular protrusion comes in several types, depending on the degree of pulp protrusion and localization.
Annular protrusion
Also called uniform or circular. There is an even bulging of the disc core along the entire circumference, with an equal distance between the protruding parts of no more than 1 mm.
Circular protrusion of the intervertebral disc is detected in approximately 50% of all patients with circular protrusion. Localization is most often in the lumbosacral area of the spine. A bulging disc leads to stenosis of the spinal canal and pinches nerve endings.
With conservative treatment, the effect is almost always positive. Degenerative processes can be stopped with drug therapy, massage, exercise therapy, and physiotherapy.
Circular-foraminal
In this case, the nucleus pulposus of the disc also protrudes in a circle, but most of it protrudes into the foramen - this is the place where the bundles of nerve roots of the spinal cord exit.
Circular foraminal protrusion can be:
- left-handed;
- anterolateral;
- posterolateral.
The pathology causes severe pain - constant or episodic, decreased sensitivity in the legs.
Dorsal circular
With this type of protrusion, the pulp protrudes in a circle and moves into the dorsal space of the disc, that is, directed towards the spinal cord. If the protrusion is large, compression of the spinal tissue occurs. Neurological symptoms occur, intense pain that intensifies with movement and radiates to the legs, hips, buttocks and groin. With dorsal-circular protrusion, drug therapy is required. In case of complicated course, surgery is indicated.
Causes
The main cause of the development of protrusion of intervertebral discs is osteochondrosis. The development of the disease is promoted by:
- maintaining a sedentary lifestyle, sedentary work (office employees, drivers, etc.);
- excessive stress on the spine caused by heavy physical work or playing certain sports;
- metabolic disorders;
- genetic predisposition;
- poor development of the muscle corset that supports the spine;
- curvature of the ridge (scoliotic deformity, kyphosis, lordosis);
- back injuries;
- excess weight;
- unbalanced diet;
- age-related changes.
Is it possible to do massage with disc protrusion?
Until recently, doctors had differing opinions about whether it is possible to do massage for protrusions. Some experts argued that manual therapy would help set vertebrae damaged by a hernia back into place, while others believed that such an effect would only worsen the clinical picture.
In fact, not a single massage, even if performed by the most experienced doctor, can correct the changes that have occurred in the intervertebral disc. However, this does not at all indicate the futility of the procedure.
The movements of the physiotherapist stimulate blood circulation in the lumbar region, which promotes accelerated transport of beneficial microelements to the damaged area, thereby ensuring active recovery of the patient.
Symptoms
The main manifestation of pathological changes in the intervertebral discs is pain. Pain even at the early, so-called pre-hernia stage can be quite severe and protracted. They are often poorly controlled with painkillers. In this case, the biomechanics of the lumbar spine often deteriorates significantly.
The thing is that all people have different disc sizes, and the spinal roots pass at different distances from them. Therefore, in some patients, the pathology does not make itself felt for quite a long time, until the protrusion reaches enormous sizes, while in others, neurological symptoms and pain occur almost immediately and are acute.
Therefore, the size of the hernia or protrusion does not play a significant role in the need for surgery. Neurosurgeons are primarily guided by the patient’s condition, and therefore, in some cases, surgical intervention is indicated for protrusions and the presence of a congenitally narrow spinal canal.
In most cases, pain appears when the protrusion reaches stage 3 of development and its size exceeds 3 mm.
The occurrence of pain, especially acute pain, is a clear sign of compression of the spinal nerves. Often the pain is aching and dull, but it can also be burning or have the appearance of a lumbago. They can radiate to one or both legs, most often to the thigh and lower leg.
Lower back pain occurs when:
- changing body position;
- physical activity;
- staying in one static position for a long time.
Also, protrusion of the lumbar spine can cause:
- reduction in the possible range of motion in the lower back (most often it is difficult for patients to bend over and turn the body due to sudden or intensifying pain);
- disturbances of sensitivity (parasthesia), which is manifested by the appearance of tingling, numbness or a feeling of crawling on the skin in the lumbar region, perineum or legs;
- decreased muscle tone in the legs and reflex spasms of the back muscles in the projection of the affected area of the spine;
- dysfunction of the pelvic organs occurs with a congenitally narrow spinal canal and compression of the nerves of the cauda equina, since they are responsible for control of urination, defecation, and the functioning of the genital organs;
- rapid fatigue, decreased performance.
The severity of pain and neurological symptoms is determined by the location of the protrusion, its size, the degree of inflammation and the amount of nerve compression.
Such symptoms are often a reason for detailed consideration of the need for surgical intervention. Prolonged delay can provoke irreversible changes and lead to paralysis.
Possible consequences and contraindications
As mentioned above, the most likely consequence of protrusion in the absence of treatment is rupture of the fibrous ring and the formation of a hernia, which will require surgery to get rid of. But pathology can also lead to significant limitation of back mobility, curvature of the spinal column and such ailments as kyphosis or lordosis. In addition, the disease can become an obstacle to military service.
To reduce the likelihood of complications, during treatment you should avoid:
- carrying heavy objects;
- wearing uncomfortable shoes (women should prefer flat soles rather than heels);
- serious physical activity;
- cigarettes and alcoholic drinks;
- visits to the bathhouse or sauna, as well as warming up the back;
- activities associated with prolonged stay in a static position.
Diagnostics
At the first visit to the doctor, the patient is examined, during which his neurological status is assessed. A qualified specialist may immediately suspect the presence of protrusion, although not make an accurate diagnosis. Since a fairly large number of spinal diseases are accompanied by the development of neurological symptoms, it is possible to accurately determine the cause of its occurrence only through instrumental diagnostics.
Therefore, the patient is referred to:
- X-ray;
- MRI;
- CT.
A thorough medical history must be taken and neurological tests performed. This allows you to evaluate:
- the nature, strength and time of occurrence, as well as the frequency of pain attacks;
- muscle strength, quality of coordination of movements and find a connection between episodes of increased pain and certain movements;
- the level of physical activity of the patient before the onset of the disease and at the present time;
- posture and determine the possible range of movement in different directions;
- quality of reflexes and tactile sensitivity;
- the condition of the vertebrae, the size of the intervertebral space and identify their displacement or the formation of osteophytes.
MRI provides the most complete information about the condition of intervertebral discs. Using this research method, it is possible to detect the smallest protrusions, even if their size does not reach 2 mm.
Sometimes patients are additionally prescribed radiography with functional tests. This test is designed to determine the presence of instability in the spine. This is an important diagnostic parameter when detecting vertebral displacement, which is often observed in people of any age and creates significant preconditions for the occurrence of compression radicular syndromes and a number of other spinal diseases.
Diet
Proper and rational nutrition is important for everyone at any time in life, but if you have pathologies of the spine, you should especially pay attention to your diet. Diet for protrusion of the lumbar spine:
- Ensures the supply of nutrients to the intervertebral discs.
- Normalizes water balance.
- Will complement therapy.
During the period of exacerbation and treatment of protrusion, the following should be removed from the diet:
- Offal.
- Smoked meats.
- Meat and dishes made from it.
- Flour products.
- Sugar and products containing it.
The menu should include foods with a large amount of nutrients, minerals and vitamins:
- Fresh vegetables and fruits.
- Whole grains.
- Dairy products.
- Freshly squeezed juices from fruits and vegetables.
If you are a vegetarian, then during treatment and to restore the health of your spine you will have to forget about this type of diet. Important proteins for the normal functioning of cartilage tissue are found in animal fats. The necessary elements for the restoration of bone structures are calcium and phosphorus.
It is necessary to get rid of bad habits and drink less caffeinated drinks.
Spinal protrusion is not a fatal pathology and can even be corrected quite well if you visit a specialist in a timely manner and follow all his instructions. In addition to medications and physiotherapeutic procedures, do not forget about physical activity. The doctor will help you choose an effective set of exercises that will be an excellent addition to the main treatment.
We advise you to study - Gymnastics for the back for lower back pain
Treatment of protrusion of the lumbar spine
Initially, for protrusions of lumbar intervertebral discs, conservative therapy is prescribed. In some cases, it helps to effectively combat exacerbations of the disease and is designed to:
- eliminate pain and inflammation, which has a beneficial effect on the condition of the spinal roots;
- improve the quality of blood circulation, which has a positive effect on metabolic processes and trophism of intervertebral discs;
- stop the progression of destruction of the fibrous ring and prevent the transition of the protrusion into a hernia;
- normalize the mobility of the pathologically altered segment of the spine;
- prevent weakening of the back and leg muscles.
However, conservative therapy does not always completely stop degenerative processes. Therefore, very often, despite all efforts, protrusion of the lumbar intervertebral disc can still transform into a hernia over time.
Conservative therapy can lead to complete recovery and normalization of the structure and shape of the lumbar intervertebral disc, especially if it was started at the 1st stage of protrusion formation, when its size does not exceed 2 mm.
In order for conservative treatment to be effective and achieve the maximum objectives, it must be comprehensive and fully take into account all the features of the course of the disease, age, gender, the nature of the patient’s work activity and many other factors. Therefore, only a highly qualified vertebrologist can select the optimal treatment tactics.
As a rule, patients with diagnosed protrusions of the lumbar spine are prescribed:
- drug therapy;
- physiotherapy;
- exercise therapy;
- manual therapy;
- diet and gentle regimen.
Methods of physiotherapy, exercise therapy and manual therapy can only be used outside the acute period of the disease.
Drug therapy
The effectiveness of the treatment largely depends on the correct selection of medications. Depending on the condition of the intervertebral discs, patients are prescribed:
- NSAIDs – eliminate pain and inflammation, are used in the form of oral preparations, injections, ointments, creams or gels;
- corticosteroids – have a pronounced anti-inflammatory effect and are used in acute, serious inflammatory processes;
- chondroprotectors - designed to improve the quality of regeneration of cartilage tissue, improve the flow of metabolic processes in it;
- B vitamins – normalize nerve conduction;
- calcium supplements – increase bone density.
For each patient, the list of medications is selected individually. All medications must be taken in courses, sometimes very long, without allowing unnecessary breaks.
Physiotherapy
Physiotherapeutic procedures help improve the patient’s well-being and inhibit the progression of pathological changes in the tissues of the intervertebral disc. All procedures and their combinations are selected individually and prescribed in courses of 10–15 sessions.
The most effective treatment for protrusions of the intervertebral discs of the lumbar spine are:
- traction therapy – involves traction of the spine using a special device, which helps to increase the intervertebral spaces and eliminate increased pressure on the discs;
- electrophoresis – ensures effective delivery of drugs directly to the lesion, which gives a pronounced analgesic and anti-inflammatory effect;
- shock wave treatment – used in the presence of spinal deformities, helps reduce pressure on nerve fibers and increase muscle tone;
- laser therapy – stimulates metabolic processes, which ensures more active saturation of disc tissue with oxygen and nutrients, helps strengthen the immune system and reduce the severity of pain;
- Magnetic therapy – aimed at improving the functioning of the circulatory system, which ensures increased nutrition of the intervertebral discs and strengthens the body’s own defenses;
- relaxation at balneological resorts - has a positive effect on the entire body and psycho-emotional state, and is used as a preventive measure.
The most effective use of physical methods of influencing the body for protrusions of mild and moderate severity in the absence of pronounced neurological symptoms.
Exercise therapy
Therapeutic exercise is one of the most important components of conservative therapy. For each patient, an individual training program is drawn up by a specialist, taking into account his condition, level of physical fitness and the presence of other diseases.
Exercise therapy involves daily performance of a specially designed set of exercises that help:
- reduce the load on the pathologically changed area;
- increase muscle flexibility and strength;
- have a tonic effect on the body;
- activate blood circulation in the problem area and improve the course of metabolic processes;
- normalize the size of the intervertebral space and create the prerequisites for the release of nerve roots.
The effectiveness of physical therapy has been clinically proven. The method allows you to keep lumbar protrusion under control and prevent its progression. But for this, the set of exercises and load must be selected strictly individually by a specialist. Otherwise, if you choose exercises without permission, the exercises will not bring good results or may even lead to a worsening of the patient’s condition.
All exercises are performed slowly, without sudden movements. The load is increased gradually and only with the permission of the attending physician.
The first exercise therapy sessions should be carried out under the supervision of a specialist. If pain occurs while performing any exercise, you should immediately stop the activity and consult a doctor to find out the causes of the pain syndrome and correct the physical therapy program.
Manual therapy
Manual therapy and therapeutic massage are aimed at restoring the normal anatomy of the spine, improving lymphatic drainage, blood circulation and activating metabolic processes. The use of manual therapy techniques restores muscle tone, improves the quality of reflexes and normalizes tactile sensitivity by reducing pathological pressure on the nerve roots. But for certain types of protrusions, massage is completely contraindicated.
Diet and gentle regimen
When diagnosing protrusion of the intervertebral disc of the lumbar spine, much attention is paid to the characteristics of the patient’s physical activity. It is important not only to avoid excessive stress on the lower back, but also low mobility. Therefore, patients are advised to give up heavy physical labor, especially those associated with lifting weights, and also regularly take walks, not forgetting about exercise therapy.
The effectiveness of conservative treatment also largely depends on the quality of nutrition. After all, it is with food that a person receives the bulk of the substances necessary for the proper functioning of biochemical transformations in the body.
Therefore, it is worth enriching your diet with foods that are sources of calcium:
- fish;
- fermented milk products;
- veal;
- poultry meat;
- vegetables;
- herbs (parsley, dill, basil are especially useful);
- nuts.
It is also worth including dishes containing natural gelatin in the menu. These are meat broths, seaweed, marmalade, etc. It is important to limit the consumption of alcohol, fried, fatty and spicy foods.
If you are overweight, it is recommended to take measures to reduce it, since this leads to an increase in the load on the spine and negatively affects the condition of other organs.
It is recommended to eat 5-6 times a day in small portions. This will allow you to achieve the optimal combination of products, receive all the substances necessary for the proper functioning of the body and not overeat, which will have a positive effect on your weight and overall well-being.
How to relieve pain during protrusion
If you had to think about whether the limbs hurt during spinal protrusion, and also how the pain syndrome can be relieved, you should understand that the condition requires immediate treatment. It is not enough to remove the pain and postpone the visit to the doctor. However, to alleviate the condition until you find time to visit the clinic, you can use the following methods:
- taking medications - analgesics from Paracetamol to Ketanov help;
- local medications - pain-relieving ointments such as Diclofenac or Fastum Gel will be effective in this case;
- orthopedic patches - for example, Voltaren;
- acupuncture, laser therapy or massages;
- gymnastics and exercise therapy aimed at relaxing the back muscles and eliminating pain in the affected area.
If your case is severe, with protrusions causing severe back and abdominal pain, a neurologist can prescribe novocaine and lidocaine blockades, which are a temporary measure to alleviate the patient’s condition.
Surgery
In approximately 5–10% of patients with lumbar protrusions, surgical intervention is indicated. It is recommended for:
- no positive changes in the patient’s condition after 3–6 weeks;
- frequent attacks of severe pain;
- disruption of the functioning of the nerves of the cauda equina;
- chronic reflex and radicular syndrome;
- rapidly increasing deterioration of the condition.
- Congenitally narrow spinal canal
Today, preference is given to minimally invasive methods of percutaneous surgery (puncture nucleoplasty), which allows one to achieve excellent results with minimal trauma to soft tissues. The procedure is aimed at reducing the pressure inside the altered intervertebral disc of the lumbar spine, which creates the preconditions for restoring its normal shape and boundaries. This is achieved by influencing the nucleus pulposus:
- cold plasma;
- laser;
- radio wave electromagnetic radiation;
- hydroplastics
All methods work on approximately the same principle. The essence of puncture hydroplasty is the introduction, under the control of an image intensifier, into the pathologically altered disk of the nucleus pulposus from a posterior approach. The skin is pre-treated with an antiseptic solution.
Once the needle reaches the center of the nucleus, a working port is inserted into it, through which the nucleotome is inserted. Observing his actions through the monitor, the neurosurgeon turns on the device generator and begins to perform reciprocating movements in different planes, without going beyond the nucleus pulposus of the disc.
This leads to the removal of nuclear tissue at the site of passage of the nucleotome, which reduces its size, eliminates pathological pressure on the fibrous ring and promotes retraction of the protrusion.
The operation is performed under local anesthesia and does not require a hospital stay. It is performed on an empty stomach and takes on average no more than half an hour. After nucleoplasty, a puncture of no more than 2–5 mm in size remains on the skin, so it does not require sutures and heals independently, without leaving noticeable marks on the skin. The wound is covered with a sterile bandage.
The use of nucleoplasty is not recommended for patients over 50–55 years of age, since intervertebral discs at this age are already significantly dehydrated and lose the ability to invert retraction.
Hydroplasty, which, unlike cold plasma, laser or radio wave nucleoplasty, is based on the destruction of part of the nucleus pulposus by the pressure of a physiological solution. The operation is also performed through a puncture of soft tissue. The solution is fed through a conductive needle, which additionally has a branch for aspiration of waste material. The effect of hydroplasty is similar to the results of nucleoplasty and also consists in the reverse retraction of the protrusion.
But if an MRI has already detected a rupture of the fibrous ring of the disc, i.e. the formation of a true hernia, nucleoplasty loses its relevance. In such cases, it is usually necessary to resort to microdiscectomy, endoscopic surgery, and others.
General description of the disease and its pathogenesis
Protrusion is a consequence of the presence of pre-existing degenerative processes developing in the spinal column. With this pathology, the fibrous ring located inside the intervertebral disc is seriously damaged. It does not yet have signs of disruption in the shell with bulging into the external space, as happens with a hernia, but is quite stretched and deformed, which is recorded in osteochondrosis. Such an anomaly of the thoracic spinal column is its complication.
A disorder develops due to a lack of fluid and mineral components required to restore the spinal disc. The fibrous ring begins to deplete, and gradually the problem affects its second layer - the nucleus pulposus. When the lack of collagen fibers and organic components in fibrous tissues reaches a dangerous level, the formation of microcracks begins, the core and outer elastic membrane become thin, swollen, and slight bulging is noted.
Intervertebral disc deformation
Gradually, a large amount of lactic acid accumulates in the tissues, which can ultimately lead to the formation of a hernia. At the same time, the damaged area becomes less mobile, due to the decreased intervertebral disc, the bones rub against each other, and severe pain is noted.
With protrusion, pain can spread throughout the entire spinal column.
Impact of massage
Massage is not only a simple “muscle kneading”, but a whole complex of activities that activate the neuroendocrine system and normalize muscle tone, both when it weakens and when it increases. Three main therapeutic factors can be distinguished: neuro-reflex, humoral, and mechanical effects. What are these factors? Here is their brief assessment:
- The neuro-reflex factor arises as a result of the rhythmic mechanical influence produced by the hands of a specialist. Various movements, changes in pressure, and tempo lead to periodic activation of large receptor fields of afferent (sensitive) impulses in the brain. The activation of the autonomic nervous system is connected, associated with the need to change blood flow in the area of influence. In the cerebral cortex, at the correct, calm pace of work, a focus of diffuse inhibition is formed, so after the procedure the person is in a state of pleasant relaxation. He wants to sleep or take a nap.
After processing the impulse, they are transformed into motor signals to muscles, blood vessels, soft tissues, and internal organs. The muscles restore impaired tone, the blood volume is redistributed in the vessels, the inflammatory edema associated with the occurrence of protrusion, as well as hernia, is eliminated;
- The humoral factor is associated with the release of special biologically active substances into the blood. These are norepinephrine, acetylcholine, histamine, bradykinin. These substances, being universal, can both help restore the body’s immune status and also have a negative effect under special conditions. Blood flow to the skin after a session, redness, a feeling of warmth - this is certainly a positive effect.
In the case of an acute allergic reaction, an excess of the same histamine causes severe skin itching, hives, and Quincke's edema. This is an example of how one substance can have positive and negative effects on the body;
- mechanical factor. The physical work of a massage therapist on the skin and subcutaneous tissue leads to improved blood circulation in the outer layers of soft tissues, and their resistance to the influence of hands increases. In the case of conduction sensitivity disorders, improved blood circulation sometimes makes it possible to restore tactile and pain sensitivity.
Back after massage.
The skin is cleansed, swelling in the subcutaneous tissue of the lower back is eliminated, and the excess heat provided by the movements and hands of the massage therapist promotes blood flow to the skin, its outflow from the deep muscles of the back, as well as the zone of inflammation that appears under the influence of protrusion and hernia.
Muscles respond with great gratitude to a properly performed massage. Their tone is normalized, blood supply and venous outflow are improved. Lactic acid begins to be released from the deep back muscles, which are irritated by protrusion, hernia and osteophytes. This improves muscle contractility, lymphatic drainage from them, and muscle regeneration increases.
In the case of a long history of the disease and the involvement of muscles in the secondary inflammatory process, proper massage can even lead to the release of muscles from cicatricial adhesions and increase their strength in case of flaccid or peripheral paralysis and paresis. It is these types of movement disorders that occur with protrusions, and even more so with herniated intervertebral discs.
Despite the fact that the intervertebral joints in each individual case are relatively inactive due to their small amplitude, the impact of the hands improves articular circulation and leads to strengthening of the ligamentous apparatus of the spine. Accordingly, the venous outflow from the deep fascia of the back and longitudinal ligaments, which are rich in nerve endings and cause severe pain with discogenic complications of osteochondrosis, improves.
Healthy and osteochondrosis-affected spine on CT scan.
We must not forget about the formation of new conditioned reflex connections that are caused by regularly repeated sessions. For example, a competent specialist can use vibration and tapping techniques in the lumbosacral region to enhance intestinal motility and additionally help the patient in the fight against atonic constipation.
Massage of the lumbosacral area can be of great help in improving blood circulation in the pelvic organs, as well as in the lower extremities. Massage of this area, in addition to eliminating pain from protrusions and hernias, can be indicated for patients with an inactive stage of CNM - varicose veins. It helps women and men with chronic congestion in the pelvis, for example, in the presence of benign prostatic hyperplasia (prostate adenoma).
There are other zones rich in vegetative fibers that can be considered reflexogenic. For example, when massaging the protruding 7th cervical vertebra, the reflex effect on the heart is activated, and the effect on the area of the 5th thoracic vertebra improves blood flow to the stomach.