Intervertebral disc protrusion is a degenerative disease resulting from prolonged exposure to negative factors. At the same time, the shape and structure of the intervertebral formation changes, which affects the surrounding soft tissues. It is important to start therapy as soon as possible, since the process is reversible. However, with further development of the pathology, extrusion of the vertebral fragment is formed - the fibrous ring ruptures, and the nucleus pulposus begins to compress the blood vessels and nerve endings. In this case, treatment requires much more time and involves several courses of treatment procedures.
Symptoms of Spinal Extrusion
Often the pathology is asymptomatic, clinical manifestations are caused by the involvement of nerve endings.
Extrusion of discs of the lumbar spine is accompanied by:
- low back pain radiating to the lower limb, often sciatica occurs as a reaction to physical activity
- dependence of unpleasant sensations in the back on the position of the body in space - in a lying position the pain decreases, when bending over it intensifies
- weakening of muscle strength in the legs
- paresthesias
When the V lumbar and I sacral roots are involved, pain occurs below the knee, in the foot and fingers. Discomfort along the anterior and outer surface of the thighs is typical for damage to the fourth nerve trunk.
Extrusion of the intervertebral disc in the thoracic region can be disguised as somatic diseases of internal organs - angina pectoris, gastritis, intestinal dyskinesia, peptic ulcer, etc.
A protrusion in the cervical segment of the spine is manifested by pain in the neck, dizziness, numbness in the back of the head, and weakening of the arm muscles.
Why and how do intervertebral hernias form?
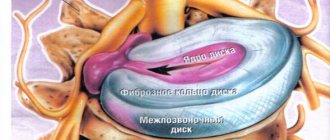
Intervertebral discs are fibrocartilaginous formations that are located between the bodies of adjacent vertebrae. Each disc consists of a central part, the nucleus pulposus, and a surrounding annulus fibrosus. The main function of the discs is a spring one: they spring during walking, changing body position, when jumping, and absorb any impacts, the force of which is directed along the spinal column.
The main causes of intervertebral hernias:
- spinal column injuries;
- long-term intense physical activity;
- sedentary lifestyle, constant work in a monotonous uncomfortable position;
- osteochondrosis;
- sports injuries, sudden strong movements;
- excess body weight (in this case, the spinal column experiences constant stress).
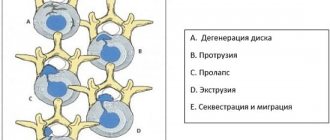
Changes that occur in the disc during intervertebral hernia:
- Stage I. Prolapse is a protrusion no larger than 2-3 mm. The disc still protrudes slightly beyond the vertebral body. But swelling forms in the area of damage, and the first symptoms of the disease may appear.
- Stage II. A protrusion is formed - a protrusion larger than 5 mm in size. Symptoms are more pronounced.
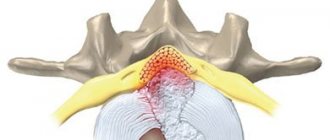
- Stage III. Extrusion is the prolapse of the core of the intervertebral disc outside the vertebra (dangling in the form of a drop). As a result of the inflammatory process, osteophytes—bone protrusions—begin to grow on the vertebrae. The nerve roots are compressed and blood circulation is disrupted.
- Stage IV. Due to inflammation, poor circulation and compression of nerve roots, atrophy processes begin in the tissues. The intervertebral disc also atrophies, shrinks, ceases to perform its functions, two adjacent vertebrae practically grow together.
The spine includes seven cervical vertebrae, which are designated by the letter C with the vertebra number - C1-C7, respectively, twelve thoracic - Th1-Th12 and five lumbar - L1-L5. Below are the five sacral vertebrae, which in an adult fuse into one bone, the sacrum. Most often, hernias form in the most mobile parts of the spine: the cervical and lumbar. In the thoracic region they are much less common, since the pectorals take part in the formation of the chest and are more rigidly fixed.
The hernial protrusion can be located in front, behind or to the side of the vertebral body. The symptoms of the disease depend on this.
Stages of development
The degenerative process begins with the nucleus pulposus, which is normally represented by a gelatinous mass with high viscosity and elasticity. Constant metabolism is ensured by chondrocytes: the structures synthesize and break down proteoglycans for the matrix of the nucleus pulposus, which retains water and collagen in the annulus fibrosus. A healthy intervertebral disc maintains a certain level of pressure.
Abnormal mechanical axial stress due to the combined effects of unfavorable heredity, age, inadequate transport of metabolites and trauma worsens the condition of chondrocytes and triggers degeneration of the nucleus pulposus. This structure loses moisture. Dehydration leads to a decrease in intradiscal pressure with the transfer of mechanical load to the fibrous ring, in which microcracks appear, progressing to rupture. Through the gap, as the load on the spinal column increases, part of the intervertebral disc prolapses; during extrusion, a fragment larger than the base falls out.
Treatment
Based on the collected medical history and additional examination data, a therapeutic program is prescribed taking into account the anatomical characteristics of the patient.
The specialists of the Doctor Pozvonkov Center for Progressive Medicine adhere to the principles of non-invasive physiological restoration of health with minimal drug influence.
One of the most effective techniques is underwater spinal traction, aimed at increasing the intervertebral space and strengthening the muscle frame.
Thanks to a course of sessions, it is possible to relieve pain, eliminate inflammation and restore the correct position of the structures of the musculoskeletal system.
Book your first appointment now! Restore your body's own strength and restore your back health in our Center!
How to diagnose
The main diagnostic methods that can confirm extrusion of intervertebral discs are magnetic resonance imaging and computer scanning. An MRI will show the exact cause of back pain: lumbar radiculopathy can accompany not only intervertebral hernias, but also foraminal (lateral) lumbar stenosis against the background of compression of the sciatic nerve by a cyst, tumor, etc. CT better demonstrates damage to bone tissue.
Early in-depth diagnosis is necessary if neurological disorders increase, persistent pain syndrome occurs, or if treatment of intervertebral disc extrusion involves epidural administration of drugs.
Diagnosis of intervertebral hernias
- Lumbar disc herniation
- Cervical disc herniation
- Diffuse disc herniation
- Dorsal disc herniation
- Median disc herniation
- Paramedian disc herniation
- Sequestered disc herniation
- Foraminal disc herniation
- Circular disc herniation
The multidisciplinary CELT clinic has the best diagnostic equipment from European and American manufacturers, which allows you to quickly and reliably establish a diagnosis of intervertebral hernia, accurately determine the degree of protrusion and its location.
The main methods for diagnosing the disease are computed tomography () and magnetic resonance imaging (MRI). Modern devices allow you to recreate a three-dimensional model of the intervertebral disc and examine the hernial protrusion and surrounding tissues in detail. If necessary, it is recommended to conduct electroneurography - a study that allows you to evaluate the passage of nerve impulses along nerve fibers.
Traction treatment of intervertebral disc herniation
Traction traction will reduce the pressure of the hernia on the root, thereby allowing:
- relieve muscle tension
- numb
- restore root microcirculation
.Various modes are complemented by heating and manual techniques. Roller massage, performed simultaneously with spinal traction, allows you to relax the muscles, remove functional blocks that arise in them that prevent stretching, and improves blood flow. Heat and vibration create a feeling of comfort and further relax the muscles.
Dorsal spinal disc extrusions
Dorsal extrusion is a violation of the integrity of the fibrous ring of the intervertebral disc located in the posterior projection. It is directed outward and does not exert pressure on the dural membrane of the spinal canal. In order to understand what dorsal disc extrusion is, you need to imagine the structure of the spine. It consists of individual vertebral bodies, which have arches that form the spinal oval canal. Between them there are cartilage pads. They have the same shape as the vertebral body along with the arches. Inside the disc there is a similar oval hole that protects the spinal canal from excess pressure from the vertebral bodies and surrounding paravertebral soft tissues. The structure is connected to each other using longitudinal ligaments. They are divided into short ones, which connect two adjacent vertebrae, and long ones, which start near the back of the head and end in the coccyx area.
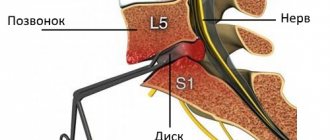
Dorsal extrusions of herniated discs are located in the posterior part, which is formed by the vertebral arches. Most often, dorsal spinal extrusion occurs in the lumbar region. This is anatomically determined, since it is in this section of the spinal column that the maximum amplitude of mobility in the frontal plane occurs. When you sharply bend forward or lift your torso with a heavy weight in your hands, extreme stress is placed on the lumbar discs. This is how the dorsal extrusion of L5-S1 is most often formed, which falls on the conditional center of gravity of the human body. Hernias often form at this point. They give a pronounced neurological clinical picture, up to complete numbness of the legs and loss of their mobility.
Dorsal extrusion of the L5-S1 disc is a dangerous condition; the patient requires immediate professional help from a neurologist or vertebrologist. With proper treatment, it is possible to achieve complete restoration of the integrity and elasticity of the damaged fibrous ring and thereby prevent the risk of developing an intervertebral hernia.
FAQ
Do treatment methods depend on the location of the hernia?
Effective treatment of a hernia depends mainly on the stage of the pathology, as well as the consequences or complications. Any type of hernial protrusion: hernia of the lower back, cervical or thoracic region, requires conservative treatment or surgical intervention. Hernial formation of any part of the spine responds positively to traditional drug therapy, gymnastics, and massages.
What are drug blockades?
Spinal block is a method that allows you to quickly and effectively relieve pain at its localization. The effect lasts about a month and accelerates the healing process. Allows you to return to your normal lifestyle and comfortably engage in therapeutic exercises.
The blockade consists of local administration of multicomponent painkillers. It is not a treatment, but serves only to relieve acute pain during conservative therapy. The procedure is carried out by a specialist - a neurologist or surgeon in a medical facility.
What is spinal traction?
Traction is an effective manipulation indicated for hernial lesions accompanied by compression of the nerve roots. It is carried out in medical clinics using special equipment and is accompanied by pain relief in the acute period. The patient is placed on a flat, hard surface, and then the spine is slowly and safely stretched, eliminating possible pinched nerve endings.
Reasons for the development of disc extrusion
There are various reasons for the development of extrusion of the vertebral discs - they mainly overlap with risk factors for the appearance of degenerative dystrophic changes. In general, extrusion is a consequence of advanced and untreated osteochondrosis. Therefore, the reasons that cause complications are the same. They include:
- maintaining a sedentary lifestyle with predominantly sedentary work;
- excess body weight, creating additional physical and shock-absorbing load on the spinal column;
- poor posture and curvature of the spinal column;
- incorrect positioning of the foot in the form of flat feet and club feet;
- deforming osteoarthritis of large joints of the lower extremities;
- spondyloarthrosis, ankylosing spondylitis, systemic lupus erythematosus and other pathologies of cartilage tissue of the spinal column;
- insufficient consumption of clean water during the day leads to dehydration and disruption of the diffuse nutrition of the cartilage tissue of the intervertebral discs;
- hard physical labor;
- suffered severe infections;
- spinal cord tumors;
- spinal tuberculosis.
In women, extrusion of the lumbar spine may appear during pregnancy or after its termination. This is due to the fact that while expecting a child, the body undergoes powerful hormonal changes. The cartilage tissue softens, posture is disrupted, the internal organs of the abdominal cavity are dislocated, blood flow changes, etc. Very often, if the rules of hygiene for pregnant women are violated, women develop numerous diseases of the musculoskeletal system. The most common of these is symphysitis, or separation of the pelvic bones. So, this condition is always accompanied by pronounced extrusion of the intervertebral discs of the lumbosacral spine. These negative consequences can be avoided by wearing a bandage and actively preparing for childbirth. To do this, you can use manual therapy methods, massage and physical therapy.
Extrusion of cervical discs
Extrusion of the cervical spine mainly develops in those patients who, during the working day, are forced to hold the muscles of the neck and collar area in prolonged static tension. Therefore, some neurologists classify extrusion of cervical discs as an occupational disease of office workers, accountants, seamstresses, tailors, cutters, programmers, translators, etc.
Cervical spine extrusion may present as tenderness in the neck. A person may also be bothered by occipital headaches, dizziness, absent-mindedness, drowsiness, decreased concentration and memory. With prolonged development of disc extrusion in the cervical spine, arterial hypertension, vegetative-vascular dystonia, vertebrobasilar vascular insufficiency and other unpleasant complications can develop.
Extrusion of C5-C6 causes motor and sensory disturbances in the upper extremities. One of the branches of the radicular nerve extending from the spinal cord in this intervertebral space is involved in the formation of the brachial nerve plexus. Therefore, when an inflammatory process occurs, pain in the arm on the affected side begins to appear, a sensation of crawling goosebumps, a decrease in muscle strength and skin sensitivity.
Rehabilitation
After any operation, the rehabilitation period begins. But after nucleoplasty or hydroplasty, there are practically no restrictions and pain. After endoscopic surgery, you need to stay in the hospital for about 5 days, after microdiscectomy - 7-10 days and stay in bed for 24 hours without getting up. Naturally, after more traumatic surgical interventions, postoperative pain is present and a long period is required for complete recovery.
Thus, depending on the type of operation performed, patients may be prescribed for different periods of time:
- drug treatment;
- exercise therapy;
- wearing a corset;
- kinesitherapy;
- massotherapy;
- physiotherapy.
Even after successful completion of the operation for intervertebral hernia and the rehabilitation period, it is necessary to adhere to a gentle regimen and avoid strong physical exertion, but physical inactivity is also dangerous. Therefore, it is worth doing physical therapy every day, taking breaks to warm up during sedentary work, and swimming regularly.
Pain in the lower back (lumbar region) is one of the most common causes of disability and seeking medical help [1]. In the structure of the causes of pain in the lumbar region, the leading role is given to musculoskeletal (nonspecific) sources (90-95%) [2]. Discogenic radiculopathy occurs in clinical practice much less frequently (less than 5%) [3], however, patients with radicular syndrome have more intense pain, severe disability and decreased quality of life. In this regard, the volume of therapeutic and diagnostic measures increases, and direct and indirect costs increase [4-6]. For discogenic radiculopathy, both surgical and conservative treatment methods are used, and most patients have a positive effect from conservative therapy [2, 7]. Surgical treatment allows for quicker relief of pain and associated temporary disability, but patients’ condition gradually improves even with conservative management, and after a year of follow-up, the differences between approaches are erased [8, 9]. Improvement in the condition of patients with conservative treatment is often accompanied by natural regression of the disc herniation, which is confirmed by high-quality neuroimaging methods. Over the past 10 years, a number of cases of spontaneous regression of disc herniations have been published in the literature [10–19]. We present a clinical case of regression of a large disc herniation in the lumbar spine against the background of conservative treatment, which we observed at the Clinic of Nervous Diseases named after A.Ya. Kozhevnikova.
The patient, 38 years old, complained of intense pain in the lower back and left gluteal region, radiating along the posterolateral surface of the thigh and lower leg to the fourth and fifth toes of the left foot, a feeling of numbness and tingling in the area where the pain radiated. The patient began to experience episodic pain in the lumbar region about 6 years ago. Exacerbations were observed periodically (up to 3-4 times a year), which could be successfully stopped by taking non-steroidal anti-inflammatory drugs (NSAIDs). It should be noted that the patient’s work involves long periods of sitting at a computer. According to the patient, the real deterioration is caused by lifting heavy objects in an uncomfortable position. In contrast to previous episodes, greater intensity of pain was observed, irradiation into the leg and development of numbness along the posterolateral surface of the leg to the IV-V toes of the left foot. Taking NSAIDs did not bring any significant effect. The pain intensified significantly with movements in the lumbar spine. Due to persistent intense pain and the ineffectiveness of drug therapy, the patient turned to the Clinic for Nervous Diseases named after. AND I. Kozhevnikova.
Upon admission to the clinic, the intensity of pain in the back was up to 8 points on the digital rating scale (DRS), in the leg - up to 6 points, with a pronounced neuropathic component (4 points on the DN4 questionnaire). Severe disability was noted (Oswestry index 68%). Indicators of emotional status corresponded to the norm (according to the Hospital Anxiety and Depression Scale, anxiety was 5 points, depression was 0). The decrease in quality of life was due primarily to the physical component of health (on the SF-12 scale - physical component of health - 36.4, psychological - 61.8 points). According to a special questionnaire (Start Back Screening Tool), the risk of chronic pain was assessed as average (overall score 5 points, subscale score 2 points).
The neurological status revealed hypoesthesia and paresthesia (in the form of a tingling sensation) along the posterolateral surface of the thigh and lower leg to the IV-V toes of the left foot, absence of the left Achilles reflex, positive Lasegue symptom on the left - 45 degrees, pain on deep palpation and percussion in the projection of the spinous processes lower lumbar vertebrae. There are no other neurological disorders, muscle strength is sufficient, pelvic functions are not impaired. Taking into account complaints of intense pain in the lower back with irradiation in the leg to the foot, which developed after heavy lifting, and the presence of signs of radiculopathy (positive Lasegue sign, loss of the Achilles reflex, neuropathic pain and hypoesthesia in the dermatome of the first sacral root), a clinical diagnosis was established: vertebrogenic left-sided lumbar ischialgia , radiculopathy of the first sacral root (against the background of a probable disc-radicular conflict).
Blood tests (general and biochemical), urine analysis without pathology.
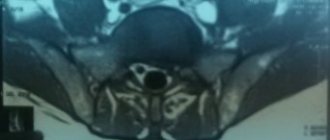
MRI confirmed the discogenic nature of the radiculopathy, revealed paramedian sequestered extrusion of the disc between the fifth lumbar vertebra and the sacrum up to 11 mm with lateralization to the left, in the subchondral parts of the adjacent vertebrae there was an increase in the MR signal in T1 and T2 modes, corresponding to the stage of fatty degeneration (Modic II; see picture,
MRI of the patient's lumbosacral region. Upon admission a-c: paramedian sequestered extrusion of the L5-S1 disc up to 11 mm with lateralization to the left is visualized, in the subchondral parts of the adjacent vertebrae (arrows) an increase in the MR signal was noted in T1 and T2 modes, corresponding to the stage of fatty degeneration (Modic II), and after 9 months; d-f: regression of the L5-S1 disc herniation was noted, with preservation of protrusion up to 3 mm, changes (Modic II). a-c).
Due to the absence of emergency indications for surgery, it was decided to use conservative treatment options. The patient was administered steroids in combination with a local anesthetic via the epidural foraminal approach under radiographic guidance. Additionally, NSAIDs were used to reduce pain. The patient's motor mode was corrected: the limitation of heavy lifting during the period of exacerbation and the technique of safer performance of the movement in the future (from a squatting position with a straight back, and not due to bending) were discussed, the need to take breaks during prolonged static loads, the ergonomics of the workplace was adjusted patient (height of the table, chair, location of the computer monitor), therapeutic exercises were selected.
After treatment for 2 weeks, the pain completely regressed in the leg and significantly decreased in the lower back (up to 4 points according to the CRS). The patient returned to normal daily activities, went to work, and continued her professional activities in full. Over the course of 9 months, there were no repeated exacerbations, but periodically I was bothered by lower back pain (up to 3 points according to the CRS) with awkward movements. Indicators of work ability have improved: the Oswestry index decreased to 14%, which corresponds to a minimal limitation of functional status. Indicators of quality of life are normal (physical component of health - 49.6, psychological - 60.7 points), indicators of anxiety and depression on the hospital scale - 0. In the neurological status, only a decrease in the left Achilles reflex, a subjective feeling of numbness along the lateral edge of the foot are noted . Repeated MRI of the lumbosacral spine revealed regression of disc extrusion between the fifth lumbar vertebra and the sacrum, protrusion of up to 3 mm and Modic II type changes remain (see figure, d-f).
Thus, against the background of complex conservative treatment with the use of epidural steroids, the patient with discogenic radiculopathy achieved significant clinical improvement, which allowed her to quickly restore her ability to work. During follow-up, regression of disc extrusion was demonstrated. It should be noted that the decrease in the severity of symptoms significantly outpaced the changes on MRI.
For the first time, regression of a herniated intervertebral disc, confirmed by computed tomography in a 25-year-old patient, was described by F. Guinto et al. in 1984 [20]. Subsequently, with the introduction into widespread practice of MRI, which is highly accurate in assessing changes in soft tissues, including intervertebral disc structures, more publications of both individual clinical cases and their series appeared [10-14, 16-18]. Cases of regression of large hernias have also been described in our country [15, 19].
Currently, three main mechanisms of regression of disc herniations are considered in the literature [12, 16, 21, 22]. The first proposed option, mechanical “reduction” of the hernia, is predominantly speculative in nature and is hypothetically possible only with a intact fibrous ring, for example, with small protrusions. The second mechanism discussed is dehydration, which results in a decrease in the volume of the hernia. This assumption is based on studies that show a higher likelihood of hernia regression in young patients with an increased T2 signal on MRI (due to high fluid content) [21].
The third hypothesis about an immune-mediated reaction against hernia fragments seems to be the most convincing [23-26]. During development, the intervertebral disc is formed as an immune-privileged organ, without interaction with the immune system, which excludes it from the processes of immunological tolerance. During disc degeneration and its extrusion (formation of a hernia), accompanied by a violation of the integrity of the fibrous ring, the nucleus pulposus comes into contact with the immune system, which perceives it as a foreign body and triggers a complex cascade of biochemical and immunological reactions. The autoimmune reaction is realized by the activation of antibody-producing B-lymphocytes and cytotoxic T-lymphocytes. The production of pro-inflammatory cytokines (tumor necrosis factor - TNF, interleukins - IL-1α, IL-1β, IL-6 and IL-17) increases, which contribute to the degradation of the extracellular matrix and increased expression of chemokines. This leads to the penetration of activated immunocytes into the disc and the production of endothelial growth factor, which promotes neovascularization and ensures increased phagocytosis and resorption of disc herniation fragments. Inflammatory cytokines such as TNF further stimulate the production of metalloproteinases (especially metalloproteinase type 7, which causes collagen dissolution).
The development of inflammatory processes in a disc herniation was confirmed by immunohistochemical study of materials obtained during surgery in patients with lumbar ischialgia: high levels of phospholipase A2, inflammatory interleukins, chemokines, and matrix metalloproteinases of various groups were revealed [27]. In the work of M. Yoshida et al. [28] in an experimental model of disc herniation revealed an increase in the level of TNF and IL-1β already on the 1st day. By the 3rd day, the content of monocyte chemoattractant protein type 1 increased, which contributed to active infiltration by macrophages, which led to regression of the hernia after 12 weeks.
The timing and predictors of regression of disc herniation have not been fully studied. The literature presents extremely variable periods of regression (from 3 to 30 months), however, many studies note that regression is more possible in large hernias with sequestration, which probably provokes a maximum immune response. In 2014, M. Macki et al. [29] presented a review of the literature on spontaneous regression of sequestered disc herniations in the lumbar spine. The average time for regression of hernias according to MRI was 9.27±13.32 months, while regression of clinical symptoms was noted much earlier - on average 1.33±1.34 months from the onset of the disease. The authors explain that symptomatic regression, significantly outpacing hernia regression, is likely consistent with the natural history of discogenic radiculopathy. A study of the dynamics of clinical symptoms showed complete resolution of back pain, a decrease in the severity of paresis to 86%, sensory impairment to 68%, and hyporeflexia to 75%. In the case we present, significant clinical improvement during conservative therapy was noted within 10 days, while sensory disorders regressed to a lesser extent. Radiographic changes were noted at 9 months from the onset of the disease.
The influence of the type of disc herniation on the possibility of its regression was studied in a systematic review by S. Chiu et al. in 2015 [21]. The probability of spontaneous reduction of sequestrations reached 96%, extrusions - 70%, protrusions - 41%. The chances of complete regression for sequesters were 43%, and for extrusions - 15%. The authors concluded that the larger the disc herniation, the greater the immune response it provokes, and therefore the greater the likelihood of its regression. In addition, the following features of the hernia were noted that predispose to its reduction. These include migration of disc fragments into the epidural space, usually associated with rupture of the posterior longitudinal ligament, which is consistent with previous studies [30, 31]. Entry of disc fragments into the epidural space makes them more accessible to the immune system and increases the chances of immune-mediated lysis. Contrast enhancement of the peripheral parts of the hernia indicates their vascularization and the possibility of phagocytosis. According to R. Autio et al. [32], the wider the contrast zone, the greater the likelihood of regression. High signal intensity in T2 mode corresponds to a higher fluid content in the disc herniation and predisposes to the dehydration mechanism of its reduction. The authors also noted that the isolated factor of hernia regression does not always correlate with a better outcome of the disease, and on the contrary, clinical improvement is possible without reducing the hernia; thus, once again emphasizing that the reduction of symptoms is determined not only and not so much by radiological changes.
A. el Barzouhi et al. came to a similar conclusion. [33] when studying the relationship between neuroimaging findings and clinical outcome. A year after the onset of the disease, 84% of patients noted a good result of treatment. At the same time, on MRI, disc herniation was detected in 35% of patients with a good outcome and 33% of patients in the group with unsatisfactory treatment results. In the group of patients without a disc herniation, a satisfactory treatment result was observed in 83%, but in the group with a persistent hernia, satisfactory results were observed in 85%. The authors concluded that MRI scans one year after disease onset do not differentiate between patients with different disease outcomes.
The presented clinical case illustrates the effectiveness of multidisciplinary conservative treatment of discogenic radiculopathy using epidural blocks. The possibility of regression of a large sequestered disc herniation was noted. The decrease in the severity of clinical symptoms significantly outpaced neuroimaging changes, which is likely determined by the peculiarities of the course of immunological and biochemical processes in the area of the disc-radicular conflict. It seems promising to study predictors of clinical outcome and hernia regression in patients with discogenic radiculopathy to optimize their management tactics.
The authors declare no conflict of interest.
Additional points
Its action does not cause a weakening of concentration and sedation, and is not accompanied by a weakening of muscles in general. It is allowed to be prescribed to people for a long time who, for certain reasons, cannot be exposed to such influences. However, the drug should be prescribed only by a doctor or subject to the choice of the drug in agreement with him.
Mydocalm should not be taken by pregnant women and nursing mothers, as well as infants who cannot tolerate lidocaine and suffer from myasthenia gravis.
After taking measures, the pain gradually subsides after a few days. Massage sessions and physiotherapy treatments may be prescribed. The next stage of treatment is to carry out restorative therapeutic exercises. It is not only a method of treatment, but also helps to permanently consolidate the result and prevents the occurrence of relapses and the development of new intervertebral hernias.
Surgery for spinal hernia L5–S1
Surgery for a hernia of the lumbosacral spine is a last resort measure, which is resorted to in strictly defined situations:
- in the absence of positive changes in the patient’s condition after 1–3 months of treatment with conservative methods;
- severe cauda equina syndrome;
- the occurrence of paralysis;
- sequestered hernias.
All operations performed for hernia are minimally invasive and have a high level of safety. Modern neurosurgery offers such ways to solve the problem as:
- nucleoplasty;
- endoscopic surgery;
- microdiscectomy.
The specific surgical tactics for L5–S1 disc herniation are selected based on its size, type, and general health of the patient. If at the stage of preoperative preparation it is assumed that a significant part of the intervertebral disc will be removed, the neurosurgeon will notify the patient of the need to install a special implant to close the resulting defect. Today, a special Barricaid mesh is used for these purposes. It is used to fill the missing part of the annulus fibrosus and prevent the nucleus pulposus from leaking out through the existing defect.
Sometimes the L5–S1 intervertebral hernia reaches such a size that complete removal of the disc is required. In such situations, neurosurgeons may decide to achieve spinal fusion, i.e. fusion of the L5 and S1 vertebrae with each other, but this will lead to limited mobility of the spine, which is not always acceptable for patients.
Another option to solve the problem is to install an M6 endoprosthesis. It is a copy of a natural intervertebral disc, as it has an artificial fibrous ring and nucleus pulposus. Installing an endoprosthesis requires a neurosurgeon to have a thorough knowledge of the technology, but if the doctor has undergone appropriate training, then installing the M6 does not cause any difficulties.
Puncture surgery
Methods of puncture surgery (nucleoplasty) have appeared in the arsenal of neurosurgeons recently, but have already managed to completely revolutionize the idea of operations for intervertebral hernias. They are practically devoid of intraoperative risks, allow you to leave the clinic on the day of surgery, completely free from pain, and avoid the formation of scars.
The essence of nucleoplasty is the introduction, under the control of an image intensifier, of a thin cannula into the nucleus pulposus of the disc through the soft tissue above the affected spinal motion segment. As soon as it reaches the center of the nucleus, an electrode is immersed in it, which creates:
- laser energy (laser nucleoplasty);
- cold plasma (cold plasma);
- radio waves (radio wave).
In the first case, evaporation of part of the nucleus pulposus is carried out using the thermal energy of the laser, but this is associated with the risk of overheating of surrounding tissues, which may include blood vessels and nerves. Therefore, recently preference has been given to other methods of nucleoplasty, especially cold plasma and hydroplasty.
The essence of cold plasma nucleoplasty is the use of cold plasma, which destroys nuclear tissue without causing strong heating. As a result, negative pressure is created in the intervertebral disc, which leads to the retraction of the resulting protrusion back.
Hydroplasty is based on the destruction of the contents of the nucleus by the pressure of a saline solution. It is carried out using a SpineGet device specially created for this procedure. The tip inserted into the body has 2 branches: for injection of liquid supplied under pressure and for suction of waste material. Since the destruction of the nucleus and removal of the resulting particles along with saline solution occurs simultaneously, the neurosurgeon can very accurately control how much of the nucleus pulposus should still be removed.
But puncture therapy methods can only be used for hernias L5–S1, the size of which does not exceed 7 mm.
Endoscopic hernia surgery
Endoscopic operations are indicated for large hernias or their location in narrow areas of the spinal canal. The essence of the method is to create access with a shaver in its projection and insert the endoscope. It is a tube through which special instruments are inserted into the surgical field and the altered tissue is excised. The neurosurgeon controls his every step through a camera inserted into the treatment area using a similar technique.
Endoscopic surgery for intervertebral hernia has a low percentage of intraoperative complications and a short recovery period. But it also cannot be performed in all cases.
Microdiscectomy
One of the classic techniques for removing hernias is microdiscectomy. It involves removal of a protrusion or the entire disc in an open manner through an incision of up to 3 cm. The method is indicated for severe neurological complications, the impossibility of using other techniques, and this operation is also indicated for sequestered hernias L5–S1.
Prevention of extrusion formation
- The basis for preventing spinal problems is correct posture. Maintaining a healthy back should be cultivated from early childhood to avoid the formation of scoliosis and kyphosis.
- Proper lifting of weights.
- Body weight control - it’s no secret that most diseases “cling” to a person precisely when they are overweight. Obesity not only puts undue stress on our skeleton, but also leads to endocrine imbalance.
- Prevention of adynamia - mandatory physical activity maintains a strong muscle corset, which provides additional protection and support to the spine.
- A balanced diet with sufficient amounts of calcium (see here for foods that contain the most calcium) and phosphorus.
Ertrusion is an early stage in the development of the hernia itself; surgical intervention is not necessary here; it can usually be managed with conservative treatment methods. The goal of treatment in this case is to eliminate inflammation of the pinched root, relieve swelling and eliminate the compression itself.
The basis of treatment, after the pain subsides, is therapeutic exercises
If necessary, the doctor can prescribe massages and physiotherapeutic treatment.
After the pain completely subsides, therapeutic exercises become the basis of treatment. It is this that allows you to restore the condition of the muscular corset of the body and improves the condition of the ligamentous apparatus. Thanks to this, it is possible to prevent relapses of the disease and the appearance of new hernias.
At the same time, the patient must understand that in the future he will need to independently perform exercises from the physical therapy complex, since the condition of the muscles and ligaments needs to be maintained. Also, very often the patient has to develop a new motor stereotype and learn to avoid provoking movements.
This is where conservative treatment ends; it is assumed that in the future the person will monitor the condition of his spine and follow these recommendations.
- Scoliosis, chondrosis without proper and timely treatment is the initial path to disc deformation and destruction. Small cracks appear on the fibrous ring, which will increase if outside help is not provided.
- The second stage of neglect of the spine is the formation of protrusion - this is the protrusion of the intervertebral disc in any direction due to the weak resistance of the walls of the fibrous ring, but without rupture of its tissues. The contents of the core are still contained by the ring, but the disk is no longer static. The protrusion at this stage ranges from 1 to 5 mm.
- A rupture of the annulus fibrosus is precisely an extrusion, when the internal substance cannot be restrained by a special barrier and freely exits into the outer cavity, changing the curvature of the spine and, in some cases, its height and elasticity.
Often, internal deformations in the spinal discs do not affect the transmission of impulses through the nervous and circulatory systems, which does not cause discomfort to a person. This depends on the location of the protrusion and extrusion of the intervertebral discs.
Therefore, more frequent visits to a neurologist remain cases when a hernia is diagnosed or surgical intervention is required due to the large size of the disc extrusion.
Prevention
It is strictly not recommended to use traditional methods of treatment as the main therapy. It is necessary to understand that extrusion between the vertebrae almost always leads to a hernia. Start monitoring your lifestyle, engage in moderate physical activity, and do light exercises for the spine several times a day.
Be sure to start eating right: a deficiency of vitamins and minerals can cause destructive changes in bone mass.
Give up bad habits, since drinking alcoholic beverages and smoking are factors that disrupt the natural metabolism in the body. The disease can be prevented with a timely preventive examination once a year. In the early stages, cracks and inflammation of the spinal column can be diagnosed. Such preventive measures will help to avoid surgical intervention, as well as long-term drug treatment.
source
Conservative methods of treating spinal hernia L5–S1
Treatment without surgery for L5–S1 disc herniation in the early stages of development is often successful and leads to normalization of the patient’s condition. But the duration of remission directly depends on how correct a person’s lifestyle is and what stress they are exposed to daily. But in order to achieve positive dynamics, therapy must be correctly selected and comprehensive.
Drug therapy
Necessary to eliminate pain, muscle spasms and improve the conduction of nerve impulses. For this purpose, NSAIDs, muscle relaxants, and B vitamins are prescribed. To accelerate the processes of cartilage tissue restoration, chondroprotectors can be used, but the effectiveness of drugs from this pharmacological group is not 100% confirmed.
Blockades
Injections of anesthetics (lidocaine, novocaine), sometimes in combination with corticosteroids, at certain points in the area of the affected spinal motion segment. They are used to quickly relieve acute pain, but can only be performed by qualified medical personnel under completely sterile conditions.
Manual therapy
A course of sessions conducted at a certain interval allows you to eliminate spasms of overstrained muscles and, conversely, tone overly relaxed ones. Restoring the correct anatomy of the spinal motion segment may even lead to a reduction in the size of the hernia.
Exercise therapy
A set of individually selected exercises allows you to strengthen the muscle corset and reduce the load on the affected area of the spine.
Physiotherapy
Aimed at reducing the intensity of pain, normalizing muscle tone and improving nerve conduction. For this purpose, a course of electrophoresis, magnetic therapy, and diadynamic current therapy is prescribed.
In certain cases, patients are recommended to undergo traction therapy, i.e., spinal traction. With its help, displaced vertebrae fall into place, and the distance between them increases slightly, which eliminates excess pressure on the affected intervertebral discs.
To increase the effectiveness of conservative treatment, patients can resort to additional methods:
- reflexology;
- kinesitherapy;
- osteopathy;
- hirudotherapy.
Forms of intervertebral disc extrusion
There are many reasons leading to disturbances in the structure of the discs, but the main factor is a failure in the supply of nutrients to a certain part of the spine and, as a result, wear and tear of the discs between the vertebrae and their gradual destruction.
Among the majority of circumstances leading to nutritional deficiency, the following are worth noting:
- The specifics of age-related changes in the body, when the tissues surrounding the spine begin to dry out.
- Various spinal injuries leading to displacement of discs and narrowing of the gaps between the skeleton, vascular system and nerve processes. Even birth trauma in infants without timely treatment can provoke the formation of extrusion in the future.
- Spinal pathologies - osteochondrosis, scoliosis, spondylitis, which were not diagnosed or the chosen therapy did not give positive dynamics.
- Excessive stress on the skeleton when lifting heavy objects without following certain rules. This may be due to professional activities when it is necessary to systematically lift weights, improperly carrying loads in front of you or on your back.
- Hormonal pathologies leading to metabolic failure. An unbalanced diet and, as a result, excess weight, which puts pressure on the spine every day.
Intervertebral extrusion is classified according to the place of formation of the changes and according to the characteristics of the protrusion of the internal substance:
- Cervical form of extrusion - changes occur in the discs of the cervical spine;
- Thoracic - ring deformation is formed in the thoracic vertebrae;
- Lumbar - pathology is localized in the lumbar vertebrae.
Cracks in the ring determine the location of the exit of the nucleus pulposus and this should be indicated when diagnosing extrusion, because it affects the choice of therapy and the manifestation of symptoms:
- Lateral, or lateral, when the protrusion is observed along the lateral projections of the spine;
- Dorsal, or posterior, in which a protrusion towards the soft tissues supporting the spine is visible;
- Central, when destruction of the fibrous ring leads to protrusion of the nucleus towards the spinal cord and varying degrees of compression of the brain.
A serious form of extrusion is considered to be subligamentary pathology, in which the longitudinal ligament of the spinal column is damaged.
Then the jackhammer principle comes into play - every human movement that loads the spine leads to the core “hitting” the fibrous ring. This, of course, is not a full blow, but simply increased pressure, but “water wears away stones.” Sooner or later, the fibrous ring begins to recede. The disc bulge begins to increase.
Let us note that while there is no pain, the only symptoms we see are increased fatigue. There is often a “kind soul” who advises in this situation to go in for sports to restore your back. But trainers at regular gyms have a slightly different understanding of the phrase “restore your back”; as a result, a person begins to perform exercises that further accelerate the development of the disease.
As a result, the nucleus pulposus finds a weak spot in the annulus fibrosus (which is already seriously damaged) and wedges into it, resulting in the second phase of the disease - disc protrusion
Please note that the fibrous ring has not yet been ruptured, the nucleus pulposus has not gone beyond its limits. There is simply a serious disc bulge
Symptoms of protrusion
In some cases, this stage of the disease may be completely asymptomatic if the bulging disc “has not reached” the nerve roots. Otherwise, the nature and localization of pain will depend entirely on the location of the protrusion. Local pain may appear in the back or neck, it can “radiate” to the leg or arm, in some cases the pain can spread to the intercostal spaces or the back of the head.
Also typical for protrusion are headaches, surges in blood pressure, dizziness, and numbness of the fingers (if the problem is in the cervical spine).
Kinesio treatment of intervertebral disc herniation
Kinesio therapy provides non-forced traction of the spine in a passive mode, in a lying position, without the active participation of the trunk muscles, with adjustment of the current gain (angle and amplitude of flexion and extension).
Thereby improving microcirculation in the area of compression by the hernia. In addition, therapeutic movements on the device develop deep muscles that are not used in normal life, and restore the rhythm and depth of breathing.