- Home >
- Clinic services >
- Orthopedics Center >
- Disc protrusion
- Protrusion of the thoracic intervertebral disc
- Treatment of disc protrusion
- Disc protrusion in the cervical region
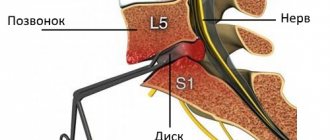
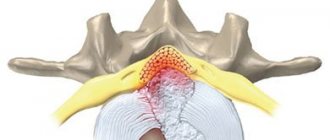
Disc protrusion is a pathology associated with degenerative changes in the intervertebral discs located between the vertebrae of the cervical, thoracic and lumbar spine.
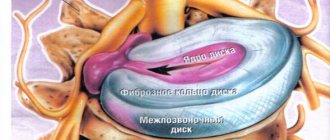
Intervertebral discs, due to their structure, impart elastic properties to the spine, which allows it to achieve a wide range of movements and alleviate the pressure placed on the spine in everyday life. This is due to the special structure of the discs, which include the annulus fibrosus and the nucleus.
The basis of the core is the pulp, a gelatinous substance consisting of proteoglycan with a high concentration of water. Around the nucleus pulposus there is a cartilaginous ring with a concentric layered structure - the fibrous ring, which holds the nucleus in a stable position.
With age, the water concentration decreases, structural changes occur in the pulp - it becomes harder due to dehydration, more susceptible to deformation.
The fibrous ring loses its elasticity and can gradually be pressed outward, forming a bulge - a protrusion.
Degenerative changes in the intervertebral discs can be aggravated by loads along the axis of the spine, which in turn leads to the development of microtraumas in it and the appearance of prerequisites for the formation of hernias. In some cases, the annulus fibrosus bursts, the pulp is squeezed out of the nucleus, and sometimes beyond the disc (sequestration).
Due to the pressure of deformed intervertebral discs, inflammation and swelling of the surrounding tissues occur. All this, along with the existing hernia, often leads to compression of the nerve roots or spinal cord. This, in very general terms, is the mechanism of pathogenesis of many complications of spinal diseases.
Classifications of protrusions
Protrusions are classified depending on the location of deformation changes:
- central protrusion - the bulge occurs at the back, towards the center of the spinal canal, where the spinal cord is located;
- paracentral, paramedian disc protrusion (“mid-right-sided” or “mid-left-sided”) - the bulge occurs towards the center with a shift to the right or towards the center with a shift to the left from the midline of the spinal canal, where the spinal cord and nerve roots are located;
- foraminal - protrusion occurs in the left or right side of the spinal canal, where the bases of the nerve roots are located;
- extraforaminal (lateral) - protrusion occurs to the left or right of the spinal canal, where the nerve roots extend from the spinal cord.
Compression of a spinal nerve root can result in symptoms known collectively as radiculopathy. Central (median) and paramedian disc protrusions that compress nerve roots may include symptoms such as:
- muscle weakness;
- pain radiating to the arm, leg, neck;
- numbness or tingling in the arms, one arm, or one or two legs;
- Urinary incontinence.
Treatment
Did you know that...
Next fact
The choice of treatment methods is related to the severity of the disease and the location of the problem area . At the initial stage, its goal is to minimize the load on the lumbar area; in most cases, bed rest and selection of an immobilizing corset are prescribed. There are several conservative treatment methods and surgical ones.
Medicines
Basic treatment with drug therapy is aimed at the following effects:
| Anti-inflammatory |
|
| Reduced swelling |
|
| Blocking muscle spasms |
|
| Normalization of cartilage tissue |
|
Surgery
It is used only when the conservative method is ineffective:
- If, despite taking medications, the pain does not subside for more than a month.
- In case of pronounced neurological pathologies with impaired leg movement.
- With progressive compression of the nerve roots against the background of immobility of the legs.
Treatment is carried out traditionally or using endoscopic technology (with minimal trauma). In this case, the destroyed parts of the disc are removed, which compress the nerves and adjacent tissues.
Removal of the median hernia is performed endoscopically
Exercise therapy, massage
The set of exercises for vertebral hernia is divided into 3 types: flexion, extension and traction. Only a specialist can combine these movements.
But there are general rules for exercise therapy for these pathologies:
- The muscles are pre-warmed. To do this, the body is rubbed, lightly pinched and patted, ensuring blood flow to the superficial vessels.
- The movements are smooth and slow, not abrupt.
- Twisting and maximum bending should be avoided.
- Jumping, pushing and aerobics are prohibited.
Massage serves to stimulate blood circulation in the problem area , relieve swelling, and improve metabolism. It is not used in the acute period with severe pain.
Treatment at home
Home treatment is possible only for the first and second stages of the disease , which corresponds to a protrusion of the hernia of no more than 8 mm. At the same time, exercise therapy classes are regularly attended under the guidance of a specialist, qualified massage is used, and if necessary, a course of drug therapy prescribed by a doctor is included. Physical activity is excluded, but movement is not contraindicated. Therapeutic walking in the air is practiced, and time at the computer is strictly dosed.
Prevention
To prevent and treat the disease, laser, magnetic and ultrasound therapy, mud therapy, other physiotherapeutic procedures, massage and exercise therapy are used . These procedures are combined with vitamin therapy, a balanced diet, and sometimes with a fasting diet.
The main prevention of spinal hernias is physical exercise.
Giving up bad habits and unhealthy foods reduces the risk of depletion of intervertebral discs. To avoid physical inactivity, you should not forget about daily walks in the air. To keep your discs hydrated, it is important to drink plenty of still water regularly.
People with a predominance of physical labor need to pay special attention to the dosage of physical activity , and if this is not possible, then wear special belts and bandages that protect the spine from overstrain. When lifting weights, you need to keep your back straight and squat, bending your legs. And when driving in a car, you should not forget about seat belts.
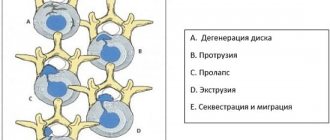
Protrusion and herniation of intervertebral discs
The protrusion process begins with a point bulging of the ring: a protrusion from 1 to 8 mm is formed from its fibrous plates. At the same time, the internal structure of the fibrous ring has already been destroyed, and, most likely, significantly - by the time protrusion appears, usually more than half of the outer shell of the disc is cracked and has lost its functionality. But the outer, stronger layer of the disk still holds the core.
In the scientific literature, especially foreign, a herniated disc is considered to be a localized displacement of part of the disc (nucleus pulposus, cartilage, collagen rings in various combinations) outside the intervertebral disc space, generally speaking, both when the fibrous ring is ruptured (prolapse) and when the integrity of the outer, more durable layers of the fibrous ring (protrusion). In popular scientific literature and in everyday life, a hernia is most often understood as prolapse - loss of the internal tissues of the ring through a rupture of its outer shell.
Thus, protrusion in a simplified view is the initial stage of the formation of a hernia, but at the same time it can lead to consequences no less serious than a developed disc herniation. In the diagram you can see that the main threat is not so much the rupture of the fibrous ring, and not the bulge of the disc itself, but its size and location in relation to the nerve roots and spinal cord, compression of which will inevitably lead to the occurrence of pain and other consequences.
Not every protrusion causes concern and threatens health, just as not every protrusion will inevitably turn into prolapse. But the presence of protrusions of any type and size in the intervertebral discs indicates the development of degenerative processes in the spine and should be an incentive to begin timely treatment of osteochondrosis in order to avoid severe stages of the disease and complex surgical intervention.
Surgery for dorsal hernia
If conservative therapy does not produce positive results within 1–3 months, patients are advised to consult a neurosurgeon and determine whether there are indications for surgical treatment. It is carried out when:
- sequestered hernias;
- severe neurological disorders;
- loss of control over urination and defecation (often caused by a dorsal median disc herniation of L5–S1 measuring significantly more than 0.5–0.6 cm);
- decreased quality of life.
Surgical treatment of dorsal disc herniation L5–S1 or any other can be carried out using different methods:
- puncture surgery (nucleoplasty and hydroplasty);
- endoscopic surgery;
- microdiscectomy.
Shaboldin A.N.
microsurgically removes a herniated disc. Which one is optimal for a particular patient is decided individually by neurosurgeons. If the operation involves the removal of a significant part of the nucleus along with the fibrous ring, the patient will be offered the installation of a special Barricaid mesh to prevent recurrence of the hernia in the same place.
In cases where it is necessary to remove the entire affected disc, it must be replaced with a fully biocompatible and highly functional M6 endoprosthesis. If this is not possible for one reason or another, neurosurgeons will likely recommend transpedicular fixation.
M6 intervertebral disc prosthesis
In both cases, there is no recurrence of the hernia at the same level, since the disc itself has been removed, but there remains a possibility of its formation at other levels of the spine if the patient does not follow the doctor’s recommendations and does not change his lifestyle.
Nucleoplasty
Puncture surgery involves reducing the volume of the nucleus pulposus by destroying part of it with laser energy, radio waves, cold plasma or liquid pressure. The instrument is inserted through a pinpoint puncture of soft tissue, the size of which does not exceed a few millimeters.
The method using liquid pressure is recognized as one of the most effective and safe, since it does not involve the risk of overheating of surrounding tissues and provides a high degree of control over the volume of intervention performed. It is called hydroplastic.
SpineGet hydronucleoplasty device
But the use of puncture surgery methods is only possible for dorsal disc herniation measuring up to 0.7 mm. Moreover, if the patient does not change his usual lifestyle, continues to spend a lot of time in a sitting position or, on the contrary, performs too hard physical work, a hernia can form again either in the same spinal motion segment or in another.
Endoscopic surgery
A gentle method of surgical treatment of dorsal hernia, used when it is located in a narrow place of the spinal canal or is large in size. Unlike nucleoplasty and hydroplasty, the operation is performed under general anesthesia and requires hospitalization for one day.
Shaboldin A.N. endoscopically removes a herniated disc
At the same time, it is quite low-traumatic, since all manipulations are also performed through pinpoint punctures of soft tissues. A thin port (hollow tube) is installed through which, under a video camera, the herniated disc is removed. Intraoperative risks are insignificant, since access to the affected intervertebral disc is provided through the use of a shaver.
Microdiscectomy
Microdiscectomy is an open, but low-traumatic operation, performed through an incision of about 2 cm. It is performed under general anesthesia and allows you to remove almost any hernia, including sequestered ones.
Remote disc herniation
In particularly difficult cases, some patients may require a rather traumatic operation - laminectomy. This operation involves access to the spine through a large incision, but allows you to carefully examine all anatomical structures and solve a complex of problems in this area. As a result, not only the entire disc, but also part of the vertebra may be removed.
Prerequisites for the occurrence of intervertebral disc protrusion
The occurrence of protrusions depends on a number of circumstances, ranging from preventable causes (for example, injury, inadequate physical activity, improper lifting and moving objects) to inevitable (genetics, aging).
In addition to degenerative processes in the spine (osteochondrosis), there are other predisposing factors, such as:
- constitutional weakness of the ligaments,
- congenital pathology of the spine;
- incorrect posture during work;
- pregnancy;
- obesity;
- falls on the buttocks, legs, injuries, weightlifting;
- bending, torsion of the spine;
- weakness of the abdominal muscles and muscles that support correct posture.
These and other reasons can lead to protrusion of the annulus fibrosus, usually on the posterior side, where the annulus fibrosus is thinner, up to rupture of the nucleus pulposus and the formation of a prolapse (hernia) into the epidural space of the spinal canal with the appearance of symptoms of compression of nerve tissue.
What are the symptoms of the disease?
Affected discs may not cause any clinical manifestations, but more often present with pain. It happens that intervertebral disc protrusion is not diagnosed immediately, as patients come with vague pain in the hips, knees or legs. Although it is theoretically possible for a hernia to appear in any part of the spine, in practice, as a rule, patients are faced with damage to the intervertebral discs in the cervical and lumbar regions. The onset of protrusion formation can be acute, due to injury or sudden movement, or develop slowly, progressively, without visible external causes.
Symptoms of intervertebral disc protrusion may vary depending on the location of the hernia and the type of soft tissue that is affected by it. They can range from a pain-free existence, where a bulging disc is the only change, to severe and unrelenting pain in the neck or lower back that radiates to adjacent areas. Other symptoms may include sensory changes such as numbness, tingling, or a crawling sensation; Muscle weakness, paralysis, and changes in reflexes may occur.
For example, in the case of a disc protrusion in the lumbar region, the patient may experience pain along the outer or back surface of the leg, a feeling of “muscle spasm,” numbness or tingling in these areas.
Damage to the nerves in the lumbosacral region can lead to loss of bowel and bladder control, as well as sexual dysfunction (cauda equina syndrome).
After the appearance of protrusions of the cervical intervertebral discs, pain occurs, localized in the neck and sometimes in the arms. Typically, symptoms are experienced on only one side of the body.
If the bulge is very large in shape and volume, pressure on the spinal cord can cause pain on both sides of the body, often with serious consequences, which can lead to permanent nerve damage or paralysis.
Protrusions can cause secondary changes in the spine, such as:
- intervertebral disc herniation - rupture of the fibrous ring.
- Spinal stenosis is a narrowing of the spinal cord canal, which leads to compression of the spinal cord and the nerve roots emerging from it. Stenosis can also be the result of thickening of the ligaments, the presence of posterior marginal growths, and other reasons.
- Osteoarthritis of the intervertebral joints is the result of wear and tear of the articular cartilage in the intervertebral joints. In this case, the distance between the vertebrae decreases, which changes the relationship of the articular surfaces to each other, as well as the mechanics of the joint itself.
Protrusion in the lumbar region
The lumbar spine constantly experiences the greatest loads, as a result of which protrusions occur in it much more often. Its clinical manifestations are as follows:
- pain in the lower back of an acute or chronic nature, radiating to the lower extremities;
- attacks of radiculitis;
- a feeling of stiffness in the lower back, limited mobility;
- dysfunction of the pelvic organs;
- numbness of the lower extremities;
- weakness in the legs, paralysis.
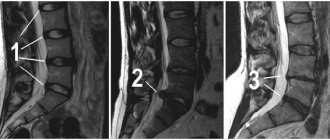
Diagnosis of intervertebral disc protrusions
If you experience back pain in the lumbar region, neck, sensory disturbances in the limbs and other symptoms described above, you should consult a neurologist and undergo an examination.
To diagnose degenerative changes in the spine, the doctor usually finds out the presence of typical painful symptoms, concomitant rheumatic diseases, sensory and motor disorders, and deterioration of reflex activity. In addition, MRI plays a decisive role in forming an objective diagnosis.
Treatment at the Energy of Health clinic
Neurologists at the Energy of Health clinic will come to the rescue both at the first signs of protrusion and at an advanced form of the disease. We will conduct a comprehensive diagnosis to accurately determine the type and degree of pathology, and also prescribe adequate and effective treatment, including:
- modern drug regimens for high-quality pain relief and elimination of radicular syndrome, including injections of long-acting agents;
- drug blockades for quick pain relief;
- physiotherapy, massage and manual therapy in the absence of contraindications;
- physical therapy directly in the clinic, as well as drawing up a daily home workout plan;
- organization of sanatorium-resort treatment during remission.