Aging of the musculoskeletal system is an irreversible process. With age, each of us increases the risk of degenerative-destructive changes, especially if the dosage of physical activity is incorrect and microtraumas are ignored.
Deforming arthrosis of the ankle joint is a disease that can be successfully treated at the initial stage, when the first signs appear. In advanced cases, the disease can seriously complicate life and even lead to loss of ability to work.
In the treatment of ankle arthrosis, much depends on the patient
Arthrosis of the ankle - what is it?
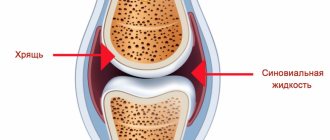
Osteoarthritis of the ankle joint
is a disease whose progress is accompanied by the destruction of the cartilage tissue of the joint of the lower extremities, as well as the adjacent bones.
It is also worth noting that osteoarthritis of the ankle joint is characterized by a chronic nature and undulating course (systematic periods of exacerbations followed by remissions).
The disease is characteristic mainly of people of the older generation, but recently it is increasingly occurring in a situation where arthrosis is diagnosed in people under 45 years of age. According to statistical data, destruction of the cartilage tissue of the ankle is detected in 6% of applicants.
Timely diagnosis and a well-defined treatment plan for ankle arthrosis can completely cure the disease.
Degrees of the disease
For ankle arthrosis, three degrees are distinguished, which are specified by hardware diagnostics:
- I degree - pathological changes are not noticeable, there is a narrowing of the gap of the ankle joint, compaction of the talus;
- II degree – as a consequence of the progression of the disease, swelling occurs, pain appears in the weather, leg mobility decreases, and joint deformation is noted;
- III degree – there is a loss of shock-absorbing properties of the joint, ossification of cartilage tissue, and deformation of the foot leads to disability.
Main causes and principles of progression of ankle osteoarthritis
Arthrosis of the ankle joint is a special disease that can be a primary phenomenon, or it can be secondary, in which the disease progresses after injury or inflammation.
Regardless of the type, arthrosis occurs mainly in conditions of disruption of the natural processes occurring inside the articular cartilage.
Considering the key factors in the development of the disease, it is worth highlighting:
- microtraumas, as well as major injuries to the ankle joint;
- excess body weight;
- performing surgery on a joint;
- improperly selected shoes, abuse of high heels;
- excessive physical activity;
- metabolic disorders caused by various diseases (gout, hormonal imbalance);
- diseases of the musculoskeletal system;
- genetic predisposition;
- bad ecology.
Under conditions of normal metabolic processes, the superficial articular tissues are characterized by smoothness and elasticity, ensuring unhindered gliding during movement.
When a joint is injured or metabolic processes are disrupted, the smoothness and elasticity of the tissues is lost, which causes friction and significantly aggravates the consequences.
Diagnostics
The diagnosis of “grade 2 arthrosis of the ankle joint” (or any other stage) is made based on a survey, visual examination and laboratory results. X-rays play a decisive role. At the most advanced stages, deforming osteoarthritis and cyst-like formations in the bone area are detected. In difficult cases, the patient is referred to a CT scan of the ankle for a more accurate assessment of the bone structures. An MRI of the ankle may be prescribed to examine soft tissues.
- Arthrosis of the ankle joint - causes, symptoms, diagnosis, degrees of disease and treatment
Types and degrees of ankle osteoarthritis
Today, it is customary to distinguish two types of arthrosis localized in the ankle joint:
- primary
– the development of pathological processes directly on healthy cartilage tissues; - secondary (post-traumatic)
– degenerative processes that occur during the development of various types of diseases/injuries.
In addition, modern medicine also distinguishes several degrees of degenerative disease:
Arthrosis of the ankle joint 1st degree
– the first stage of the development of the disease, accompanied by a clear manifestation of symptoms. Patients complain mainly of symptoms such as:
- increased fatigue;
- leg pain.
During diagnostic procedures, pathological processes are practically invisible, which complicates the process of identifying the disease.
Arthrosis of the ankle joint 2 degrees
– manifests itself in severe pain that disrupts the healthy sleep of patients.
Visual signs of the disease appear. Inflammation of the joint becomes visually noticeable: a local change in the color of the skin (redness) occurs, as well as an increase in its temperature. In addition, swelling begins, movements are limited.
Arthrosis of the ankle joint 3rd degree
– accompanied by pronounced discomfort and severe aching pain, which is a sign of the beginning of the transformation of cartilage into bone tissue.
Joint mobility is limited or completely lost. Joint movements occur with a crunch.
The lack of necessary treatment for arthrosis of the ankle joint in the later stages of the disease inevitably leads to loss of ability to work and obtaining the “disabled” status.
When should you sound the alarm?
At the initial stage, ankle arthrosis, as a rule, does not make itself felt, and yet there are indirect signs that cannot be ignored:
- fatigue in the legs that was not there before;
- unusual fatigue;
- minor pain, especially after intense physical activity.
Among athletes, who constitute the main risk group for arthrosis, they often do not pay attention to mild pain and minor limitation of movement. Meanwhile, it is these symptoms that indicate the onset of degenerative-dystrophic changes in the ankle joints. At this stage, drugs that improve metabolism are sufficient to treat deforming arthrosis of the ankle joint. If the moment is missed, the therapy will be much more serious.
It is not difficult for an orthopedic doctor to diagnose arthrosis even at the initial stage
Symptoms of ankle arthrosis
Before understanding how and how to treat osteoarthritis of the ankle joint, it is important to identify its symptoms.
Considering the clinical picture of the disease, one can notice that the key symptoms of arthrosis localized in the ankle joint are increased fatigue and severe pain. As the disease develops, the situation worsens, which leads to increased pain that does not go away even during periods of rest and long sleep.
Over time, the motor activity of the affected joint is significantly limited, and a fairly severe deformation of the ankle is visually visible. However, in addition to this, symptoms of ankle arthrosis include:
- an increase in pain even with minor exertion;
- discoloration of the skin and swelling of the tissues of the affected joint;
- swelling of the foot;
- characteristic crunch when moving the joint;
- loss of the ability to freely move the ankle;
- local increase in temperature indicators.
The presence of just a few or even one symptom of ankle arthrosis should be the reason for urgently seeking qualified medical help.
Clinical picture
The first clinical manifestation of the pathology is pain, which intensifies when walking, especially when going up or down stairs. Post-traumatic arthritis is often accompanied by crepitus. This is the medical name for characteristic clicks and crunches during movement or flexion-extension of a joint. At rest there are no discomfort sensations. But another specific symptom of the pathology is “starting pain.” It occurs at the beginning of movement after a long rest in a sitting or lying position.
As destructive and degenerative changes in the ankle progress, the intensity of the pain syndrome increases. Other signs of joint damage also occur:
- aching pain disturbs a person at night or during sudden changes in weather;
- the range of motion in the ankle decreases, “stiffness” develops;
- swelling remains in the joint area, increasing in the morning;
- when palpating the joint, pain and uneven swelling are felt;
- the axis of the damaged limb is bent;
- The ankle deformity gradually worsens.
In the absence of medical intervention at the initial stage of post-traumatic arthrosis, it takes a relapsing course. Stages of remission alternate with painful relapses. Muscle contracture may develop, and reflex ankle spasms become chronic. The person avoids full support on the leg and begins to noticeably limp. With a disease of high severity, the joint loses mobility, dislocations, subluxations, ruptures of ligaments and tendons become common.
With exacerbations of post-traumatic arthrosis, synovitis often develops. The synovium becomes inflamed, and exudate accumulates in the joint cavity. This not only accelerates the progression of arthrosis, but also provokes symptoms of general intoxication of the body: fever, fever, indigestion, headaches.
Which doctor should I contact and how to treat arthrosis of the ankle joint?
Doctors such as an orthopedic traumatologist and a rheumatologist treat osteoarthritis of the ankle. If you suspect the presence of a disease, you should refrain from self-medication. Ignoring symptomatic manifestations can aggravate degenerative processes and lead to extremely negative consequences.
Arthrosis of the ankle joint grades 1 and 2 can be successfully treated. For this reason, when the first signs appear, it is important to contact your local physician, who will refer you to a specialist for diagnosis.
Despite the complexity of the situation, grade 3 ankle arthrosis is also treatable, but mostly radical measures are used.
Today, various methods are used to treat ankle arthrosis, including non-drug therapy and medication.
Let's look at the available methods in more detail.
Physiotherapy for ankle osteoarthritis
Physiotherapy
is a unique area of modern medicine that uses natural as well as artificially created physical capabilities for the prevention and treatment of various diseases.
The use of physiotherapy as a treatment for ankle osteoarthritis makes it possible to significantly reduce the amount or completely eliminate the use of medications.
Physiotherapy methods help to significantly improve blood circulation in the affected joint, which ensures activation and acceleration of the recovery processes occurring inside the ankle.
In the treatment of ankle osteoarthritis the following are used:
- laser irradiation;
- ultrasonic influence;
- electrical stimulation.
Treatment of ankle arthrosis is determined in accordance with the symptoms that appear and the intensity of the disease.
Massage and ankle arthrosis
Massage
is a complex of mechanical and reflex techniques, the use of which ensures increased blood circulation, which significantly accelerates the restoration of affected tissues.
Treatment of ankle osteoarthritis with massage, in addition to reducing the rate of progression of the disease, helps prevent the likelihood of its exacerbation.
Only a specialist who knows the structural features of the joints can perform a massage to treat arthrosis of the ankle joint. It is important to note that the duration of the massage should be at least 25 minutes.
Using massage in tandem with exercises for arthrosis of the ankle joint will ensure the achievement of the most effective results in a relatively short time.
Exercises and exercise therapy for ankle arthrosis
Despite the fact that many are of the opinion that physical therapy (physical therapy) for arthrosis is ineffective, physical activity is the key to getting rid of hated pain and significantly improving well-being.
Correctly selected exercises for arthrosis of the ankle joint lead to:
- eradication of the feeling of stiffness when walking;
- activation of blood circulation in the internal tissues of the joint;
- slowing down, and in some cases even completely stopping the course of the disease;
- restoration, improving quality of life.
It is important to note that for osteoarthritis of the ankle joint, exercises are selected exclusively in accordance with the recommendations of the attending physician.
Surgical intervention for osteoarthritis of the ankle joint
In a situation where conservative treatment of ankle osteoarthritis does not produce the desired results, a more radical method of eliminating the disease comes to the rescue - surgery.
Today, the following types of surgical intervention are possible:
- endoprosthetics
– complete replacement of the ankle joint; - arthroscopy
– elimination of excessive formations inside the ankle; - arthrodesis
– immobilization of the ankle while preserving remnants of cartilage.
Surgery falls into the category of last resort methods for treating ankle arthrosis. Timely diagnosis and a well-structured treatment plan can prevent the need for radical measures.
In order to consolidate the postoperative result and speed up the recovery of the joint, specialists prescribe a set of exercises for osteoarthritis of the ankle joint.
Is there an alternative to surgery?
In difficult cases, when conservative treatment of arthrosis of the foot has not helped and there is no mobility, surgery is indicated. Like any surgical intervention, endoprosthetics (replacing a joint with an implant) has contraindications and carries certain risks. Today, fortunately, this is not the only way to restore joint health - this can be done at the second or third stage of the disease, with the help of a synovial fluid endoprosthesis.
For example, the biopolymer with silver ions “Noltrex” is intended for intra-articular administration in a sterile dressing room. Its task is to restore the viscosity of the synovial fluid in the affected ankle joint. The drug reduces friction in the joint, which relieves pain and improves mobility. However, Noltrex does not affect the metabolism of cartilage. A feature of the Noltrex endoprosthesis is its very slow biodegradation, which explains its long-term effect (at least six months).
The synovial fluid endoprosthesis is inserted under local anesthesia in a dressing room or operating room. Here's how it works in the case of the ankle joint:
After inserting a synovial fluid implant, it will not be superfluous to prevent complications. Orthopedic doctors recommend that physical activity be dosed correctly, monitor nutrition and body weight, and that athletes respond to injuries and microtraumas in a timely manner. Movement is life, and ankle health is the key to an active lifestyle!
Treatment of ankle arthrosis with drugs
Drug treatment of ankle arthrosis is part of complex therapy, providing the opportunity to relieve unpleasant symptoms and stop degenerative changes.
How to treat arthrosis of the ankle joint can only be determined by a specialist who knows the characteristics of the disease being diagnosed. Self-medication with medications can cause irreparable harm to the body.
All drugs for the treatment of osteoarthritis of the ankle joint are divided into several groups, each of which differs not only in the principles of action, but also in the degree of effectiveness.
Let's look at some of them in more detail.
Anti-inflammatory and painkillers
Nonsteroidal anti-inflammatory drugs for the treatment of osteoarthritis of the ankle joint are used at various stages of the development of the disease.
The key focus of this type of action is to relieve pain and relieve inflammation in the joint.
Today, the medicine market offers anti-inflammatory and painkillers not only in the form of gels and ointments, but also in the form of tablets, patches and injections, the most effective of which are considered to be “Artradol”, “Ketoprofen”, “Structum” and “Aceclofecan” .
Antispasmodics-muscle relaxants
Drugs for the treatment of osteoarthritis of the ankle joint, such as antispasmodics and muscle relaxants, are prescribed as an active aid in the fight against spasms of the muscles adjacent to the affected joints.
Antispasmodics provide muscle relaxation and pain relief. Mydocalm is considered to be the most relevant drug today.
Chondroprotectors
Chondroprotector
is a drug for the treatment of osteoarthritis of the ankle joint, providing stimulation of the production of a sufficient amount of intra-articular fluid, which ensures accelerated tissue regeneration and saturation with essential vitamins and minerals.
The most effective effect is provided by the drug "Artracam", which has proven itself in the market of modern medicines.
Basics of conservative treatment
First of all, it is important to eliminate the provoking factors, otherwise the treatment will not be effective. For some it’s excess weight, for others it’s high heels or standing for long periods of time. It will never be a bad idea to switch from flour, salted and smoked foods to fiber, fresh fruits and fermented milk products in order to stabilize the metabolism.
After such recommendations, the patient is prescribed medication according to indications:
- non-steroidal anti-inflammatory drugs and painkillers (tablets, ointments, injections);
- chondroprotectors containing glucosamine sulfate and chondroitin sulfate to give the cartilage layer density and elasticity (taken for a long time - more than six months).
Complex treatment may include:
- physiotherapy (regular procedures stop destruction in the joints);
- therapeutic massage - to strengthen the muscles of the foot and lower leg, as well as improve blood circulation;
- wearing orthopedic shoes that reduce the load on the joint;
- hiking and swimming;
- sanatorium-resort treatment in specialized health resorts.
Best way to restore ankle mobility - swimming and walking
Possible complications
In the absence of comprehensive treatment for ankle arthrosis, the likelihood of complete recovery is reduced to almost zero.
Self-treatment and ignoring the symptoms of the disease inevitably lead to limb immobilization and disability.
In the presence of symptoms and insufficient treatment of arthrosis of the ankle joint, the progress of destructive processes causes the occurrence of osteophytes (growths on bone tissue), which negatively affects a person’s quality of life.
Constant swelling of the tissues of the affected joint can also cause the development of pathological processes in the blood vessels, in particular, deterioration of blood circulation, impaired blood flow.
Long-term destructive processes developing in the joint lead to immobilization of the ankle, which increases the risk of concomitant diseases and injuries.
Development mechanism
Due to injury, a disruption occurs in the structure of articular or cartilage tissues. The bones change position in relation to each other and can no longer move safely. Cartilage ceases to perform a shock-absorbing function and becomes deformed, and a lack of synovial fluid develops in the joints. Competent treatment can stop this process.
Sometimes therapy for post-traumatic arthrosis may be needed after surgery. During surgery, soft tissues and muscles are damaged, scars form on them, which makes proper nutrition of the joints impossible. This leads to inflammation and then to degenerative phenomena.
The disease most often affects the knees, which bear the maximum dynamic load. A synovial fluid prosthesis of the knee joint or complex therapy can help solve the problem. Representatives of certain professions, such as massage therapist, painter, tennis player, are also at risk. Their degenerative phenomena manifest themselves due to regular injury to the elbow joints.
Older people are most susceptible to post-traumatic arthrosis
Basic principles of dietary nutrition for ankle arthrosis
According to numerous studies, it has been noted that arthrosis mainly occurs in people who do not follow their diet.
Following a diet and taking into account certain nutritional principles speeds up the treatment of many diseases, in particular arthrosis.
The key principle of nutrition for arthrosis is balance. In addition, criteria such as:
- regularity of meals;
- variety of food products;
- correspondence between nutritional value and intensity of energy expenditure.
During the period of treatment and rehabilitation, the patient's diet should consist mainly of dishes prepared using gelatin. In addition, it is important to give preference to foods enriched with vitamins of various groups and other beneficial microelements.
To speed up your recovery, it is also recommended to avoid drinking sugary carbonated drinks and alcohol.
Arthrosis 3 degrees
The most serious degree of development of arthrosis of the lower leg joint. The symptoms of the disease are very pronounced and cause serious discomfort to the person. Characterized by deviations:
- The articular bone constantly grows, a large amount of excess fluid accumulates in the joint cavity, and significant deformation of the joint occurs.
- Restriction in ankle movements. In some cases, it is possible to perform rocking actions. Restrictions in activities may require the doctor to register a disability.
- The constant presence of acute, severe pain, the condition is also typical in a state of rest and rest. The pain is caused by constant painful spasms of the muscles located nearby. Spasms are reflexive in nature. Reactive synovitis develops.
- A serious inflammatory process occurs in the joints.
- The damaged joint reacts with pain to changes in weather conditions.
- The muscles around the ankle joint are atrophied and subject to constant spasms.
Limb bending often occurs.
X-ray photographs show complete disappearance of the articular cavity, the cartilage of the joint is severely deformed. On the surface of the joint, an increase in the number and size of osteophytes.
The patient's disability will occur with a severely advanced form of grade 3 ankle arthrosis. In such situations:
- Constant severe pain is felt, movements, especially on the stairs, become a test;
- The crunching in the ankle joints is clearly audible to others.
- Movements are limited, sometimes impossible;
- The joint is severely deformed.
The photographs show destruction of the ligaments, lack of cartilage, and the formation of sclerosis.
Prevention of ankle osteoarthritis
The best treatment for ankle osteoarthritis is prevention
.
To minimize or completely eliminate the likelihood of degenerative-dystrophic processes in the ankle, experts around the world recommend adhering to the simplest principles:
- constant monitoring of diet;
- tracking and control of optimal body weight;
- caution and avoidance of injuries to the lower extremities;
- allocating enough time for a good warm-up before physical activity;
- timely treatment of inflammatory diseases;
- maintaining an optimal balance of microelements in the body.
Compliance with the simplest preventive recommendations will eliminate the likelihood of symptoms of ankle arthrosis and limit the need to treat ailments of this kind.
Remember, consulting a doctor when observing the initial symptoms of osteoarthritis of the ankle joint guarantees its timely diagnosis and high-quality, successful treatment.
Traditional methods
Village recipes come to the aid of complex therapy of the ankle joint for arthrosis:
- Symptoms and treatment of deforming arthrosis of the ankle joint
- Chalk and kefir. Mix the two ingredients to form a paste. Apply this mixture to the sore joint at night to relieve swelling.
- Butter and cinquefoil root. Mix the ingredients in a ratio of 10:1 and rub into the sore joint at night to relieve pain.
Massage
First of all, you need to remember that massage cannot be done during an exacerbation! In the subacute period, the muscles are massaged as usual, and only stroking and light rubbing are used for the joint. During the remission stage, you can massage more actively.
- How to treat arthrosis of the foot at home: folk remedies and medications, video
- The session begins with a massage of the lower leg muscles: first the back surface, then the sides. Particular attention is paid to the Achilles tendon. Gradually descending to the joint, soften the impact and reduce the pace. Finish by rubbing the front surface of the foot.
- Each transition to a different massage area begins and ends with stroking and/or rubbing. Kneading can be used on the muscles. Excluded: vibration and shaking.
The duration of one procedure is 20–30 minutes. Massage should be performed every day (you can do it 2 times a day before physical education or physiotherapy). It should be done in courses of 10–15 sessions with a break of 1–3 weeks.