Due to their mobility and high activity, the joints of a person’s lower extremities are subject to significant daily loads, especially the ankle. In this regard, they tend to wear out over time and suffer various diseases.
Arthrosis of the ankle joint - today this disease is very common, the main cause of which can be called upright posture. Walking and bearing the weight of the human body lead to thinning of the cartilage covering of the joint, cracking, triggering the inflammatory process and the formation of osteophytes. Advanced stages of arthrosis are accompanied by severe pain and deprive a person of the ability to walk fully, and sometimes even leave him immobile. It is very important to receive adequate treatment in a timely manner when the first symptoms begin to appear, and also not to forget about the prevention of arthrosis.
ICD-10 code: (M15-M19) – Arthrosis.
Reasons for the development of the disease
Chronic disease of the ankle joint - arthrosis - is a degenerative change in the articular cartilage. As the disease progresses, the cartilage begins to break down. Subsequently, bones, joint capsule, and ligaments are involved in the pathological process.
The causes of the disease may be:
- overweight person, which creates additional stress on the joint;
- congenital foot deformities, such as clubfoot, cauda equina, or flat feet;
- metabolic disorders, which can manifest themselves in diseases such as gout, diabetes mellitus, atherosclerosis of the joints of the lower extremities;
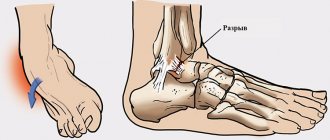
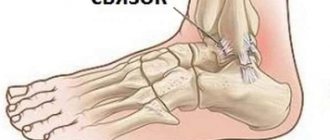
- various injuries of the lower extremities, damage to the ligamentous apparatus, fractures of the bones of the foot or ankles;
- systematic physical overload of the ankle joint, its microtraumatization, for example, in people carrying heavy loads or in athletes;
- predisposition to a hereditary disease;
- some diseases of an inflammatory, infectious nature, as well as systemic illnesses, for example, rheumatoid arthritis.
The first symptoms of this disease play an important role.
Clinical picture of the disease
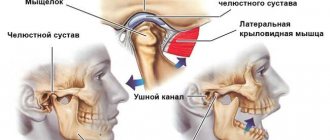
The ankle joint is composed of two ankles, articular ligaments and talus bones (tibia and fibula).
When an inflammatory process develops in the articular cartilage, arthrosis is diagnosed. The pathological process leads to tissue destruction, thinning of cartilage and a decrease in its strength.
In the process of inflammation, bone formations grow, which leads to ankle deformation.
According to the international classification of diseases, ankle arthrosis is assigned the ICD-10 code M19. The disease develops suddenly under the influence of predisposing factors.
At the earliest stages, there is no symptomatic manifestation; incipient pathological changes can only be detected by x-ray. Over time, the signs of arthrosis will intensify as the degree of inflammation increases. The advanced form of the disease becomes a cause of disability.
Stages and forms
Arthrosis of the ankle can be primary or secondary. In the first case, the disease develops independently in an initially healthy joint, in the second, it is a consequence of trauma to the cartilage or a complication of another disease associated with it. Based on its origin, arthrosis is divided into several categories:
- Post-traumatic – caused by ankle injury
- Dysplastic – caused by undiagnosed and untreated dysplasia
- Static – resulting from a disproportionate division of the load on the joints over a long period of time
- Post-inflammatory – occurring during acute or chronic inflammation of cartilage
Depending on the location, arthrosis can develop on the right ankle or on the left. Most often, bilateral pathology is diagnosed. The disease occurs in 3 stages.
Stage 1 is characterized by an asymptomatic course of pathology in bone tissue. At stage 2, the deformities are more pronounced, and pain appears in the affected area. At the final stage, an exacerbation of all symptoms occurs, contributing to the loss of joint mobility. It is at this stage that the likelihood of becoming disabled is high.
Symptoms of ankle arthrosis
Arthrosis of the ankle joint in the early stages may have subtle symptoms, however, if timely treatment is not given, the disease can progress and have quite serious consequences for the patient.
Main symptoms of the disease:
- starting pains that can occur after a night's sleep or prolonged sitting, when a person tries to lean on his legs;
- a feeling of stiffness in movement, especially after a long period of rest, in which the patient needs a certain time to disperse;
- aching pain associated with the development of the inflammatory process;
- specific crunching of the ankle joint, clicks when the patient tries to make movements;
- the occurrence of swelling, especially pronounced in the area under the ankles;
- restriction of usual mobility;
- wasting of the muscles located around the sore ankle joint, as well as weakness of the ligamentous apparatus, which can occur when the patient tries to spare the sore leg;
- deformation of the diseased ankle joint, which is characteristic of the last stages of arthrosis.
At the first symptoms, you should not delay treatment and consult a doctor.
- Arthrosis of the ankle: causes of development, symptoms, treatment and prevention of the disease
Symptomatic manifestation
At a very early stage, the disease occurs without visible changes in the ankle and general well-being. As the stage of development of arthrosis increases, the manifestation of symptoms intensifies. The general clinical picture may look like this:
- When sitting for a long time or leaning on the sore leg, a short-term feeling of stiffness occurs, which disappears a few minutes after the start of movement.
- When applying a load, the pain in the joint intensifies.
- When moving, a crunching, clicking or squeaking sound is heard.
- There is some stiffness of movement.
- The axis of the lower leg is bent.
- Atrophy occurs in the muscles adjacent to the injured area.
- The joints may become swollen.
- The temperature of the feet increases.
- Subluxations occur more often.
As the disease progresses, some symptoms become more pronounced, and the discomfort becomes unbearable. Immediate medical attention is required to avoid complications or complete destruction of the cartilage.
Treatment of ankle arthrosis
Patients with suspected ankle arthrosis who notice characteristic symptoms of the disease should not delay visiting a doctor. The specialist will be able to conduct an examination and immediately make the correct diagnosis, as well as prescribe the optimal treatment in accordance with the stage of arthrosis. An X-ray examination may be prescribed as additional diagnostic measures. The images can easily distinguish narrowing of the joint spaces, even small ones, and also show deformations and bone growths in the later stages of the disease.
As a rule, treatment for arthrosis of the ankle joint is aimed at solving such problems as pain relief and relieving the inflammatory process, regeneration of affected cartilage tissue, expanding the range of joint movements, improving metabolic processes in the joint and the anatomical areas of the foot and lower leg located nearby.
To solve these problems, the patient may be prescribed the following treatment methods:
- drug therapy with the use of non-steroidal anti-inflammatory drugs, glucocorticoids, anesthetics, joint agents, muscle relaxants, chondoprotectors, hyaluronic acid preparations;
- physiotherapeutic procedures, including magnetic therapy, UHF, laser therapy, SMT;
- therapeutic massage session;
- physical therapy classes;
- use of folk remedies;
- wearing orthopedic insoles and choosing comfortable shoes without heels;
- surgical intervention with prosthetics.
Treatment of pseudarthrosis
When a false joint occurs, treatment without surgery is impossible. I surgically fix the affected area again to form a callus and ossify.
For this purpose, osteosynthesis is performed according to Ilizarov. For the operation, an external fixation device is used, which the patient wears for about 6 months.
Ladisten Medical Center performs minimally invasive surgical interventions. The method has proven its effectiveness over 30 years of practice. The new design used, the Veklich apparatus, has a patent.
Dr. Veklich’s device is a reliable device for bone fusion; the device is quite lightweight and has improved ergonomics. It does not involve the use of traumatic needles, thereby reducing the risk of infection and rehabilitation time.
Gymnastics for the ankle joint with arthrosis
A special place in complex treatment is given to therapeutic exercises. By performing a set of special exercises, you can relieve muscle spasms and strengthen the muscular-ligamentous apparatus. The exercises must be performed daily and repeated each 10 times.
An approximate set of exercises might look like this:
- Post-traumatic arthrosis of the knee joint according to ICD 10
- performing flexion-extension movements with the toes, sitting or lying down;
- performing foot stretches towards yourself and away from you, sitting or lying down;
- turning the foot alternately outward and inward;
- performing circular movements with the feet clockwise and counterclockwise, etc.
Swimming and water aerobics are considered quite effective. You can avoid the disease if you constantly pay due attention to the safety of the lower extremities, avoid injuring them, use comfortable shoes without heels for everyday life, engage in moderate exercise, and also eat right.
Expired - ArchiveSearch in current clinical protocols and materialsAlso: HS-014
RCHR (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan) Version: Archive - Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2007 (Order No. 764)
ICD categories: Other specified arthrosis (M19.8)
Post-traumatic arthrosis of other joints
ICD-10 International Classification of Diseases M00-M99 Diseases of the musculoskeletal system and connective tissue M00-M25 Arthropathy M15-M19 Arthrosis M19 Other arthrosis
M19.1
Post-traumatic arthrosis of other joints
Post-traumatic arthrosis OBD Diagnosis / disease Post-traumatic arthrosis of other joints Diagnosis / disease code M19.1 Standards of medical care for diagnosis / disease M19.1 See Full explanation of the ICD code M19.1: ICD code M19.1 / International Classification of Diseases / Diseases of the musculoskeletal system and connective tissue / Arthropathy / Arthrosis / Other arthrosis / Post-traumatic arthrosis of other joints
general information
Short description
Osteoarthritis (OA) is a chronic progressive degenerative joint disease characterized by degradation of articular cartilage with subsequent changes in the subchondral bone and the development of marginal osteophytes, leading to loss of cartilage and concomitant damage to other components of the joint (synovium, ligaments). Protocol code: HS-014 “Osteoarthrosis (polyarthrosis, coxarthrosis, gonarthrosis)” Profile: surgical Stage: hospital ICD-10 code(s): M15 Polyarthrosis M16 Coxarthrosis (arthrosis of the hip joint) M17 Gonarthrosis (arthrosis of the knee joint) M19 Other arthrosis
Cloud MIS "MedElement"
Clinic automation: fast and inexpensive!
- 290 clinics from 4 countries connected
- 1st place - 800 rubles / 4500 tenge per month.
- Registration + Cashier - 15,800 rubles / 79,000 tenge per year
Find out more+7 / +7 707 707 07 [email protected]
Cloud MIS "MedElement"
Clinic automation quickly and inexpensively!
290 clinics from 4 countries work with us- Connection of 1 workplace -
800 rub / 4500 tenge per month - Learn more about the system
+7 / +7 707 707 07 16 /
Classification
Classification by Nasonov V.A., Astapenko M.G., 1989. — primary (idiopathic); - secondary. - polyarthrosis; - oligoarthrosis; - monoarthrosis; - in combination with osteoarthritis of the spine, spondyloarthrosis. — interphalangeal joints (Heberden’s nodes, Bouchard’s nodes); - hip joints (coxarthrosis); — knee joints (gonarthrosis); - other joints. Synovitis: - present; - absent. — functional ability is limited (FN-1); — ability to work is lost (FN-2); - needs outside care (FN-3) (FN - functional failure).
Diagnostics
Diagnostic criteria Complaints and anamnesis: 1. Pain during physical activity and/or at rest, at night, when palpating the joint. 2. Stiffness in the affected joint in the morning or occurring after any rest, not exceeding 30 minutes. 3. Limitation of joint mobility or a feeling of instability in it. Physical examination: painful points in the places where the tendons attach to the joint capsules, crepitus and cracking in the joint when moving. Clinical features of individual forms of OA OA of the hip joint (coxarthrosis) is one of the most common variants of the disease. OA develops with equal frequency in men and women, but in women it is much more severe. It is noted that if coxarthrosis develops before the age of 40, it is usually associated with joint dysplasia (congenital acetabular dysplasia). The main symptoms of OA are mechanical pain in the joint area; gait disturbance (limping) occurs early on. In some cases, pain initially appears in the knee joint, groin, buttock, thigh, and lower back. The pain syndrome appears when walking and subsides with rest. The first clinical symptoms (pain, limited range of motion) appear in the absence of radiological changes in the joint; they are caused by muscle spasm. With bilateral damage, patients with coxarthrosis develop a “duck gait.” OA of the knee joint (gonarthrosis). The knee joint is the second most common location of deforming OA. Gonarthrosis usually affects women, which is facilitated by obesity and poor circulation in the lower extremities. The first symptoms usually appear between 40 and 50 years of age. The most common etiological factors in the development of the disease are poor posture and frequent trauma. As a rule, gonarthrosis is bilateral, but the patient complains of pain in one joint for a long time. With long-term gonarthrosis, a “blockade” of the joint may periodically occur, associated with the appearance of a “joint mouse” in the articular cavity. Damage to the knee joint can be complicated by osteonecrosis of the femoral condyle, this is observed with varus deviation. Instrumental studies: X-ray picture of joint damage, confirming the diagnosis - narrowing of the joint space until it disappears, bone growths along the edges of the articular surfaces, grossly deformed articular ends. List of main diagnostic measures: 1. X-ray examination of the joint. 2. Computed tomography of joints. 3. Nuclear magnetic resonance of joints. 4. Ultrasound of internal organs.
Online consultation with a doctor
Consult an experienced specialist without leaving your home!
Health consultation from 2500 tenge / 430 rubles
Interpretation of analysis and research results
- Arthrosis, unspecified (M19.9)
Second opinion regarding diagnosis, treatment
Choose a doctor
Signs and causes of the disease
Have you noticed any uncharacteristic sounds such as clicking, creaking or crunching in your knee when performing movements? Or maybe the leg in this section suddenly, after a simple walk or immediately after sleep, began to bother you with painful signs and/or stiffness? And after some time, did they go away on their own: in the first case - after rest, in the second - after 30-60 minutes, when the limbs had warmed up? But we ask all this for a reason, since these are the symptoms with a high degree of probability that can indicate gonarthrosis, at best stages 1-2.
The most important symptom of problems with the musculoskeletal system is pain. As long as it doesn't hurt, no one worries.
Important! If you do not pay attention to the problem in time, the pathological focus will reach an irreversible phase (stage 3-4), and conservative therapy will no longer be needed, you will have to undergo surgery. Often surgery is required already at stage 2, mainly for pathologies of rheumatoid origin.
So, if you have given an affirmative answer to at least one question, do not delay your visit to an orthopedic doctor and immediately undergo all the necessary examinations. After a thorough diagnosis, you will be individually prescribed the most effective treatment appropriate to the diagnosis. To make a diagnosis, it is usually sufficient to take an x-ray and test the biomechanical abilities of the knee area. Assessment of motor potential is carried out by performing certain movements of the limb with the help of a specialist and by the patient himself.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Treatment
Treatment tactics Treatment goals: reduction of functional joint insufficiency, correction of therapy. Non-drug treatment Algorithm for the treatment of osteoarthritis. Stage I: - physiotherapy (thermal procedures, hydrotherapy); — physical therapy (the main task is to reduce the load on the joint and strengthen the muscles): correction of posture and length of the lower extremities, exercises with isometric loads, exercises for individual muscle groups; - local analgesics and NSAIDs (ointment, gel, cream). Drug treatment Algorithm for the treatment of osteoarthritis. Stage II: - systemic NSAIDs (non-steroidal anti-inflammatory drugs) when signs of manifest osteoarthritis occur and when signs of inflammation appear; - oral and rectal NSAIDs - ibuprofen, diclofenac, ketoprofen, lornoxicam, priroxicam, celecoxib; - chondroprotectors; - for persistent synovitis - intra-articular administration of glucocorticoids. Stage III: - if conservative treatment is ineffective - orthopedic surgery: hip or knee replacement, arthroscopy with abrasive chondroplasty. 1. Local analgesics (drugs with irritating and distracting effects) - finalgon. 2. Local NSAIDs - diclofenac, ibuprofen, ketoprofen, piroxicam. 3. Systemic NSAIDs - diclofenac (100–150 mg/day), ibuprofen (1200–2400 mg/day), ketoprofen (200–300 mg/day), naproxen (500–100 mg/day), piroxicam (20 mg/day), lornoxicam (8–16 mg/day). 4. Specific COX-2 inhibitors: celecoxib (200–400 mg/day). 1. Chondroitin sulfate (500 mg 2 times a day). 2. Hyaluronic acid derivatives for intra-articular administration (3 weekly intra-articular injections). Preventive measures: prevention of joint injuries, timely, complete treatment of arthritis. Further management: - elimination of mechanical factors (wearing orthopedic shoes, a corset or support belt, using a cane); - weight loss; - unloading of the affected joint. List of essential medications: 1. *Ibuprofen 200 mg, 400 mg tablet. 2. *Diclofenac sodium 25 mg, 100 mg, 150 mg tablet. 3. Diclofenac sodium, emulgel 1% for external use 4. Diclofenac potassium 12.5 mg tablet. 5. Ketoprofen solution for injection 100 mg/2 ml, amp. 6. Lornoxicam 4 mg, 8 mg tablet. 7. Celecoxib 100 mg, 200 mg caps. 8. Naproxen 250 mg tablet. 9. Piroxicam 10 mg tablet. 10. Chondroitin sulfate 5%, ointment 11. Phosphaden 0.05 g tablet, 2% solution for injection, amp. 12. Pentoxifylline 100 mg, dragee, solution for injection 100 mg/5 ml amp. 13. *Nadroparin calcium - solution for injection in pre-filled syringes 2850 IU anti-Xa/0.3 ml; 3800 IU anti-Xa/0.4 ml; 5700 IU anti-Xa/0.6 ml; 7600 IU anti-Xa/0.8 ml, 9500 IU anti-Xa/1.0 ml Indicators of treatment effectiveness: reduction in functional joint failure.
* – drugs included in the list of essential (vital) medicines.
Hospitalization
Indications for hospitalization: severe pain, lack of effect of outpatient therapy, synovitis of the joint. The required scope of examinations before planned hospitalization: 1. X-ray of the affected segment and symmetrical joint in 2 projections. 2. General blood test (6 parameters). 3. General urine analysis. 4. Determination of C-reactive protein. 5. Reaction of Wright and Heddelson during joint production. 6. ECG. 7. Examination of stool for worm eggs. 8. Microreaction.
Information
Sources and literature
- Protocols for the diagnosis and treatment of diseases of the Ministry of Health of the Republic of Kazakhstan (Order No. 764 of December 28, 2007) 1. Nasonova V.A., Osteoarthrosis. 2001; 2. Drozdov V.N., Osteoarthrosis, 2004; 3. Nasonova V.A., Muravyov Yu.V., Tsvetkova E.S., Belenkiy A.G., Osteoarthritis of the knee joint, 2003; 4. Nasonova V.A., Nasonov E.L., Alekseeva L.I., Muravyov Yu.V., Osteoarthrosis of the hip joint, 2004; 5. Nasonova V.A., Modern view of the problem of osteoarthritis, 2004; 6. Povoroznyuk V.V., Osteoarthrosis: modern principles of treatment, 2003.
Information
Attached files
| 1. (HS-014-Osteoarthrosis__polyarthrosis,_coxarthrosis,_gonarthrosis.pdf) | read/download file |
Mobile application "MedElement"
- Professional medical reference books. Standards of treatment
- Communication with patients: online consultation, reviews, making an appointment
Download the application for ANDROID / for iOS
Mobile application "MedElement"
- Professional medical reference books
- Communication with patients: online consultation, reviews, making an appointment
Download the application for ANDROID / for iOS
Attention!
If you are not a medical professional:
- By self-medicating, you can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Guide” cannot and should not replace a face-to-face consultation with a doctor. Be sure to contact a medical facility if you have any illnesses or symptoms that concern you.
- The choice of medications and their dosage must be discussed with a specialist. Only a doctor can prescribe the right medicine and its dosage, taking into account the disease and condition of the patient’s body.
- The MedElement website and mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Directory” are exclusively information and reference resources. The information posted on this site should not be used to unauthorizedly change doctor's orders.
- The editors of MedElement are not responsible for any personal injury or property damage resulting from the use of this site.
In ICD-10, the term “Post-traumatic osteoarthritis” is considered a nosological synonym for the diagnosis Unspecified Arthrosis (M19.9).
Prevention and prognosis
To prevent the development of ankle arthrosis, you should eat a balanced and healthy diet, avoid injury and promptly treat any inflammatory diseases. Regular physical activity with an even distribution of effort is allowed.
It is impossible to completely get rid of arthrosis, but it is quite possible to achieve a long period of remission with the help of drugs and folk remedies. At the same time, do not forget to follow the rules of disease prevention and control your body weight. excess weight is an additional burden not only for joints, but also for the functioning of internal organs.
Reviews about the treatment of ankle arthrosis, see our video:
In ICD-10, the term “Post-traumatic osteoarthritis” is considered a nosological synonym for the diagnosis Unspecified Arthrosis (M19.9).
Active substances related to code M19.9
Below is a list of active substances related to ICD-10 code M19.9 (names of pharmacological groups and a list of trade names associated with this code).
- Active ingredients
- Aminophylline + Diphenhydramine + Indomethacin
Pharmacological group: NSAIDs - Acetic acid derivatives and related compounds in combination with other drugs - Amtolmetin guacil
Pharmacological group: NSAIDs - Acetic acid derivatives and related compounds - Bovhyaluronidase azoximer
Pharmacological group: Enzymes and antienzymes - Valdecoxib
Pharmacological group: NSAIDs - Coxibs - Hyaluronic acid
Pharmacological groups: Correctors of bone and cartilage tissue metabolism, Regenerants and reparants - Hydrocortisone
Pharmacological groups: Glucocorticosteroids, Ophthalmic drugs - Glucosamine + Chondroitin sulfate
Pharmacological group: Correctors of bone and cartilage metabolism in combination with other drugs - Dexamethasone
Pharmacological groups: Glucocorticosteroids, Ophthalmic drugs - Dexketoprofen
Pharmacological group: NSAIDs - Propionic acid derivatives - Diclofenac + Misoprostol
Pharmacological group: NSAIDs - Acetic acid derivatives and related compounds in combination with other drugs - Diclofenac + Pyridoxine + Thiamine + Cyanocobalamin
Pharmacological groups: Vitamins and vitamin-like drugs in combination with other drugs, NSAIDs - Acetic acid derivatives and related compounds in combination with other drugs - Dimethyl sulfoxide
Pharmacological group: Dermatotropic agents - Bile
Pharmacological group: Local irritants - Ibuprofen
Pharmacological group: NSAIDs - Propionic acid derivatives - Indomethacin
Pharmacological groups: Ophthalmic drugs, NSAIDs - Acetic acid derivatives and related compounds - Ketoprofen
Pharmacological group: NSAIDs - Propionic acid derivatives - Ketoprofen lysine salt
Pharmacological group: NSAIDs - Propionic acid derivatives - Cat's claw bark extract
Pharmacological group: General tonics and adaptogens - Lidocaine + Tolperisone
Pharmacological group: n-cholinergics (muscle relaxants) in combination with other drugs - Mabuprofen
Pharmacological group: Other non-narcotic analgesics, including non-steroidal and other anti-inflammatory drugs - Meloxicam
Pharmacological group: NSAIDs - Oxicams - Meloxicam + Chondroitin sulfate
Pharmacological groups: Correctors of bone and cartilage tissue metabolism in combination with other drugs, NSAIDs - Oxycams in combination with other drugs - Methylprednisolone
Pharmacological group: Glucocorticosteroids - Naproxen
Pharmacological group: NSAIDs - Propionic acid derivatives - Naproxen + Esomeprazole
Pharmacological groups: Proton pump inhibitors in combination with other drugs, NSAIDs - Propionic acid derivatives in combination with other drugs - Nimesulide
Pharmacological group: Other non-narcotic analgesics, including non-steroidal and other anti-inflammatory drugs - Niflumic acid
Pharmacological group: Other non-narcotic analgesics, including non-steroidal and other anti-inflammatory drugs - Capsicum fruit extract
Pharmacological group: Local irritants - Prednisolone
Pharmacological group: Glucocorticosteroids - Salicylamide
Pharmacological group: NSAIDs - Salicylic acid derivatives - Tenoxicam
Pharmacological group: NSAIDs - Oxicams - Tolperisone
Pharmacological group: Drugs affecting neuromuscular transmission - Tolperisone + Lidocaine
Pharmacological group: n-cholinergics (muscle relaxants) in combination with other drugs - Phenylbutazone
Pharmacological group: NSAIDs - Butylpyrazolidines - Celecoxib
Pharmacological group: NSAIDs - Coxibs - Etoricoxib
Pharmacological group: NSAIDs - Coxibs
All joint diseases are very diverse - each disease will develop in its own direction, having its own classification and symptoms. Arthrosis and arthritis of an infectious nature reduce the quality of life of each patient. I would like to pay special attention to and consider such a diagnosis as arthrosis of the ankle joint.
What it is?
Arthrosis of the ankle joint is a disease that provokes deformation of the joint itself and destruction of the structure of cartilage tissue, limiting or complete loss of mobility. The pathological process itself in medical circles is often called osteoarthritis - this is a destructive process, if the disease is accompanied by an inflammatory process - doctors talk about arthrosis.
The structure of the ankle joint
The diagnosis of arthrosis and arthropathy itself has several stages in its course:
- The first stage is the initial stage, when the disease is just beginning. Characterized by slight pain in the foot. But the cartilages of the lower leg and foot are not deformed at this stage.
- The second degree is marked by more severe attacks of pain and rapid fatigue during intense physical exertion; movement may be difficult. The patient may observe slight thickening and growth in the lower leg area of the bone, which was not previously observed. If treatment is not prescribed, the growth will grow and the pain will intensify and bother you throughout the day.
- With stage 3 arthrosis, the ankle itself becomes completely deformed, and foot movements become impossible and very difficult. It is when this degree of arthrosis is diagnosed that if the patient does not seek treatment, the patient is diagnosed with disability.
After a fracture or internal/external trauma, the patient develops post-traumatic arthrosis of the ankle joint. Along with this, the disease can also manifest itself after injury to the talus, as well as the tibia of the ankle itself.
The surface of the bone becomes deformed and uneven, and a pathological tumor forms on the joint itself.
Causes
Before dealing with the treatment of ankle arthrosis, it is worth understanding what causes the pathological process.
Reasons that provoke pathology:
- Prolonged stress on the joint itself - standing work or excessive participation in sports - leads to the development of arthrosis. If you do not occupy yourself with the issue of proper rest, the pathological process will cause disability.
- If you are overweight. In this case, the body mass index should not exceed 21-25 points - extra pounds put stress on the joint, leading to its destruction and deformation.
- Trauma and surgery on a joint can cause the development of pathology.
- Wearing uncomfortable shoes, high platforms and heels provokes the appearance of arthrosis.
- An inflammatory process occurring in the joint, as well as a hereditary, congenital pathology in the structure of the musculoskeletal system itself.
- A number of diseases that can indirectly “help” the development of arthrosis are diabetes mellitus and malfunction of the thyroid gland, gout.
- Anomalies in the structure and function of blood vessels - a failure in the blood supply will lead to an insufficient supply of nutrients to the joint, causing its destruction and deformation.
We recommend reading this article: “Rheumatoid arthritis of the ankle: important information.”
Causes of pseudarthrosis pathology
Congenital pseudarthrosis is formed for the following reasons:
- intoxication;
- rickets;
- tumors;
- endocrine disorders.
Among all cases of pseudarthrosis, congenital pathologies account for up to 4%. The remaining 96% falls to the share of acquired ones. Their main reasons:
- errors during bone surgery - incorrect fixation, resection of fragments;
- improper short-term rehabilitation - early removal of the fixation device, excessive load during the recovery period;
- suppuration and infection.
At the Ladisten Center for Modern Medicine and Traumatology, they conduct thorough diagnostics and correct the consequences of surgical errors.
Symptoms
When ankle arthrosis is affected, each stage of the pathological process has its own symptoms.
Symptoms of the pathology by stage are as follows:
- Symptom of the first stage. Rapid fatigue of the affected leg and foot, minor pain will increase with physical activity and go away at rest. There will be a crunching sound when the ankle is flexed, and x-rays will clearly show a narrowing of the joint space due to the destruction of cartilage.
- At the second stage of the pathological process, the pain becomes severe and goes away with long rest, all movements in the area of the affected joint are limited, and the muscles around it also become deformed in the absence of treatment. In the photographs, the radiologist can discern a narrowing of the joint gap by 2-3 times the norm, and a crunching sound can be clearly heard when moving.
- At stage 3 of the pathological process, the mobility of the lower leg and joint is severely limited, the person can only swing the leg. The pain will remain even if there is no load on the leg, the joint is unstable, doctors diagnose a complete narrowing of the gap between the bones.
In the absence of timely treatment, the quality of life decreases, movements are limited, up to the establishment of one or another disability group.
Factors provoking pathology
If a person’s general health status is good, he leads a healthy lifestyle, usually his joints function well and are not bothered day after day with or without painful sensations, even in old age. Otherwise, degenerative changes may arise that will begin to aggressively destroy important articular components that provide motor, support and shock-absorbing functions of the lower extremities at any age.
This is a real photo of the surface of the knee joint with gonarthrosis. Pay attention to damage that should not be there, the cartilage should be smooth as glass.
It is the progressive destructive processes in the knee joint that are commonly called gonarthrosis in medicine. It leads to the death of hyaline cartilage, which covers all surfaces of the articular bones, and as it becomes thinner and fibered, it leads to exposure and deformation of the latter and, as a consequence, to an extreme decrease in the quality of life.
An astroscope view of the destroyed cartilaginous surface in the joint cavity.
Arthrosis pathogenesis is often secondary, that is, when it becomes a consequence of certain pathologies, injuries, increased physical activity, etc. Anatomical and functional changes, as we have found out, mainly develop and become more complicated due to various negative factors. Among them, the most common ones are:
- congenital anomalies of the joints of the limbs (shortening of one of the legs, dysplasia, O-shaped and X-shaped deformities of the lower leg, etc.);
- post-traumatic consequences (complications of bruises, fractures, dislocations, sprains, etc.);
- joint hypermobility (JHM);
- rheumatoid arthritis, systemic lupus erythematosus, gout and pseudogout;
- local chronic infections and inflammations;
- obesity and metabolic diseases;
- endocrine diseases, especially diabetes and hypothyroidism;
- hormonal imbalances during menopause;
- excessive physical activity on the lower limbs;
- lack of physical activity, physical inactivity;
- constant overload of the legs associated with professional activities (sports, weight lifting, etc.);
- sitting for long periods of time in incorrect positions, for example, with your legs tucked under you;
- vascular pathologies of the extremities, hypothermia.
By the way, age-related physiological changes in bones, cartilage, and muscles occur in everyone as the body ages. These components wear out over time, becoming weaker, less flexible and elastic. This is not a paradox, but a natural phenomenon provided by nature, which begins approximately from the period when a person crossed the forty-year mark. Normally, it develops at a very slow pace, so nothing globally terrible happens to the joints. But there is one “but”. If the wear and tear of biological tissues significantly dominates the processes of metabolism and cellular nutrition, which is observed with the above factors, the joint begins to be progressively damaged.
It is enough to provoke the disease even by starting abruptly, without preparation, to engage in physical exercise, which you have never done before. Often, in pursuit of health, older people decide to radically change their lifestyle, for example, start running in the morning. Unprepared knee joints, which, as we noted, have some deviations due to age, are easily injured, and micro-tears appear in their structures and nearby areas. Such traumatization at the micro level, especially in people of retirement age, entails the development of gonarthrosis, not to mention more serious injuries.
The knee and hip joints are most often affected. The picture shows the dynamics of destruction from left to right, from the complete absence of the disease to the last stage.
The disease can develop not only in the older generation (after 40 years or more), but also in young people 25-40 years old. Periods of mature and old age certainly provide more chances for complex pathology, because the natural elements of the joint are no longer as strong as they were before. In addition, women have a greater predisposition to pathomorphological phenomena in the joint, which is mainly explained by the hormonal characteristics of the female body.
Diagnostics
To make an accurate diagnosis, doctors resort to different diagnostic methods.
Diagnostics is complex and consists of the following stages:
- Carrying out an inspection. This diagnostic method does not require preliminary preparation from the patient and during examination the doctor can identify the first symptoms of pathology. This is a local increase in body temperature and hypertrophy of the periarticular muscles, the skin takes on a thinner appearance. During palpation, the patient may feel pain even from the slightest touch. In advanced forms of arthrosis, deformation of the joint and destruction of cartilage are visible to the naked eye.
- Laboratory research. In this case, doctors take a blood test for examination. With the development of inflammation of the inner lining of the joint, when the synovial fluid is affected, the level of ESR in the blood increases, and the indicators of seroreactive protein and globulin compounds change slightly upward. Preparation for taking a blood test is standard - do not eat anything for 12 hours, drink is allowed, stop taking medications for 2 days, if this is not possible, inform the doctor. It is also prohibited to drink alcohol 1-2 days in advance, and minimize any physical activity.
- Instrumental research methods. Most often, in this case, doctors resort to diagnostics using X-rays, as well as using MRI or CT equipment. In some cases, doctors can also use the arthroscopy method - this is an examination of the joint cavity using an endoscope.
These methods do not require special preparation - just remove clothes, shoes, and jewelry.
Images may show the growth of osteophytes, as well as pathological narrowing of the joint space and hardening of bone tissue. In each case, the doctor interprets the data obtained taking into account the cause and stage of the pathological process.
Diagnosis of pseudarthrosis
To accurately diagnose a pseudarthrosis, clinical recommendations call x-rays the main method. Pictures must be taken in frontal and lateral projections.
The main sign: there is no bone callus on the x-ray. The ends of the bone fragments are smoothed and rounded, the cavity at the level of the medullary canal is closed.
When diagnosing, the 1976 classification according to Weber-Cech is used.
Classification of false joints²:
- hypertrophic. The ends of the bone fragments are thickened;
- atrophic. The ends of the fragments are conical;
- true. The end of fragments of different shapes. One is convex, the other is concave.
Treatment
Treatment of ankle arthrosis involves an integrated approach. This includes drug therapy, traditional medicine, massage and exercise therapy. It is important to remember that positive results of therapy will show if treatment is started in a timely manner. Otherwise, the patient faces restriction of movement and complete destruction of the joint, ankle cartilage, and disability.
Medication
Drug therapy is characterized by an integrated approach and involves the prescription of a number of drugs, taking into account the course of the pathological process.
The course of drug therapy includes:
- In order to relieve pain and relieve inflammation, non-steroidal anti-inflammatory drugs are prescribed. Most often, doctors prescribe Ibuprofen, Diclofenac, Flurbiprofen - all drugs can be in the form of tablets, injections, or ointments.
- In order to normalize the natural production of synovial fluid in the joint and improve the general condition of cartilage tissue, chondroprotectors are prescribed - Dune, Artra, Chondrolon, Structum. The course of therapy can vary from 1 to 3 months when taking tablets and 14-21 days when injections are given into the joint.
- To relieve inflammation and pain, doctors prescribe injections of drugs from the group of corticosteroid hormones. On average, 3-5 injections are given over 7-14 days.
- In order to improve joint mobility and blood flow, nutrition of cartilage, a course of laser irradiation and sessions of magnetic therapy, ultrasound or electrophoresis with medications are prescribed.
In the absence of positive dynamics from a course of drug therapy or in the case of a severe degree of destruction of the joint and cartilage tissue, surgical intervention and installation of artificial prostheses are practiced.
ethnoscience
In addition to traditional therapy, many doctors and herbalists recommend using recipes from the arsenal of traditional medicine. On their own, they will not have a pronounced effect, but as a supplement they will enhance the effect of tablets and injections, massage and exercise therapy.
We recommend you read an interesting article: “How to treat arthrosis of the ankle joint at home?”
The course of traditional medicine provides the following recipes:
- Recipe based on mumiyo resin: Dissolve 0.5 g of mumiyo in a few drops of rose or tea tree oil and rub with gentle movements into the area of the affected joint. Wrap in plastic and a warm scarf, leaving overnight until morning.
- Potato-based lotions: Grate the raw root vegetable on a coarse grater, squeeze out the excess liquid and apply to the affected joint for half an hour.
- Decoction of comfrey herb Mix 1 glass of vegetable oil and the same amount of crushed comfrey plant - simmer everything over low heat, not allowing it to boil for 7-8 minutes. After removing from the stove, allow to cool and filter. Rub it into the affected joint 3-5 times throughout the day.
- Chicken egg shell You should add dried and crushed chicken egg shells to your food. The main thing is not to add more than 1 tsp per day.
All recipes are natural and safe, but in any case it is important to take into account the individual tolerance of a particular component and coordinate their use with your doctor.
Exercise therapy
Next, we will consider a set of exercises for grades 1 and 2 of the severity of arthrosis, since when diagnosing stage 3, any load, even within the framework of exercise therapy, is contraindicated.
| Exercise | Repeat number |
| Lie down on a flat floor and in this position, alternately move your toe toward you/away from you, replacing it with your heel. | In the first stage of arthrosis, you can perform 10-15 exercises on each leg; in the second stage, limit yourself to 5-10 repetitions |
| Rotate first with toe, then with heel clockwise/counterclockwise | At the first stage of arthrosis, 10-12 times in each direction will be enough; at the second stage, we reduce the widow's |
| Rotate the foot inward and outward—right and left | At the first stage, 10-15 turns will be enough, at the second we cut it in half |
| Sit on a chair, perform foot movements as when walking, alternately lifting the heel, moving to the toe | At the first stage of arthrosis, it is enough to perform 10–15 times, divided into 2 approaches. For the second degree of the pathological process, divide the number by two |
| Sit on a chair and use your toes to crumple the fabric. | At the first stage, 10-15 times on each leg is enough, at the second stage, divide the number in half |
| We practice walking - first on the outside of the foot, then on the inside | 2-3 minutes on each side. This exercise is carried out only in the first stage of ankle arthrosis. |
| Heel-to-toe rolls - you can place a soft roller under your feet, which will enhance the effectiveness of the exercise due to a slight massage effect | Carry out 2-3 approaches, no more than 10 times per approach |
The main thing is to carry out all the exercises constantly, and if they cause pain, stop them immediately. Each exercise should be agreed upon in advance with your doctor.
Massage
Massage is practiced when diagnosing arthrosis of the ankle joint only at the first and second stages of the pathological process; at the third stage, massage, like exercise therapy, is prohibited.
At the very beginning, the massage session begins with warming up the legs, after placing a soft roller under the Achilles tendon. After warming up, proceed to rubbing with light massaging movements - straight or transverse rubbing, performing each of them no more than 2-4 times. The massage ends with concentric stroking. Each movement starts from the bottom and moves up to the calves, moving through the Achilles tendon.
Bibliography:
- https://moinogi.ru/artroz-golenostopnogo-sustava/
- https://diseases.medelement.com/disease/12767
- https://medum.ru/mkb-posttravmaticheskij-osteoartroz
- https://sustavzone.ru/sustavi/artroz/artroz-golenostopnogo-sustava