Joints
Discontinuous connections of bones are also called synovial joints, cavitary joints or joints. The joint has its own specific design, location in the body and performs certain functions.
In each joint, basic elements and accessory formations are distinguished. The main elements of the joint include: the articular surfaces of the connecting bones, the articular capsule (capsule) and the articular cavity. See the description of polymer concrete drainage trays on the website.
The articular surfaces of connecting bones must correspond to each other in shape to a certain extent. If the surface of one bone is convex, then the surface of the other is somewhat concave. The articular surfaces are usually covered with hyaline cartilage, which reduces friction, facilitates the sliding of bones during movements, acts as a shock absorber and prevents fusion of bones. The thickness of the cartilage is 0.2-4 mm. In joints with limited mobility, the articular surfaces are covered with fibrocartilage (sacroiliac joint).
The joint capsule is a connective tissue membrane that hermetically surrounds the articular surfaces of the bones. It has two layers: the outer - fibrous (very dense, strong) and the inner - synovial (on the side of the joint cavity it is covered with a layer of endothelial cells that produce synovial fluid).
The joint cavity is a small gap between the connecting bones, filled with synovial fluid, which, by wetting the surfaces of the connecting bones, reduces friction, the force of adhesion of molecules to the surfaces of the bones strengthens the joints, and also softens shocks.
Additional formations are formed as a result of functional requirements, as a reaction to an increase and specificity of the load. Additional formations include intra-articular cartilage: discs, menisci, articular lips, ligaments, outgrowths of the synovial membrane in the form of folds, villi. They are shock absorbers, improve the congruence of the surfaces of connecting bones, increase mobility and variety of movements, and contribute to a more even distribution of pressure from one bone to another.
Discs are solid cartilaginous formations located inside the joint (in the temporomandibular joint); menisci have the shape of crescents (in the knee joint); lips in the form of a cartilaginous rim surround the articular surface (near the glenoid cavity of the scapula); ligaments are bundles of connective tissue that go from one bone to another; they not only inhibit movements, but also direct them, and also strengthen the joint capsule; outgrowths of the synovial membrane are folds protruding into the joint cavity, villi filled with fat.
The joint capsule, ligaments, muscles surrounding the joint, atmospheric pressure (negative pressure inside the joint) and the adhesion force of synovial fluid molecules are all factors that strengthen joints.
Joints perform mainly three functions: they help maintain the position of the body and its individual parts, they participate in the movement of parts of the body in relation to each other, and, finally, they participate in locomotion - the movement of the entire body in space. These functions are determined by the action of active forces - muscles. Depending on the nature of muscle activity in the process of evolution, compounds of various shapes and having different functions were formed.
Classification of joints
Based on the number of connecting bones, joints are divided into simple and complex. In simple joints, only two bones are connected, in complex joints - three or more.
According to the shape of the articular surfaces, there are spherical (with a variety - nut-shaped joint), ellipsoidal, saddle-shaped, cylindrical, block-shaped and flat joints.
By the number of axes of rotation - triaxial with three axes of rotation, biaxial with two axes of rotation and single axis with one axis of rotation. Triaxial joints include spherical and nut-shaped, biaxial joints include ellipsoidal and saddle-shaped, and odoxial joints include block-shaped and cylindrical.
Flat joints do not have axes of rotation; only a slight sliding of the bones relative to each other is possible in them. The more axes of rotation in a joint, the greater the mobility and variety of movements, but the less strength and durability.
There are also combined and two-chamber joints. Two or more independent joints, movements in which occur simultaneously, are called combined. The cavity of two-chamber joints is divided by intra-articular cartilage (cartilage) into two parts (chambers).
BONE CONNECTION (ARTHROLOGY)
Bone connections can be continuous or discontinuous. Continuous (synarthroses) are earlier in development and immobile (or semi-mobile) in function. Diarthrosis, or discontinuous joints, appear much later in the development process and are mobile in function. Between these forms there is a transitional form - a symphysis or half-joint, characterized by the presence of a small gap and not having the structure of a real joint.
According to the nature of the tissue connecting the bones, synarthrosis is divided into syndesmosis, synchondrosis and synostosis.
Syndesmosis is a joint in which connective tissue remains between the bones after birth. These include interosseous membranes, ligaments and sutures. Interosseous membranes are connective tissue that fills large spaces between bones (between the bones of the forearm or lower leg). The connective tissue of the ligaments acquires the structure of fibrous bundles (ligaments between the processes of the vertebrae). At sutures, connective tissue is a thin layer between the bones of the skull. Based on the shape of the edges of the connecting bones, a serrated suture is distinguished, in which the teeth along the edge of one bone fit into the spaces between the teeth of another (between the bones of the cranial vault), a scaly suture, in which the edge of one bone overlaps the edge of the other (between the temporal and parietal bones) and a flat suture. , having a tight fit of non-serrated edges (between the bones of the facial skull).
Synchondrosis is characterized by the transition in the spaces between the bones after the birth of connective tissue into cartilaginous tissue, the bones are connected by cartilage. Based on the properties of cartilage tissue, synchondrosis is divided into hyaline (between the first rib and sternum) and fibrous (between the vertebral bodies). According to the duration of their existence, synchondrosis can be temporary or permanent. Temporary ones exist only up to a certain age, and then are replaced by synostoses (between the three bones of the lower limb girdle, merging into a single pelvic bone). Constants exist throughout a person’s life (between the pyramid of the temporal bone and the sphenoid bone, between the pyramid and the occipital bone).
Synostosis and diaphyses of tubular bones, bones of the base of the skull, pelvic bones).
Discontinuous joints or diarthrosis are movable joints that participate in the movement of body parts relative to each other and are organs of movement of the body in space. According to the number of articular surfaces, diarthrosis is divided into: a simple joint, which has 2 articular surfaces (interphalangeal); complex, having more than two articular surfaces (ulna); complex, containing intra-articular cartilage, which divides the joint into 2 chambers (knee); combined, consisting of several joints isolated from each other, located separately from each other, but functioning together (two temporomandibular joints).
Based on the shape and function of the joints, there are uni-, bi- and multi-axial joints. Uniaxial ones perform the functions of flexion, extension, and rotation. They are cylindrical (radial and ulnar joints) and trochlear (interphalangeal joint). Biaxial muscles perform the functions of flexion and extension, rotation, abduction and adduction. These include: ellipsoid (wrist joint), condylar (knee joint) and saddle (carpometacarpal joint of 1 finger). Multi-axis joints are characterized by all the functions described above and, in addition, circular motion. These include the spherical (shoulder) and flat (between the processes of the thoracic vertebrae) joints.
Regardless of the type, any joint has a similar anatomical structure. The joint includes the epiphyses of two bones, the articular surfaces of which are covered with articular cartilage, hyaline or fibrous, 0.2-0.5 mm thick. Articular cartilage facilitates the sliding of articular surfaces, softens shocks and serves as a buffer. The articular surface of the epiphysis of one bone is convex (has an articular head), the articular surface of the epiphysis of the other bone is concave (glenoid cavity). The articular capsule hermetically surrounds the articular cavity and adheres to the articulating bones. It consists of an outer fibrous layer, which performs a protective function, and an inner synovial layer, the cells of which secrete sticky transparent synovial fluid into the joint cavity - synovium, which reduces friction of the articular surfaces. In addition, synovium plays a role in fluid exchange and in strengthening the joint, serving as a buffer that softens compression and shock of the articular surfaces. From above, ligaments and tendons of muscles, which form an auxiliary apparatus for strengthening the joint, approach the joint capsule.
SCULL
The skeleton of the head is made up of paired and unpaired bones, which together are called the skull (cranium) (Fig. 1-6). Some skull bones are spongy, others are flat and mixed.
There are two sections in the skull, different in development and function. The cranium (neurocranium) forms a cavity for the brain and some sensory organs. It consists of a vault (calvaria) and a base (basis). The facial skull (viscerocranium) is the seat of most of the sensory organs and the initial sections of the respiratory and digestive systems.
The brain skull consists of 8 bones: paired - parietal and temporal, as well as unpaired - occipital, frontal, sphenoid and ethmoid. The facial skull includes 13 bones, of which the lower jaw, vomer and hyoid bones are unpaired, and the upper jaw, zygomatic, palatine, lacrimal, nasal and inferior turbinate are paired.
The bones of the skull have a number of features. In the bones of the brain skull, which make up its vault, there are outer and inner plates of the compact substance and a spongy substance located between them, called diploe (see Fig. 5, inset). It is penetrated by diploic canals containing diploic veins. The outer plate of the vault (lamina externa) is smooth, covered with periosteum. The periosteum for the internal plate (lamina interna) is the dura mater of the brain. The inner plate of the skull bones is thin, contains a lot of inorganic and little organic substances, so it is fragile and brittle. In case of skull injuries, its fracture occurs more often than a fracture of the outer plate.
Rice. 1. Skull, front view (facial norm):
1 - frontal bone; 2 - parietal bone; 3 - sphenoid bone; 4 - temporal bone; 5 - zygomatic bone; 6 - ethmoid bone; 7 - lacrimal bone; 8 - nasal bone; 9 - left upper jaw; 10 - lower jaw; 11 - inferior nasal concha; 12 — opener
Rice. 2. Skull, side view (lateral norm):
1 - parietal bone; 2 - frontal bone; 3 - ethmoid bone; 4 - lacrimal bone; 5 - nasal bone; 6 - right upper jaw; 7 - zygomatic bone; 8 - lower jaw; 9 - sphenoid bone; 10 - temporal bone; 11 - occipital bone
The periosteum of the skull bones fuses tightly with the bones in the area of the sutures, and throughout the rest of the length it connects loosely with the bones and limits the subperiosteal cellular space within one bone. In this space, ulcers and hematomas may occur.
The inner surface of the bones of the brain skull contains depressions and elevations corresponding to the convolutions and grooves of the brain, as well as branched grooves - a trace of the contact of the vessels and sinuses of the dura mater of the brain to the bones of the skull. In some places the skull has openings that serve for the passage of emissary veins connecting the venous sinuses of the dura mater of the brain, diploic and external veins of the head. The largest of these foramina are the parietal and mastoid. Some bones of the skull: the frontal, ethmoid, sphenoid, temporal and maxilla contain cavities lined with mucous membrane and filled with air. These bones are called air-bearing bones.
Rice. 3. Skull, occipital normal view:
1 - right parietal bone; 2 - occipital bone; 3 - right temporal bone; 4 - sphenoid bone; 5 - palatine bone; 6 - upper jaws; 7 - lower jaw
Rice. 4. Skull in a vertical normal:
1 - nasal bones; 2 - frontal bone; 3 - right parietal bone; 4 - occipital bone; 5 - left zygomatic bone
Rice. 5. Skull, sagittal cut:
1 - right parietal bone; 2 - occipital bone; 3 - right temporal bone; 4 - sphenoid bone; 5 - opener; 6 - right palatine bone; 7 - lower jaw; 8 - right upper jaw; 9 - right inferior nasal concha; 10 — right nasal bone; 11 - ethmoid bone; 12 - frontal bone. Inset - spongy substance of the bones of the cranial vault - diploe
Rice. 6. Skull in basal norm:
1 - upper jaws; 2 - palatine bones; 3 — left zygomatic bone; 4 - sphenoid bone; 5 - occipital bone; 6 - right temporal bone; 7 – opener
Synovial joints (joints)
Rice.
217. Synovial joints (joints). Types of joints by shape and number of axes of rotation. Uniaxial joints; 1a, 1b – trochlear joints, ginglymus (a – articulatio talocruralis; b – articulatio interphalangea manus); 1c – cylindrical joint, articulatio trochoidea (articulatio radioulnaris proximalis). Biaxial joints: 2a – elliptical joint, articulatio ellipsoidea (articulatio radiocarpea); 2b – condylar joint (articulatio genus); 2c – saddle joint, articulatio sellaris (articulatio carpometacarpea pollicis).
Triaxial joints: 3a – spherical joint, articulatio spheroidea (articulatio humeri); 3b – cup-shaped joint, articulatio cotylica (articulatio coxae); 3c – flat joint, articulatio plana (articulatio sacroiliaca).
Discontinuous connections of bones - joints, or synovial joints, articulationes synoviales (Fig. 217), are the most common type of articulation of human bones, creating conditions for high mobility of the body.
A joint is called simple, articulatio simplex, if two bones are involved in its formation, and complex, articulatio composita, if it is formed by three or more bones.
Each joint has obligatory structural elements, without which the connection of bones cannot be classified as joints, and auxiliary formations that determine the structural and functional differences of one joint from others.
Required elements of joints
The obligatory elements of the joint include articular cartilage, covering the articular surfaces; articular capsule and articular cavity.
Articular cartilage, cartilago articulares, is usually built from hyaline cartilage, less often fibrous.
These cartilages cover the surfaces of the bones that face each other when the articulating bones face each other. Consequently, one surface of the articular cartilage is fused with the bone surface it covers, and the other is free to stand in the joint.
The articular capsule, capsula articularis, surrounds the articulating ends of the bones in the form of a closed case and, without moving onto the articular surfaces, continues into the periosteum of these bones.
The capsule is built from fibrous connective tissue and consists of two layers - membranes. The outer, fibrous membrane, membrana fibrosa (stratum fibrosum), is built from dense fibrous connective tissue and plays a mechanical role. From the inside, it passes into the synovial membrane, membrana synovialis (stratum synoviale).
The synovial membrane forms synovial folds, plicae synoviales. This membrane secretes synovial fluid (synovia) into the joint, which wets the articular surfaces of the bones, nourishes the articular cartilage, acts as a shock absorber, and also changes the mobility of the joint as its viscosity changes.
The working surface of the membrane increases not only due to synovial folds, but also due to synovial villi, vilii synoviales, facing the articular cavity.
The articular cavity, cavitas articularis, is a narrow closed gap limited by the articulating surfaces of the bones and the articular capsule and filled with synovial fluid. The cavity has no communication with the atmosphere.
Discontinuous bone connections - diarthrosis
Discontinuous connections of bones - joints (juncturae synovialis), or synovial joints, diarthrosis - were formed from continuous connections and are the most progressive form of bone connection. Each joint has the following components: articular surfaces covered with articular cartilage; articular capsule, covering the articular ends of bones and strengthened by ligaments; the articular cavity located between the articulating surfaces of the bones and surrounded by the articular capsule, and the articular ligaments that strengthen the joint (Fig. 1).
The articular surfaces (facies articularis) are covered with articular cartilage (cartilago articularis). Typically, one of the articulating articular surfaces is convex, the other concave. The structure of cartilage can be hyaline or, less commonly, fibrous. The free surface of the cartilage, facing the joint cavity, is smooth, which facilitates the movement of bones relative to each other. The inner surface of the cartilage is firmly connected to the bone, through which it receives nutrition. The elasticity of hyaline cartilage softens shocks. In addition, cartilage smoothes out all the roughness of the articulating bones, giving them the appropriate shape and increasing the congruence (coincidence) of the articular surfaces.
The articular capsule (capsula articularis) covers the articular surfaces of the bones and forms a hermetically sealed articular cavity. The capsule consists of two layers: the outer - fibrous membrane (membrana fibrosa) and the inner - synovial membrane (membrana synovialis). The fibrous membrane is formed by fibrous connective tissue. In joints that perform extensive movements, the capsule is thinner than in inactive ones.
The synovial membrane consists of loose connective tissue, which is covered with a layer of epithelial cells. The synovial membrane forms special outgrowths - synovial villi (villi synoviales), involved in the production of synovial fluid (synovia). The latter moisturizes the articular surfaces, reducing their friction. In addition to villi, the synovial membrane has synovial folds (plicae synoviales), which extend into the joint cavity. Fat can be deposited in them, and then they are called fat folds (plicae adiposae). If the synovial membrane bulges outward, synovial bursae (bb. synoviales) are formed. They are located in areas of greatest friction, under muscles or tendons. In addition, in large joints the synovial membrane can form more or less closed cavities - recesses of the synovial membrane (recessus synoviales). Such inversions, for example, are found in the articular capsule of the knee joint.
The articular cavity (cavitas articularis) is a slit-like space limited by the articular surfaces of the bones and the articular capsule. It is filled with a small amount of synovial fluid. The shape and size of the articular cavity depend on the size of the articular surfaces and the attachment sites of the capsule.
In addition to the considered main components present in each joint, additional formations are observed: the articular lip, articular discs, menisci, ligaments and sesamoid bones.
The articular lip (labrum articulare) consists of fibrous tissue attached to the edge of the glenoid cavity. It increases the area of contact between the articular surfaces. For example, the labrum is present in the shoulder and hip joints.
The articular disc (discus articularis) and the articular meniscus (meniscus articularis) are fibrous cartilage located in the joint cavity. If the cartilage divides the joint cavity completely into 2 floors, which is observed, for example, in the temporomandibular joint, then they speak of a disc. If the division of the joint cavity is incomplete, then they speak of menisci: for example, menisci in the knee joint. Articular cartilage promotes congruence of articulating surfaces and reduces the impact of shocks.
Intracapsular ligaments (ligg. intracapsularia) consist of fibrous tissue and connect one bone to another. On the joint cavity side, they are covered by the synovial membrane of the joint capsule, which separates the ligament from the joint cavity: for example, the ligament of the femoral head in the hip joint. The ligaments that strengthen the articular capsule and lie in its thickness are called capsular (ligg. capsularia), and those located outside the capsule are called extracapsular (ligg. extracapsularia).
Sesamoid bones (ossa sesamoidea) are located in the joint capsule or in the thickness of the tendon. Their inner surface, facing the joint cavity, is covered with hyaline cartilage, the outer surface is fused with the fibrous layer of the capsule. An example of a sesamoid bone located in the capsule of the knee joint is the patella.
Rice. 1. Scheme of the joint structure:
1 - synovial membrane; synovial layer; 2 - fibrous membrane; fibrous layer; 3 - fat cells; 4 - articular capsule; 5 - hyaline articular cartilage; 6 - mineralized cartilage matrix; 7 - bone; 8 - blood vessels; 9 - articular cavity
Human anatomy. S. S. Mikhailov, A. V. Chukbar, A. G. Tsybulkin; edited by L. L. Kolesnikova.
Accessory formations of joints
Auxiliary formations of joints are varied.
These include ligaments, ligamenta; articular discs, disci articulares; articular menisci, menisci articulares; articular lips, labra articularia.
Joint ligaments are bundles of dense fibrous connective tissue that strengthen the joint capsule and limit or guide the movement of bones in the joint.
In relation to the articular capsule, extracapsular ligaments, ligg, are distinguished. extracapsularia, located outside the articular capsule, capsular ligaments, ligg. capsularia, located in the thickness of the capsule, between its fibrous and synovial membranes, and intracapsular ligaments, ligg. intracapsularia, inside the joint. Almost all joints have ligaments. Extracapsular ligaments are woven into the outer sections of the fibrous layer of the capsule; capsular ligaments are a thickening of this layer, and intracapsular ligaments are intra-articular in position, but are covered with a synovial membrane that separates them from the joint cavity.
Articular discs are layers of hyaline or fibrocartilage wedged between the articular surfaces of bones.
They are attached to the joint capsule and divide the articular cavity into two floors. Discs increase the correspondence (congruence) of the articular surfaces, and, consequently, the volume and variety of movements. In addition, they serve as shock absorbers, reducing shocks and shocks when moving.
Such discs are found, for example, in the sternoclavicular and temporomandibular joints.
Articular menisci, unlike discs, are not solid cartilaginous plates, but crescent-shaped formations of fibrous cartilage. Two menisci, right and left, are found in each knee joint; they are attached with their outer edge to the capsule, closer to the tibia, and with their sharp inner edge they stand freely in the joint cavity.
The menisci diversify movements in the joint and serve as shock absorbers.
The labrum is formed by dense fibrous connective tissue. It attaches to the edge of the glenoid cavity and deepens it, increasing the conformity of the surfaces.
The lip faces the joint cavity (shoulder and hip joints).
Discontinuous bone connections - diarthrosis
Discontinuous bone connections - diarthrosis
formed from continuous connections. During embryonic development, a syndesmosis is formed, which later differentiates into a joint.
Each joint, articulatio seu junctura synovialis, has the following components: 1) articular surfaces covered with cartilage; 2) an articular capsule, covering the articular ends of the bones and strengthened by ligaments; 3) the articular cavity, located between the articular surfaces of the bones and surrounded by the articular capsule.
1. Articular surfaces, faciei articulares, are covered with articular cartilage, cartilago articularis. Typically, one of the articulating articular surfaces is convex, the other concave. The structure of cartilage can be hyaline or, less commonly, fibrous. Their free surface, facing the joint cavity, is smooth, which facilitates the movement of the bones relative to each other. The inner surface of the cartilage is firmly connected to the bone, through which it receives nutrition. Convex articular surfaces, such as the heads of long tubular bones, are covered with a thicker layer of hyaline cartilage in the most convex central part, and thinner at the periphery. Accordingly, the articular cavities on the bones have a thinner layer of cartilage in the center, and a thicker one at the periphery. The thickness of articular cartilage ranges from 0.5 to 2-3 mm. The elasticity of hyaline cartilage softens shocks. In addition, cartilage smoothes out all the roughness of the articulating bones, giving them an appropriate shape in relation to each other and increasing the congruence (coincidence) of the articular surfaces.
2. The articular capsule, capsula articularis, covers the articular surfaces of the bones, attaching along their edge or slightly retreating from them and forming a hermetically closed articular cavity. It consists of two layers: the outer layer - the fibrous membrane, membrana fibrosa, and the inner layer - the synovial membrane, membrana synovialis. The outer fibrous layer consists of fibrous connective tissue, and the fibers on the surface of the layer run longitudinally, and in the depths - obliquely or transversely. In some places, the fibrous membrane becomes thinner, and then the joint capsule is formed only by the synovial membrane. In other parts, on the contrary, it is compacted and reaches significant thickness due to the external ligaments, which are woven into the outer fibrous layer of the capsule. In those places where muscles are adjacent to the capsule or tendons pass through, it is thinner, and in other places it is thicker. In joints with extensive movements, the capsule is thinner than in those with little movement. The synovial membrane consists of loose connective tissue, which is covered with a layer of epithelial cells of a cylindrical or polyhedral shape. It has two types of structure: smooth and folded. The synovial membrane ends at the edge of the articular cartilage, where there are special outgrowths - synovial villi, villi synoviales, involved in the formation of synovial fluid, synovia. The latter wets the articular surfaces, which ensures their adhesion.
The synovial membrane, in addition to the villi, has synovial folds, plicae synoviales, protruding into the joint cavity, in which fat can be deposited, and then they are called fat folds, plicae adiposae. In cases where the synosial membrane protrudes outward, synovial bursae, bursae synoviales, are formed. They are located in places of greatest friction: under muscles or tendons. In addition, in large joints the synovial membrane can form more or less closed cavities - inversions of the synovial membrane, recessus synoviales. A number of such inversions, for example, are present in the articular capsule of the knee joint.
3. The articular cavity, cavum articulare, is a slit-like space limited by the articular surfaces of the bones and the synovial membrane. It is filled with a small amount of synovial fluid. The shape and size of the articular cavity depend on the size of the articular surfaces and the attachment sites of the capsule.
In addition to the considered main parts present in each joint, there are additional elements: the articular labrum, intra-articular discs, menisci and ligaments, sesamoid bones.
The labrum, labrum glenoidale, consists of fibrous tissue attached to the edge of the glenoid cavity. It increases the area of contact between the articular surfaces. For example, the labrum is present in the shoulder and hip joints.
Articular discs, disci articulares, non-articular menisci, menisci articulares, are fibrous cartilage located in the joint cavity. If the cartilage divides the joint cavity completely into two floors, it is called a disc, as for example, this is observed in the temporomandibular joint. If the division of the joint cavity is incomplete, they speak of menisci, for example the menisci in the knee joint. Articular cartilages create greater congruence of the articulating surfaces and reduce the effect of shocks.
Intracapsular ligaments, ligg. intracapsularia, consist of fibrous tissue and connect one bone to another, located in the joint cavity, such as the circular ligament of the hip joint. The ligaments that strengthen the articular capsule are called extracapsular, ligg. extracapsularia.
Sesamoid bones, ossa sesamoidea, are located in the joint capsule or in the thickness of the tendon. Their inner surface, facing the joint cavity, is covered with hyaline cartilage, while the outer surface is fused with the fibrous layer of the capsule. An example of a sesamoid bone located in the capsule of the knee joint is the patella.
Differences in joint shape
Joints differ in the shape of the articular surfaces and the degree of mobility of the articulating bones. Based on the shape of the articular surfaces, the following are distinguished: spherical (cup-shaped) joints, articulationes spheroideae (cotylicae); flat, articulationes planae; ellipsoid, articulationes ellipsoideae (condylares); saddle-shaped, articulationes sellares; ovoids, articulationes ovoidales; cylindrical, articulationes trochoideae; block-shaped, ginglymus; condylar, articulationes bicondylares.
The nature of movement in the joint depends on the shape of the articular surfaces (see Fig. 217).
Ball-shaped and flat joints, in which the generatrix is represented by a segment of a circle, allow movement around three mutually perpendicular axes: frontal, anteroposterior (sagittal) and vertical. Thus, in the shoulder joint, spherical in shape, flexion (flexio) and extension (extensio) are possible around the frontal axis, while movement occurs in the sagittal plane; around the anteroposterior axis - abduction (abductio) and adduction (adductio), the movement occurs in the frontal plane.
Finally, rotation (rotatio) is possible around the vertical axis, including rotation inward (pronatio) and outward (supinatio), the rotation itself is carried out in the horizontal plane. These movements in flat joints are very limited (the flat articular surface in this case is considered as a small segment of a circle of large diameter), and in spherical joints the movements are performed with a large amplitude and are supplemented by circular motion (circumductio), in which the center of rotation corresponds to the spherical joint, and the moving bone describes the surface of the cone.
Joints in which movement around one of the three axes is excluded and only possible around two axes are called biaxial.
Biaxial joints include ellipsoid joints (for example, the wrist joint) and saddle joints (for example, the carpometacarpal joint of the first finger of the hand).
Cylindrical and trochlear joints are considered uniaxial. In a cylindrical joint, the generatrix moves parallel to the axis of rotation. An example of such a joint is the atlantoaxial median joint, the axis of rotation in which runs vertically through the tooth of the second cervical vertebra, as well as the proximal radioulnar joint.
A type of uniaxial joint is a trochlear joint, in which the generatrix is inclined relative to the axis of rotation (as if beveled).
These joints include the humeroulnar and interphalangeal joints.
Condylar joints, articulationes bicondylares, are modified elliptical joints.
In some joints of the skeletal system, movements are possible only simultaneously with movements in neighboring joints, i.e., anatomically isolated joints are united by a common function.
This functional combination of joints must be taken into account when studying their structure and analyzing the structure of movements.
Joints are movable joints of the bones of the skeleton with a gap between the articulating bones. A joint is a type of bone articulation; another type of articulation - a continuous connection of bones (without a joint space) - is called synarthrosis.
Joints perform both supporting and motor functions.
Rice. 1. Structure of the joint: 1 - articular cartilage; 2 - fibrous membrane of the joint capsule; 3 - synovial membrane; 4 - joint cavity; 5 - ends of articulating bones (epiphyses); 6 - periosteum.
Rice. 2. Types of hand joints:
1 - ellipsoidal; 2 - saddle-shaped; 3 - spherical; 4 - block-shaped.
The main elements of the joint are the articular surfaces (ends) of the connecting bones, the articular capsules, lined from the inside with the synovial membrane (see), and the articular cavities (Fig.
1). In addition to these main elements that form the joint, there are also auxiliary formations (ligaments, discs, menisci and synovial bursae), which are not found in all joints.
The ends of the articulating bones (epiphyses) form the solid base of the joint and, due to their structure, can withstand heavy loads. Hyaline cartilage, 0.5-2 mm thick, covering the articular surfaces and very firmly connected to the bone, ensures a more complete fit of the ends of the bones during movement and acts as a shock absorber in the supporting joints.
The articular capsule closes the joint cavity, attaching to the edges of the articular surfaces of the connecting bones.
The thickness of this capsule varies. In some joints it is tight, in others it is loose. There are two layers in the capsule: the inner synovial and the outer fibrous, consisting of dense connective tissue.
In a number of places, the fibrous layer forms thickenings - ligaments (see). Along with the ligaments that are part of the capsule, extra-articular and intra-articular ligaments also take part in strengthening the joints. The joints are further strengthened by the passing muscles and their tendons.
The joint cavity in the form of a slit contains a small amount of synovial fluid, which is produced by the synovial membrane and is a transparent, viscous yellowish liquid.
It serves as a lubricant for the articular surfaces, reducing friction during joint movements.
The auxiliary apparatus of the joint, along with ligaments, is represented by intra-articular cartilage (menisci, discs, articular labrum), which, located between the articular ends of the bones or along the edge of the joint, increase the area of contact of the epiphyses, make them more consistent with each other and play a large role in the mobility of the joints.
The blood supply to the joints occurs due to the branches of the nearest arteries; they form a dense network of anastomoses in the articular capsule.
The outflow of blood goes through the veins into nearby venous trunks. Lymphatic drainage occurs through a network of small lymphatic vessels into the nearest lymphatic collectors.
The innervation of the joints is provided by the spinal and sympathetic nerves.
The function of the joints is determined mainly by the shape of the articulating surfaces of the epiphyses of the bones.
The articular surface of one bone is like an imprint of another; in most cases, one surface is convex - the articular head, and the other concave - the articular cavity. These surfaces do not always completely correspond to each other; often the head has greater curvature and vastness than the cavity.
If two bones take part in the formation of a joint, then such a joint is called simple; if there are more bones - complex.
According to their shape, the articular surfaces of the bones are compared with geometric figures and, accordingly, joints are distinguished: spherical, ellipsoidal, trochlear, saddle-shaped, cylindrical, etc.
Type of bone connection: diarthrosis
Nature has endowed humans with the ability not only to move, but also to perform movements that other mammals are unable to perform. The coordinated work of 200 joints - movable bone joints - helps to perform complex actions. Some joints have limited movement, while others (true) are completely mobile. Joints and bones form the musculoskeletal system.
What is diarthrosis
True joints are freely movable joints of bone surfaces. If the connection is discontinuous, with a cavity between the bones, such a joint is classified as diarthrosis. This is a Greek word where “di” means day and “arthron” means division. The bones here are endowed with a wide range of motion.
This:
- elbow joint;
- knee;
- brachial;
- wrist joints.
Diarthrosis refers to synovial joints because the heads of the contacting bones are surrounded by an articular cavity. The inside is lined with a thin synovial membrane that produces up to 3 ml of lubricant - synovial viscous fluid. The heads of the bones in the capsule are covered with smooth hyaline cartilage. Cartilage reduces bone friction when moving and acts as a shock absorber during impacts. In the knee joint, additional shock absorption is added - semilunar cartilaginous plates, menisci, wedged between the surfaces of the bones of the joint. Some joints are equipped with discs that divide the internal cavity into 2 parts.
The heads of the bones of the joint coincide: with the convex part, paired with a concave surface. The outer membrane of the capsule strengthens the joint with band-like ligaments. The more difficult the load on the joint, the thicker these cords are. In addition, due to the ligaments, the joint does not make dangerous movements.
How are joints classified?
There are 4 types of joints: connection of bones without a gap - synarthrosis; diarthrosis - a discontinuous joint surrounded by a capsule, semi-joints - hemiarthrosis and symphysis - a discontinuous joint without an articular capsule (spine).
Diarthrosis refers to a common type of joint, which is divided into classes:
Cylindrical joints (ulna and radius) perform rotational movements in one direction and the other.
In the trochlear joint, elbow, knee and ankle, the limbs bend and extend. Perform circular movements, move left and right. The bones, muscles and ligaments of these joints are strong and durable.
Helical joints include the interphalangeal joints and the junction of the humerus and ulna. The groove inside the joint looks like a spiral.
In ellipsoidal joints, the smooth, convex surface of one bone slides over the smooth, concave surface of another bone (in the wrist joint).
The condylar joints are connected by a process, the condyle, to the socket. These are the knee joints, the connection between the atlas and the skull, and the temporal bone and lower jaw.
In the saddle joint, one surface on another allows the hand to be rotated around its own axis.
The ball, free and cup joints, shoulder and hip, are formed by a ball-like head of bone and a circular notch. The joint allows the limbs to move in 3 planes. But these places are more prone to fractures.
In flat joints, the surfaces of the bones only slide against each other.
In addition, joints differ in the number of surfaces and functions.
Common diseases of mobile joints and causes
People with healthy joints are now a rarity. Frequent complaints of patients: pain while walking, difficulty raising an arm or leg, difficulty turning or squatting. Diseases appear due to professional and accidental injuries, hypothermia, inflammatory processes or due to heredity. Moreover, in the hip and knee joints the disease is asymptomatic until it manifests itself as aching pain, difficulty moving and morning swelling. This indicates the irreversibility of the process.
The ankle joints suffer less. The risk group includes overweight people, lovers of flat soles and high heels. This group also includes older people, those who move little, “diabetics” and “chronic patients”.
More often than others, with age, the hip joints are affected. The cartilage layer becomes thinner, the bones become fragile. A lot of stress goes to the kneecaps. Due to heavy physical labor or sports activities, the ankle and shoulder joints suffer. Fine motor skills are impaired in the wrist joints.
Joint diseases are divided into congenital, when a child is born with a dislocated hip, and those that a person acquires. Diseases that destroy and deform joints are called arthrosis, and inflammation is called arthritis. Arthrosis includes:
- osteoarthritis of the hip, shoulder, knee and other joints;
- intervertebral osteochondrosis;
- glenohumeral periarthritis;
- spondylosis, osteochondropathy.
Arthritis occurs due to infection in the body, allergies and other diseases of other organs.
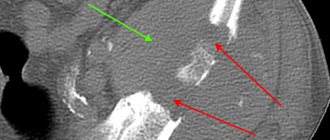
How to diagnose joint disease
If you experience pain and a suspicious crunch in the joint, stiffness after sleep, stretched skin around the sore spot, or swelling, you should undergo an examination. If this is not done in time, mobility in the joint will most likely be limited.
1. X-rays. Arthritis of the second degree: destruction of bone and cartilage tissue is visible. Third degree - the joint is deformed, the patient, at the same time, feels limited in movements.
The initial stage of arthrosis is determined by a slight reduction in the lumen between the cartilages, which have become thinner. Second degree: the inside of the joint capsule has decreased by 3 times, bone outgrowths or areas with dead cartilage have appeared. In the 3rd stage, irreversible deformations are visible, sometimes the bones grow together.
2. Ultrasound examination (ultrasound) helps to find the source of inflammation and growths or tumors.
3. Using computed tomography and magnetic resonance imaging, the condition of the soft tissues around the joint and, in fact, the joint itself is assessed.
4. Using osteoscintigraphy, the source of inflammation is found in order to eliminate it.
5. Large joints are examined with an arthroscope (microscopic camera).
Treatment of joints
In case of arthritis, soft tissues become inflamed, affecting changes in the cartilaginous layers, and are treated with non-steroidal anti-inflammatory and painkillers, corticosteroids and physiotherapy.
Arthrosis, osteoporosis and rheumatism are difficult to treat. Sometimes, it only works to eliminate the pain. As you age, cartilage tissue is produced more slowly. The friction of bone surfaces first destroys the cartilage, then the bone, the joint wears out, and this is how arthrosis appears. Treat with non-steroidal anti-inflammatory drugs, chondroprotectors and vasodilators.
With ankylosis, the joint becomes immobile because the bones have fused together. They are treated with gymnastics, massage, manual and physiotherapy. Medications include anti-inflammatory drugs, analgesics and hormones. If it doesn't help, surgery is required.
If the doctor has diagnosed periarthritis, when the periarticular tissues become inflamed, a fixing bandage and physiotherapy procedures with anesthesia are prescribed.
Gouty bumps, with crystals of uric acid salt, are located near the joint. The treatment is inpatient, so self-treatment is dangerous due to overdose.
Synovitis is inflammation of the inner lining of the joint capsule and excessive production of fluid. It is treated with dry heat and rest of the joint. Excess fluid is sometimes removed by puncture and rinsing.
Inflammation of the knee joints (gonarthrosis) requires treatment with anti-inflammatory and painkillers and drugs instead of synovial fluid. Walk with a cane and use orthotics.
Osteochondrosis destroys articular cartilage; cure is impossible. Only pain relief; if a hernia appears, surgery is prescribed.
How Valentin Dikul treats joints
Valentin Ivanovich Dikul is known as a doctor, doctor of medicine and developer of original methods for restoring patients after complex trauma. “Even an incurable joint can be restored with self-treatment and some effort,” says Dr. Dikul. He invented formal gymnastics, the effects of which he tested in his own treatment.
The first type of gymnastics, for 2 times daily, supports joints and develops muscles during recovery. The exercises of the second complex develop flexibility and elasticity of the ligaments. This complex is allowed for those patients whose joints have already been restored.
In addition to therapeutic exercises, Dikul studies medicinal homeopathic (natural) remedies and prepares healing compounds. Popular Dikul drugs cope with the treatment of bruises, sprains, treat arthrosis, osteoarthrosis, and radiculitis. The doctor's ointments relieve pain and relieve inflammation, restoring joint function.
Preventive measures
Prevention of arthrosis and arthritis is recommended for women over 45 years of age and men over 55.
Rules for preserving joints:
- Proper nutrition with vitamins, minerals and amino acids. Eat cartilage, jelly and jellied meat. Don't give up vegetables and dairy products.
- Make sure you maintain your own proper weight.
- Drink 1.5-2 liters of clean water per day.
- Avoid coffee, alcohol and cigarettes, products that wear out and dehydrate the body.
- Do morning exercises and afternoon warm-ups every day.
- Treat viral and infectious diseases in a timely manner.
- Perform therapeutic exercises and monitor correct posture.
Only a careful and attentive attitude towards your own health will help maintain the health of your joints.
Related posts:
- Tuberculosis of bones and joints
- Abortion: type and features
In each joint, basic elements and accessory formations are distinguished.
Movements can be carried out around one, two and three axes, forming one- (cylindrical and block-shaped), two- (ellipsoidal and saddle-shaped) and multi-axial (ball-and-socket) joints (Fig.
2). The number and position of axes determine the nature of the movements. There are movements around the frontal axis - flexion and extension, the sagittal axis - adduction and abduction, the longitudinal axis - rotation and multi-axis rotational movement.
1. Continuous
– synarthrosis – between the bones there is a layer that connects tissue. Motionless.
2. Semi-continuous
– hemiarthrosis (symphyses) – a small cavity with fluid
3. Intermittent
– diarthrosis (joints) of the bones are displaced relative to each other
All types of joints in the spinal column
Continuous connections : whether there is a gap or a cavity,
1. Fibrous compounds (syndesmoses) - ligaments (spreads from one bone to another), membranes - flat, wide, along the cord of bone - radius and ulna, hip joint - pelvic bone - obturator membrane - tibia and fibula; sutures - skulls - serrated suture, flat suture - facial bones, scaly suture - temporal region, impactions - attachment of teeth to the jaw; collagen - strength in the ligament, elastic fibers - mobility 2. Cartilaginous joints (synchodrosis) - permanent - sternum and 1 rib, intervertebral discs, temporary - pelvis - ischial, pubic, iliac, sacrum, places of attachment of the epiphysis and diaphysis 3. Bone joints ( synostosis) – replacement of temporary cartilaginous joints – fused sacrum
Intermittent connections
= joints.
mandatory and auxiliary elements. Mandatory: 1. The joint surfaces are in- and congruent, covered with hyaline cartilage - smoothes the bone tissue, as dense as the bone itself, it greatly facilitates movement in the joint. 2. The joint capsule is fibrous (protects the joint) and synovial membrane (rich in blood vessels, produces synovial fluid). 3. The articular cavity is a slit-like space between the articular surfaces and contains synovial fluid.
4. Synovial fluid - secreted by a membrane, with exfoliating cartilaginous and flat connective tissue cells form mucus, promotes adhesion, wetting, facilitating gliding
Semi-continuous = Half-joint – fibrous or cartilaginous joints. Symphysis pubis, manubrium sternum, intervertebral. There is no capsule, the inner surface of the fissure is not lined with synovial membrane. Can be strengthened by interosseous ligaments
10. Continuous bone connections.
Synovial joints (joints)
Classification. Examples.
Continuous connections: synarthrosis - between the bones there is a layer of tissue connecting. Fixed, no gap or cavity.
1. Fibrous compounds (syndesmoses) –
1.1. ligaments (spreads from one bone to another) - collagen fibers, low extensibility, very strong,
1.2. membranes – flat, wide, along the cord of bone – radius and ulna, hip joint – pelvic bone – obturator membrane – tibia and fibula;
sutures - skull - serrated suture, flat suture - facial bones, scaly suture - temporal and parietal regions, sutures - zones for shock absorption and shock absorption when walking, jumping. Also serve as areas for bone growth.
1.4. impaction – connection of the tooth root with the walls of the alveoli.
Cartilaginous joints (synchodrosis) are strong and elastic - permanent - sternum and 1 rib, intervertebral discs, temporary - pelvis - ischial, pubic, iliac, sacrum, attachment points of the epiphysis and diaphysis
3. Bone joints (synostoses) – replacement of temporary cartilaginous joints