Bone connections
Bones in the human body are not located isolated from each other, but are interconnected into one single whole. Moreover, the nature of their connection is determined by functional conditions: in some parts of the skeleton, movements between bones are more pronounced, in others - less. Even P.F. Lesgaft wrote that “in no other department of anatomy can one so “harmoniously” and consistently identify the connection between form and function” (function). By the shape of the connecting bones, you can determine the nature of the movement, and by the nature of the movements, you can imagine the shape of the joints.
The main point when connecting bones is that they “are connected to each other in such a way that, with the smallest volume of the junction, there is the greatest variety and magnitude of movements with the greatest possible strength in the most advantageous counteraction to the influence of shocks and shocks” (P. F. Lesgaft) .
The whole variety of bone connections can be represented in the form of three main types. There are continuous joints - synarthrosis, discontinuous - diarthrosis and semi-continuous - hemiarthrosis (half-joints).
Continuous connections
bones are those in which there is no break between the bones; they are connected by a continuous layer of tissue.
Intermittent connections
- these are those when there is a gap between the connecting bones - a cavity.
Semi-continuous connections
characterized by the fact that in the tissue, which is located between the connecting bones, there is a small cavity - a gap (2-3 mm) filled with liquid. However, this cavity does not completely separate the bones, and the essential elements of a discontinuous connection are missing. An example of this type of joint is the joint between the pubic bones.
Continuous bone connections are phylogenetically more ancient. The lower animals have exclusively continuous connections. In humans, most of the bones are discontinuous joints. This is the later, most advanced and most flexible type of joint, although less durable. Discontinuous connections occur from continuous ones through their gradual transformation.
The emergence of different types of bone joints can also be observed in human ontogenesis. Similar to the stages of bone development, the development of their joints occurs. In the early stages of skeletal formation, the bone rudiments are connected to each other only by embryonic connective tissue. Depending on the functional orientation, where there is no need for large-scale movements between the connecting bones, connective tissue remains, which can turn into cartilage to provide mobility and shock absorption, or into bone. This is how continuous connections are formed. Where greater mobility between bones is required, the connective tissue dissolves, creating a discontinuous connection, with a cavity between the bones. The cavity appears by the end of the 2nd month of embryonic life.
Functional characteristics of continuous bone connections
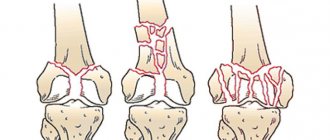
Depending on the nature of the tissue located between the connecting bones, connections are distinguished using the connective tissue itself (syndesmosis), cartilaginous (synchondrosis) and bone (synostosis) (see diagram and Fig. 23).
Rice. 23. Examples of fibrous bone joints: 1 - intervertebral disc (synchondrosis); 2 - serrated suture, fibrous connection (syndesmosis); 3 - synostosis; 4 - annular ligament - syndesmosis; 5 - interosseous membrane - syndesmosis; b - scaly suture - syndesmosis; 7 - flat seam - syndesmosis; 8 - pubic fusion (half-joint; 9 - connection of bones with the help of muscle (synzarcosis)
Syndesmoses.
If collagen fibers predominate in the connective tissue located between the bones, such connections are called fibrous, if elastic - elastic. Fibrous compounds, depending on the size of the layer, can be in the form of ligaments (between the processes of the vertebrae), in the form of membranes 3 - 4 cm wide (between the bones of the pelvis, forearm, lower leg) or in the form of sutures (between the bones of the skull), where the layer of connective tissue is only 2 - 3 mm. An example of continuous connections of the elastic type are the yellow ligaments of the spine, located between the vertebral arches.
Synchondroses.
Depending on the structure of the cartilage, these connections are divided into connections using fibrous cartilage (between the vertebral bodies) and connections using hyaline cartilage (costal arch, between the diaphysis and the epiphysis, between individual parts of the skull bones, etc.).
Cartilaginous connections can be temporary (connections of the sacrum with the coccyx, parts of the pelvic bone, etc.), which then turn into synostoses, and permanent, existing throughout life (synchondrosis between the temporal bone and the occipital bone).
Hyaline compounds are more elastic, but fragile compared to fibrous ones.
Synostosis.
These are connections of bones with bone tissue - ossification of epiphyseal cartilages, ossification of sutures between the bones of the skull.
Continuous bone connections (except synostoses) are mobile. The degree of mobility depends on the size of the tissue layer and its density. The actual connective tissue joints are more mobile, while the cartilaginous ones are less mobile. Continuous connections also have a pronounced property of shock absorption and shock absorption.
Functional characteristics of discontinuous bone connections
Discontinuous connections of bones are also called synovial joints, cavitary joints or joints. The joint has its own specific design, location in the body and performs certain functions.
In each joint, basic elements and accessory formations are distinguished. The main elements of the joint include: the articular surfaces of the connecting bones, the articular capsule (capsule) and the articular cavity (Fig. 24).
Rice. 24. Synovial joint - joint (diagram): 1 - articular ends of connecting bones; 2 - fibrous layer of the joint capsule; 3 - synovial layer of the articular capsule; 4 - articular cavity containing synovial fluid; 5 - articular cartilage; 6 - meniscus; 7 - intra-articular ligaments; 8 — inversions of the articular cavity
Articular surfaces
connecting bones must correspond to each other in shape to a certain extent. If the surface of one bone is convex, then the surface of the other is somewhat concave. The articular surfaces are usually covered with hyaline cartilage, which reduces friction, facilitates the sliding of bones during movements, acts as a shock absorber and prevents fusion of bones. The thickness of the cartilage is 0.2 - 4 mm. In joints with limited mobility, the articular surfaces are covered with fibrocartilage (sacroiliac joint).
Bursa
- This is a connective tissue membrane that hermetically surrounds the articular surfaces of the bones. It has two layers: the outer - fibrous (very dense, strong) and the inner - synovial (on the side of the joint cavity it is covered with a layer of endothelial cells that produce synovial fluid).
Articular cavity
- a small gap between the connecting bones, filled with synovial fluid, which, by wetting the surfaces of the connecting bones, reduces friction, the force of adhesion of molecules to the surfaces of the bones strengthens the joints, and also softens shocks.
Additional education
are formed as a result of functional requirements, as a reaction to increased and specific load. Additional formations include intra-articular cartilage: discs, menisci, articular lips, ligaments, outgrowths of the synovial membrane in the form of folds, villi. They are shock absorbers, improve the congruence of the surfaces of connecting bones, increase mobility and variety of movements, and contribute to a more even distribution of pressure from one bone to another. Discs are solid cartilaginous formations located inside the joint (in the temporomandibular joint); menisci have the shape of crescents (in the knee joint); lips in the form of a cartilaginous rim surround the articular surface (near the glenoid cavity of the scapula); ligaments are bundles of connective tissue that go from one bone to another; they not only inhibit movements, but also direct them, and also strengthen the joint capsule; outgrowths of the synovial membrane are folds protruding into the joint cavity, villi filled with fat.
The joint capsule, ligaments, muscles surrounding the joint, atmospheric pressure (negative pressure inside the joint) and the adhesion force of synovial fluid molecules are all factors that strengthen joints.
Joints perform mainly three functions: they help maintain the position of the body and its individual parts, they participate in the movement of parts of the body in relation to each other, and, finally, they participate in locomotion - the movement of the entire body in space. These functions are determined by the action of active forces - muscles. Depending on the nature of muscle activity in the process of evolution, compounds of various shapes and having different functions were formed.
Classification of joints.
Based on the number of connecting bones, joints are divided into simple and complex. In simple joints, only two bones are connected, in complex joints - three or more.
According to the shape of the articular surfaces, there are spherical (with a variety - nut-shaped joint), ellipsoidal, saddle-shaped, cylindrical, block-shaped and flat joints.
By the number of axes of rotation - three-axis with three axes of rotation, bi-axial - with two axes of rotation and single-axis - with one axis of rotation. Triaxial joints include spherical and nut-shaped, biaxial joints include ellipsoidal and saddle-shaped, and odoxial joints include block-shaped and cylindrical. Flat joints do not have axes of rotation; only a slight sliding of the bones relative to each other is possible in them. The more axes of rotation in a joint, the greater the mobility and variety of movements, but the less strength and durability. There are also combined and two-chamber joints. Two or more independent joints, movements in which occur simultaneously, are called combined. The cavity of two-chamber joints is divided by intra-articular cartilage (disc) into two parts (chambers).
Considering the articular surfaces of bones as geometric segments of a body of rotation, we can assume that the movements of the bones in the joints occur around the axes of rotation. The axis of rotation is the line mentally drawn through the center of the joint, around which one bone rotates in relation to the other. It should be remembered that movements in the joint occur perpendicular to the axis of rotation. There are three mutually perpendicular axes: transverse, or frontal, anteroposterior, or sagittal, and vertical. All movements in the joints are considered from the anatomical position of the body. Around the transverse axis of the limb region, flexion (when the angle between the connecting bones decreases) and extension (when the angle between them increases) is possible; in the head and torso area - bending forward and backward. Around the anterior-posterior axis in the limb region, abduction (movement from the midline of the body) and adduction (movement towards the midline of the body) are possible; in the area of the head and torso - bends to the sides (Fig. 25). Around the vertical axis in the area of the limbs, rotation outward is possible - supination and rotation inward - pronation, and in the area of the head and neck - rotation to the sides (torsion).
Rice. 25. Shape of joints and axis of rotation (scheme by M. F. Ivanitsky): 1 - spherical joint (shoulder), triaxial; 2 - nut-shaped joint (hip), triaxial; 3 - elliptical joint (radio-carpal), biaxial, 4 - saddle joint (carpometacarpal joint of the 1st finger), biaxial; 5 - trochlear joint (interphalangeal), uniaxial; 5a - complex joint (elbow), consisting of 3 joints (a - humeroradial - spherical, b - humeroulnar - trochlear, c - proximal radioulnar - cylindrical, uniaxial); 6 - cylindrical joints (proximal and distal radioulnar), combined; 7 - flat joints between the bones of the tarsus, without pronounced axes of rotation (a - scaphoid bone, b - internal sphenoid bone, c - intermediate sphenoid bone, d - external sphenoid bone, e - cuboid bone, f - metatarsal bones); 8 - screw-shaped joint (ankle-foot), uniaxial, functions as a trochlear joint
Ball joints
characterized by the fact that the surface of one of the connecting bones has the shape of a ball, while the surface of the other is somewhat concave. These joints have three mutually perpendicular axes of rotation. An example of a typical ball-and-socket joint is the shoulder. In the nut joint, the surfaces of the bones are very congruent, the head of one bone fits more than 1/2 into the glenoid cavity of the other bone. The axes of rotation here are the same as in the ball and socket joint, but the range of movements is much smaller.
Elliptical joints
have articular surfaces (both convex and concave) in the form of an ellipse. Movements in these joints occur around two axes of rotation - transverse (flexion and extension), and anteroposterior (abduction and adduction). Ellipse-shaped joints include: radiocarpal and atlanto-occipital.
In saddle-shaped
the surfaces of the connecting bones resemble part of the surface of the saddle. They also have two axes of rotation - transverse and anterior-posterior - with corresponding movements. An example of such a joint is the joint between the wrist and the 1st metacarpal bone. Here flexion is called opposition, and extension is called retraction. In ellipsoidal and saddle-shaped joints, small-scale circular movements are also possible.
Cylindrical joints
have articular surfaces in the form of segments of a cylinder, one of them convex, the other concave. Movements in them occur around a vertical axis running along the bone (the joint between the radius and ulna bones) - pronation and supination.
In block-shaped
the surface of one bone has a depression, and the surface of the second has a protrusion that guides the depression. These joints have only one axis of rotation - the transverse one, around which flexion and extension are possible. An example of a trochlear-shaped joint is the interphalangeal joint.
In flat
the articular surfaces of the bones correspond well to each other. Mobility in them is low (sacroiliac joint).
The shape of the joint is related to mobility, location of ligaments and muscles. In trochlear joints the ligaments are lateral, in spherical joints they are located more or less evenly around the joint. Muscle groups in uniaxial joints cross the axis of rotation almost at a right angle, in multiaxial joints - obliquely.
Mobility in the joints varies not only due to the different shape of the articular surfaces. It depends on their correspondence to each other, the state of the bursa-ligamentous apparatus and muscles, ambient temperature, age, gender, time of day, and the nature of the activity.
The more the connecting surfaces of the bones correspond to each other, the less mobility. The stronger, thicker the bursa and ligaments, the less extensible the muscles, the less mobility in the joints.
At high ambient temperatures, mobility is greater than at low ambient temperatures.
In the morning, mobility is less than in the evening, which is explained by stagnation of lymph in the tissues. Maximum mobility indicators are observed at 12 - 14 hours of the day. The younger the children, the greater the daily fluctuations in joint mobility. In athletes, these fluctuations are less pronounced.
Muscular activity increases mobility in the joints. However, the predominance of static loads can reduce it, which is associated with the strong development of antagonist muscles and thickening of ligaments that inhibit movement. There are also observations of the opposite nature, indicating that the development of muscle strength does not always limit mobility in the joints. For example, hockey players, compared to athletes of other specializations, have well-developed muscle strength and joint mobility in the joints of the lower limb.
The dynamic nature of the loads in sports helps to increase mobility in joints (volleyball, basketball, swimming, running), but in some joints mobility increases to a greater extent, in others to a lesser extent. Even in one joint there may be a fragmented increase in mobility, for example, flexion-extension mobility of the upper limb in skiers, pronator-supinator mobility of the forearm in tennis and volleyball players, hip abduction and adduction in breaststroke swimmers, etc.
In children, mobility in the joints is greater than in adults, due to the fact that in the former the size of the cartilage, layers of connective tissue, articular cavities are larger, the congruence of the articular surfaces is less, and the elasticity of the bursa-ligamentous apparatus is greater. With old age, mobility decreases due to a decrease in the elasticity of ligaments and muscles due to tissue dehydration, as well as due to the growth of bone tissue along the edges of connecting bones, which increases their congruence. In women, mobility in the joints is greater than in men (the tissue is more elastic, the tone of the muscles opposite to the movement is less pronounced).
A study of the development of mobility in bone joints was carried out in a wide age range (from 7 to 70 years) by B.V. Sermeev. It showed that age-related changes in mobility in individual joints occur differently. The mobility of the spinal column increases in primary and secondary school age, and then gradually decreases, especially after 50-60 years. The rate of increase in mobility of the spinal column during flexion and extension is higher than during lateral movements (bending to the side).
Mobility in the joints of the upper limb girdle and in the shoulder joint continuously increases until 12-13 years of age; until 16 years of age, mobility indicators remain at a high level, and then begin to decrease, especially sharply after 50 years of age.
In the elbow joint, flexion-extension mobility increases until 11-12 years of age, remains at approximately the same level until 40 years of age, and then sharply decreases. Pronator-supinator mobility of the forearm increases only up to 9-10 years.
In the radiocarpal joint, an increase in active mobility is observed up to 31-40 years, while passive movements of the hand decrease after 8-9 years.
In the hip joint, the most intensive increase in mobility is characteristic of primary school age; at 12-15 years of age, its changes are small; from 16 years of age it decreases slightly, stabilizes at 20-50 years of age, and decreases again after 50 years of age.
In the knee joint, flexion-extension mobility begins to decrease from the age of 7. Pronator-supinator mobility of the lower leg increases until 10-11 years, and then decreases.
Three stages can be distinguished in age-related changes in foot mobility: the first stage, from one year to 11-13 years, is characterized by a decrease in the range of movements; the second stage, up to 40 years of age, is accompanied by some stabilization of mobility; the third stage, after 40 years, is characterized by a subsequent decrease in mobility, especially progressing towards 70 years.
Thus, according to the nature of age-related changes in active mobility in the joints, two groups of joints can be distinguished: Group I - joints of the spinal column, hip, shoulder and elbow, in which an increase in mobility occurs up to 11 - 14 years (with its subsequent continuous decrease); Group II - knee and ankle joints, in which a decrease in mobility begins at the age of 7 years.
There are three stages in the development of passive mobility in joints: the first stage - up to 12 years - reduction in the range of movements, the second stage - from 12 to 40 years - stabilization of mobility and the third stage - from 41 to 70 years - subsequent decrease in mobility.
The greatest extensibility of the muscular-ligamentous apparatus was noted at the age of 7-12 years, and from the age of 13 it noticeably decreases. The degree of mobility in joints in athletes aged 10-17 years is higher than in children and adolescents of this age who do not engage in sports, which indicates the important role of muscle activity in its formation.
At the age of 7-8 years, the relationship between muscle strength and joint mobility is small; it increases by 9-14 years. At 15-17 years of age, a negative relationship is established between muscle strength and mobility in joints, indicating the increasing role of muscles in limiting mobility in bone joints.
The effect of sports on the skeleton.
Under the influence of increased muscle activity, significant changes occur in the athlete’s skeleton. The condition of the skeleton is also influenced by other factors associated with sports: the characteristic position of the athlete’s body (cyclists, speed skaters, boxers, rowers, etc.). the force of pressure on the skeleton (in weightlifters), the tensile force when hanging, when twisting the body (in acrobats, gymnasts, figure skaters, etc.). With correctly dosed loads, these changes are usually favorable. Otherwise, pathological changes in the skeleton are possible.
The simplest mechanism for the occurrence of skeletal changes in athletes can be presented as follows. Under the influence of increased muscle activity, a reflex expansion of blood vessels occurs, the nutrition of the working organ improves, first of all the muscles, and then nearby organs, in particular the bones with all its components (periosteum, compact layer, spongy substance, medullary cavity, cartilage covering the articular surfaces bones, etc.).
All changes in the skeleton appear gradually. After a year of systematic exercise, one can already observe clearly expressed morphological changes in the bones. They are most pronounced in the first two years of classes. Subsequently, these changes stabilize, but internal restructuring of the skeleton occurs throughout the entire training process. When active sports activities cease, adaptive changes in the bones remain for quite a long time.
The changes that occur in the skeleton under the influence of sports activities concern the chemical composition of bones, their internal structure, and the processes of growth and ossification.
Bones that bear a large load are richer in calcium salts than bones that bear a smaller load. Experiments with radioactive phosphorus showed that in animals that endured a large running load, its content increased, and more in the bones located closer to the supporting surface and experiencing greater mechanical load (M. G. Prives, V. G. Shishova, E. I. Shcherbak). On radiographs, the bones of athletes have a clearer pattern than the bones of non-athletes, which is explained by greater ossification of bone tissue and better saturation of it with mineral salts.
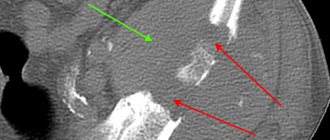
Under the influence of sports activities, the external shape of the bones changes. They become more massive and thicker due to an increase in bone mass. All protrusions, ridges, and roughness are more pronounced. These changes depend, naturally, on the type of sport. Thus, weightlifters have more massive bones than gymnasts, and gymnasts have more massive bones than swimmers, especially in the upper part of the skeleton and upper limbs. Swimmers have a poorly defined neck of the humerus, and kayakers have a poorly defined neck of the radius. Weightlifters may experience bending of the entire diaphysis of the radius, thickening of the clavicle, scapula, changes in the manubrium of the sternum, and vertebral bodies; in boxers - heads - metacarpal bones, especially the second and third. With increased physical activity beyond normal limits, changes may gradually occur in the bone tissue, bordering on a pre-pathological and pathological state, wear and tear phenomena, changes in the shape of the heads of bones are observed, marginal growths of bones appear in the area of the joints, places of rarefaction of the bone substance, etc. .
Changes in the internal structure of the bone under the influence of sports are expressed, in particular, in the thickening of its compact substance. Moreover, the thickening is usually greater in those bones that bear the greatest load. It can be uniform along the length of the entire bone or on one side, more often in places where muscles are fixed. Changes in compact matter can be symmetrical or asymmetrical. Even on the same bone they may not be the same. In gymnasts, these changes are more pronounced in the humerus and hand bones; in tennis players - in the bones of the right upper limb, especially in the radius, as well as in the area of the 1st and 2nd metacarpal bones (in connection with gripping the racket). Under the influence of static loads, greater changes in the skeleton occur than under the influence of dynamic loads, although bone strength remains high due to increased osteonization - an increase in the number of osteons and their strong connection with fibrils. It has been established that osteonized bone is more differentiated, perfect, and strong compared to lamellar bone, which has fewer osteons. Therefore, changes in the compact substance can occur without thickening it, without changing the diameter of the bone.
The cancellous bone also undergoes certain changes. In connection with the function of bones in the body, they distinguish: coarse-celled, medium-celled and fine-celled structure of spongy substance. Under the influence of increased load on the bone, the crossbars of the spongy substance become thicker, larger, and the cells between them are larger (at older ages, the cells also become larger, but the crossbars are thinner). Thus, in those who do not engage in sports, the spongy substance of the tarsal bones has a medium-cellular or even fine-cellular structure, while in football players and weightlifters it has a coarse-cellular structure; The spongy substance of the carpal bones in those who do not engage in sports has a fine-celled structure, while in gymnasts and acrobats it has a coarse-celled structure. The architecture of the spongy substance also changes. Different muscle functions not only in strength, but also in the direction of traction, the effect of gravity, i.e., an increase in body weight (for example, in weightlifters), displacement of o. c. i.e., redistribution of gravity (in cyclists, speed skaters, boxers), changes in the nature of movement - various types of repulsion (from the toe, outer edge of the foot) and landing - all this modifies the structure of the spongy substance, and may even contribute to the formation of new force lines from the crossbars of spongy substance, not usually characteristic of humans (in the heel bone of speed skaters).
Due to the thickening of the compact substance, the bone marrow cavity decreases. Under large static loads, it decreases almost until it is completely overgrown. In non-athletes, the width of the compact layer is usually less than the width of the medullary cavity at the same bone level. For athletes, the relationship can be the opposite. It must be assumed that due to the decrease in the medullary cavity in the bones, the amount of yellow bone marrow decreases, and the amount of red bone marrow increases. Since red bone marrow is a source of red blood cells, the amount of hemoglobin increases, which provides the body with oxygen, which is so necessary for the athlete’s body when performing physical exercises.
Under the influence of physical activity, the periosteum becomes stronger - it thickens, especially in football players and weightlifters, but at the same time it acquires elasticity, the number of vessels in it increases, and its osteogenic function increases.
Fractures in athletes heal faster. Articular cartilage, which covers the joint surfaces of bones, can thicken, which increases its shock-absorbing properties and reduces pressure on the bone. As for the influence of motor activity on growth and ossification processes, most authors believe that dosed physical activity leads to activation of growth zones, intensive division of cartilage cells, and rapid growth of tubular bones. For example, gymnasts and boxers have longer wrist bones. The process of synostosis in young athletes lasts longer than in children of the same age who do not engage in sports. Excessive loads initially activate bone growth, but reduce the duration of synostosis processes. The changes that occur in the joints of bones under the influence of training are expressed in increased mobility due to better extensibility of the soft tissues of the joints, ligaments and muscles lying on the side opposite to the movement, and an increase in the strength of the muscles responsible for the movement. Mobility in individual joints changes selectively, depending on the type of sport. Thus, gymnasts and acrobats are characterized by greater mobility in all joints, for tennis players - mobility in the joints of the hand, for handball players - in the joints of the bones of the upper limb, for swimmers - in the bones of the upper limb, for hockey players - in the bones of the lower limb, for track and field athletes - mobility of the foot and so on.
Connective tissues
Rice. 1. Bone connection: serrated suture, squamosal suture, mandibular joint, flat suture, vertebra, intervertebral disc, ligaments
In continuous joints, the bones are connected to each other by a layer of connective tissue, devoid of any gaps or cavities. Depending on the type of connective tissue, fibrous, cartilaginous and bone continuous connections are distinguished.
Fibrous joints include numerous ligaments, interosseous membranes, sutures between the bones of the skull and connections between teeth and jaws (Fig. 1). Ligaments are dense bundles of fibers that extend from one bone to another. There are a lot of ligaments in the spine: they are located between individual vertebrae; when the spinal column moves, they limit excessive bending and promote return to the starting position. The loss of elastic properties of these ligaments in old age can lead to the formation of a hump.
Interosseous membranes look like plates stretched between the bones over a considerable length. They firmly hold one bone next to another and serve as a place for muscle attachment. Such membranes are located, for example, between the long tubular bones of the forearm and lower leg.
Hand and foot
Rice. 4. Shoulder joint (ball-and-socket): scapula, humerus
The main differences are observed in the structure of the hand and foot. There are many movable joints among the joints of the hand, as a result of which a variety of subtle movements can be performed. The joints of the thumb are especially important, due to which the thumb of the hand can be opposed to all the others, which helps to grasp objects. The joints of the hand achieve such development only in humans! The foot bears the entire weight of the human body. Thanks to its vaulted structure, it has spring properties. Flattening of the arches of the feet (flat feet) leads to rapid fatigue when walking.
Joint mobility increases under the influence of training - remember the amazing agility of athletes and circus acrobats. But even ordinary people need to move more to maintain good joint mobility. Children's joints tend to be more mobile than those of adults and especially older people. This is due to a decrease in the elasticity of the ligamentous apparatus with age, abrasion of articular cartilage and other reasons.
Muscles
Joints are formed under the influence of muscle activity, and their structure is closely related to function. This law operates both in the process of evolution and during the individual development of the organism. An example is the features of the skeleton of the upper and lower extremities of a person, which in both cases has a general structural plan, but differs in the fine organization of the bones and their joints.
In the skeleton of the limbs, there is a girdle (shoulder and pelvic) and a free limb, which includes three parts: the shoulder, forearm and hand of the upper limb; thigh, lower leg and foot at the bottom. Differences in the structure of the skeleton of the limbs are due to their different functions. The upper limb is a labor organ adapted to perform varied and precise movements. Therefore, the bones of the upper limb are relatively smaller in size and are connected to each other and to the body by very movable joints. The lower limb in humans is designed to support the body and move it in space. The bones of the lower limb are massive, strong, and the joints have dense capsules and powerful ligamentous apparatus, which limits the range of movements.
Continuous cartilaginous connections
Many continuous cartilaginous connections between bones are present only in childhood. With age, they ossify and become continuous bony joints. An example is the fusion of the sacral vertebrae into a single bone - the sacrum, which occurs at 17-25 years of age. The formation of some skull bones (for example, occipital, temporal) from several separate parts is observed between the ages of 1 and 6 years. Finally, the fusion of the ends of the tubular bones with their middle part in the period from 17 to 21 years in women and from 19 to 23 years in men determines the completion of growth processes.
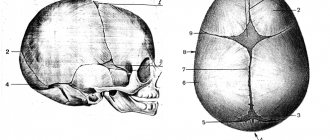
Skull sutures
Skull sutures are connections between the bones of the skull using thin layers of fibrous connective tissue. Depending on the shape of the edges of the skull bones, serrated, scaly and flat sutures are distinguished. The most elegant flat suture is found only in the facial region of the skull, and a strong serrated suture, similar to a zipper, is found in the roof of the brain. The temporal bone, like fish scales (hence the name suture), is attached to the side of the skull.
Fontana In a newborn baby, there are no sutures, and the large membranous spaces between the bones of the skull are called fontanelles. Due to the presence of fontanelles, the shape of the skull can change during the passage of the fetus through the birth canal, which facilitates the birth of the child. The largest anterior, or frontal, fontanel is located in the crown of the head, has a diamond shape and disappears only in the second year of life. Smaller fontanelles, located in the occipital and temporal regions of the skull, close in the 2–3rd month after birth. The formation of sutures ends by 3–5 years of age. After 30 years, the seams between the bones of the skull begin to heal (ossify), which is associated with the deposition of calcium salts in them. In men, this process occurs somewhat earlier than in women. In old age, the human skull becomes smooth, the boundaries between the bones are virtually indistinguishable.
Chief healer - movement
Limitation of mobility and pain during joint movements may be associated with the gradual destruction of articular cartilage and impaired production of synovial fluid. At the same time, the articular cartilage gradually becomes thinner, cracks, and the amount of lubrication becomes insufficient - as a result, the range of motion in the joint decreases. To prevent this from happening, you should lead an active, healthy lifestyle, eat right, and, if necessary, strictly follow the doctor’s instructions, because life is movement, and movement is impossible without proper functioning of the musculoskeletal system.
Author: Olga Gurova, Candidate of Biological Sciences, Senior Researcher, Associate Professor of the Department of Human Anatomy of the RUDN University
Intervertebral discs
Continuous connections of bones with the help of cartilage tissue are characterized by strength, elasticity and low mobility, the degree of which depends on the thickness of the cartilage layer. This type of connection includes, for example, intervertebral discs (see Fig. 1), the thickness of which in the lumbar, most mobile, part of the spinal column reaches 10–12 mm. In the center of the disc there is an elastic nucleus pulposus, which is surrounded by a strong fibrous ring. The core is strongly compressed and constantly strives to expand, so it springs and absorbs shocks, like a buffer. Under excessive loads and injuries, intervertebral discs can become deformed and displaced, resulting in the mobility and shock-absorbing properties of the spine being impaired. With age, with metabolic disorders, calcification of intervertebral discs and ligaments and the formation of bone growths on the vertebrae can occur. This process, called osteochondrosis, also leads to limited mobility of the spinal column.