Reasons for development
A sedentary lifestyle increases the risk of developing the disease
Dysplastic coxarthrosis is most often caused by congenital pathologies of the hip joint or underdevelopment of its individual structures. At a young age, this may not make itself felt, but after 50 years, when the joint wears out, dysplastic coxarthrosis develops.
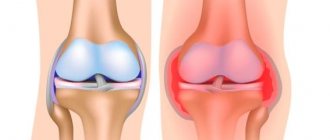
Coxarthrosis is manifested by the destruction of cartilage tissue and individual parts of the joint. Most often, the degenerative-dystrophic process affects the joints of the acetabulum; the pathological process can spread to the hip bones.
More than 80% of patients with this diagnosis are women over 50 years of age. In men, the pathology is rare.
Reasons that provoke the development of pathological changes in the hip joint:
- injuries;
- excessive stress on the legs;
- a large amount of excess weight;
- hormonal changes;
- physical inactivity;
- difficult pregnancy;
- circulatory disorders in the lower extremities;
- inflammatory diseases of other joints.
Often in women, pathology appears after a difficult pregnancy. This is explained by the fact that during gestation the load on the hip bones increases many times over. The hormonal changes that accompany this process make the bones more vulnerable. If a woman initially had congenital pathologies of the hip joint, there is a high risk of developing coxarthrosis. Moreover, pathology associated with pregnancy and childbirth can make itself felt already at 30-35 years of age. However, coxarthrosis is a slowly progressive disease, so severe symptoms appear ten years after the onset of joint destruction.
Another common reason that provokes the development of bilateral dysplastic coxarthrosis is a large amount of excess weight. Because of this, the hip joint is heavily loaded and quickly wears out, which soon makes itself felt by pain and impaired mobility in the joint.
Reasons for appearance
Crusarthrosis is a degenerative phenomenon that spreads to joint tissues, muscles, tendons and even blood vessels with nerves.
Inflammation occurs for the following reasons:
- Age-related changes in joint tissues. This explains the large percentage of patients over 60 years of age. If a person previously had good health, then this disease develops more slowly in him than in others. Disability does not occur so often.
- Obesity, starting from the second degree. Excess weight always has a negative impact on the ankle joints. The weight of the body puts pressure on the joints, so they collapse almost at lightning speed.
- Systematic abnormal loads on the ankle.
- Old injuries.
- Foot deformity that appears at birth or later.
- Genetic predisposition to developing the disease. If there are people in the family who suffer from this type of arthrosis, then the likelihood of the disease appearing in their relatives increases.
- Continuous wearing of ill-fitting shoes.
- Uneven joint load due to improper surface resistance.
Classification
Coxarthrosis can affect only one or both hip joints
Coxarthrosis is classified according to the reason for its development and characteristics of the pathological process, as well as by location.
For this reason, there are three types of disease:
- post-traumatic – occurs against the background of a femoral neck fracture, bruises and other injuries of the hip joint;
- dysplastic (dysplasia) – is a consequence of congenital dysplasia of the hip joint;
- idiopathic or unspecified - a pathology the cause of which cannot be identified.
Also, dysplastic coxarthrosis can be unilateral or bilateral. There are primary and secondary coxarthrosis. Primary dysplastic coxarthrosis in ICD-10 is designated by code 16.0 (bilateral lesion) and 16.1 (only one joint is affected). The causes of primary or idiopathic coxarthrosis cannot be established; it is associated with age-related changes.
Dysplastic coxarthrosis, resulting from joint dysplasia, is designated by code M16.2. It should be noted that this form of pathology is always bilateral.
Secondary coxarthrosis is a disease that develops against the background of other pathologies, most often injuries, bruises or inflammation in the joint. In ICD-10 it was assigned codes M16.4 – M16.7.
Based on the localization of the degenerative-dystrophic process, three forms of the disease are distinguished:
- Damage to the upper structure of the joint is accompanied by acute pain, the main cause is repeated injury to the distal part of the joint.
- Damage to the central part of the joint is the most common type, in which there is a rapid increase in symptoms. Diagnosed in the early stages.
- Damage to the lower parts of the hip joint is the most severe form of pathology, since it is this part that takes part in adducting and abducting the hip back and to the side. This form is difficult to treat.
The classification of the disease according to the localization of the pathological process is not official, but is used to facilitate understanding of the essence of the pathology.
Concept of crusarthrosis
Crusarthrosis of the ankle is a pathological phenomenon in the cartilage that occurs in a chronic form. It develops gradually, affecting tissues: over time they become thinner and destroyed. When treatment for ankle crus arthrosis is delayed, the person gradually loses important ankle functions , which significantly impacts their quality of life.
According to the international classification of diseases, arthrosis has the code M19. Crusarthrosis is more difficult to find on this list because it is a subtype of the disease. It is in the group called “Other arthrosis”. This is where you need to look for the exact definition of crusarthrosis according to ICD 10.
Symptoms of dysplastic coxarthrosis
Dysplastic coxarthrosis is manifested by pain in the joint, which can radiate to the buttocks, lower back and spread to the entire thigh, as well as a specific crunch and limitation of movement. In later stages, shortening of the limb, lameness, or inability to lean on the affected leg are noticeable.
The first symptoms to look out for are:
- pain after exercise;
- sudden aching pain at rest;
- reduction in the volume of the muscles of the thigh, buttock and lower leg;
- lameness after loading the lower limbs;
- muscle spasms.
These symptoms correspond to the early stages of the disease. You should immediately consult a doctor and begin treatment; you should not wait until the affected joint is completely deformed and cannot cope with its functions.
Degrees and stages of the disease
The stages of dysplastic coxarthrosis of the hip joint describe the degree of displacement of the femoral head and structural deformations of individual joints. There are two classifications - one describes the stages of the disease, the other - the degree of the pathological process. While stages denote structural changes, degrees are used to denote symptoms.
Stages of development
An X-ray is the best diagnostic method to find out at what stage of development the disease is
There are 4 stages of the pathological process:
- Dysplastic coxarthrosis of the hip joint of the first stage is characterized by moderate displacement of the femoral head. The deformation is insignificant, the displacement to the pelvic cavity does not exceed 50% of the distance from the original location.
- The second stage is characterized by a displacement of approximately 60-70%, the femoral head is partially hidden in the socket. The process of deformation of the joint begins, a pseudo-joint is formed, which creates the appearance of expansion of the hip part.
- The third stage is characterized by a significant shift of the femoral head, which moves towards the pelvic cavity, and only a small part of it remains in the acetabulum. The deformation of the joint is more pronounced.
- The fourth stage is the most difficult. The head completely leaves the cavity; this stage is characterized by its complete dislocation, shift to the upper part and rotation.
If we talk about symptoms, at the first stage they are moderate, and at the fourth stage, joint deformation leads to loss of motor function.
Degrees and clinical picture
The degrees of the pathological process describe specific symptoms at different stages of the disease. There are three degrees in total:
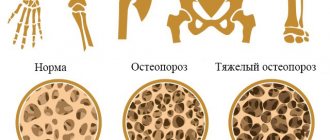
- The first degree is accompanied by a decrease in the range of motion in the joint and periodic pain that occurs after exercise. There is also a crunch in the joint, especially when rotating the pelvis and abducting the hip. X-ray shows a slight narrowing of the joint space, osteophytes are only indicated.
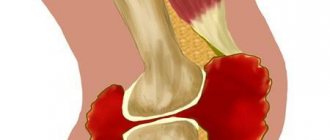
- Dysplastic coxarthrosis of the 2nd degree is characterized by a significant decrease in motor activity and periodic intense pain that occurs even at rest. The photographs show how the joint space has narrowed by 2-3 times, bone tumors (osteophytes) are clearly visible, and cysts also form on the joint.
- The third degree is characterized by severe deformation of the joint and dislocation of the femoral head. Necrosis of the femoral head may develop. The patient constantly feels pain, the supporting function of the affected limb is impaired, and movement without support is impossible. Shortening of the affected limb is also noticeable.
The most severe form is bilateral dysplastic coxarthrosis of the 3rd degree, since in this form of the disease a person cannot walk due to severe deformation of the joints.
Diagnostics
The diagnosis and treatment of dysplastic coxarthrosis is carried out by a rheumatologist. To make a diagnosis, it is necessary to take an x-ray of the diseased joint. The image clearly shows changes in the bone structure and degeneration of cartilage tissue.
MRI and CT can also be used for diagnosis - these methods are recommended for those who are afraid of X-rays.
Based on the examination results, the doctor selects a treatment regimen, which depends on the severity of the pathological process and the degree of preservation of the motor function of the joint.
Treatment of dysplastic coxarthrosis
In the initial stages of the disease, conservative treatment can be used
Treatment depends on the stage of dysplastic coxarthrosis of the hip joint - with pathology of the 1st degree, it is still possible to reduce the severity of symptoms with medications, but with the 3rd degree, surgery is necessary.
For grade 1 coxarthrosis, therapy pursues the following goals:
- reduction of pain syndrome;
- normalization of trophic processes;
- cartilage restoration;
- improved mobility;
- preventing the progression of the pathological process.
Treatment tactics for second-degree dysplastic coxarthrosis depend on the effectiveness of drug treatment. Once a therapeutic effect is achieved, surgery can be delayed. It is proposed to treat dysplastic coxarthrosis of the hip joint of the 3rd degree with the help of endoprosthetics, and in case of bilateral deformation of the joints, surgery is the only way to restore the motor and support function of the limb.
Conservative therapy
Conservative treatment is practiced in the first and second stages of the disease. It consists of taking medications, physical therapy, and manual therapy. At the first stage of the disease, special exercises may be prescribed.
Non-surgical treatment also includes an orthopedic regimen.
Drugs
The tablet is taken three times a day: in the morning, in the afternoon and before bedtime
The main medications for coxarthrosis of the hip joint are painkillers. They are prescribed primarily to reduce pain. In general, the therapy is complex and long-term.
- To reduce pain - Diclofenac, Nimesulide, Piroxicam and other non-steroidal anti-inflammatory drugs. Diclofenac can be used in the form of injections, intramuscular injections. 400 mg of ibuprofen and 500 mg of paracetamol help to quickly cope with acute pain, however, all drugs in this group can only be taken in short courses, otherwise they severely disrupt the functioning of the gastrointestinal tract, kidneys and liver.
- For thigh muscle spasms, muscle relaxants are used. Quite often, these drugs effectively relieve pain caused by spasms. The most famous drugs of this group are Sirdalud, Mydocalm.
- For inflammation in the joint, fluid stagnation and the risk of necrosis of the femoral head, corticosteroid injections are used. These hormonal drugs are injected directly into the joint capsule, and only a specialist gives the injection.
- When the production of synovial fluid decreases, a drug based on hyaluronic acid is injected into the joint, which acts as a lubricant for the cartilage.
- To restore nutrition to cartilage tissue, chondroprotectors are prescribed (Chondroitin, Structum, a biostimulator based on calf cartilage). The use of vasodilators that improve peripheral circulation is also justified.
- Additionally, vitamins and minerals, Omega-3, chondroitin and glucosamine can be used.
Chondroprotectors and restorative vitamin preparations are prescribed in long courses, because their main goal is to prevent the progression of the disease.
Orthopedic mode
Patients with coxarthrosis need to choose special orthopedic shoes to normalize the distribution of load on the lower limbs. Special corrective shoes are required when one limb is shortened.
Also, with coxarthrosis, it is recommended to move with a cane or crutch to reduce the load on the diseased joint.
Physiotherapy and exercise therapy
In dysplastic coxarthrosis, physiotherapy plays an important therapeutic role. Such procedures improve the nutrition of the cartilage and joint, normalize local blood circulation and the production of synovial fluid, thereby preventing the progression of the disease.
The choice of physiotherapeutic procedures remains with the doctor. Electrophoresis with nicotinic acid or corticosteroids, amplipulse, laser therapy and magnetic therapy have proven themselves to be effective.
Physiotherapy is not able to cope with the disease alone, but it significantly increases the effect of the medications taken and relieves pain.
Treatment is supplemented with a course of manual therapy. Therapeutic massage eliminates muscle spasms, normalizes blood circulation and improves the mobility of the affected joint.
For grade 1 coxarthrosis, it is recommended to engage in exercise therapy. Therapeutic exercise is aimed at restoring and maintaining normal mobility in the joint, but is performed only under the supervision of a rehabilitation physician.
Operation
Dysplastic coxarthrosis of the hip joint of the 3rd degree is accompanied by severe deformation of the joint and loss of the supporting function of the limb, therefore only surgical treatment can restore motor activity.
In case of moderate deformation, arthroplasty of the joint is performed; in case of dislocation and displacement of the femoral head with destruction of cartilage tissue, endoprosthetics is practiced.
The choice of surgical treatment method depends on the stage and severity of the pathological process. In any case, surgery is the most effective method of treatment; the motor functions of the joint are restored after the postoperative swelling subsides.
Treatment of ankle crusarthrosis
Therapy for crusarthrosis requires an integrated approach. In the treatment of the disease, medications and additional therapy methods are used. With the permission of a doctor, it is even permissible to use folk remedies. When conservative methods of combating the disease are unsuccessful and the situation worsens, surgical treatment of arthrosis of the ankle joint is used.
Therapy using medications is effective in stopping the severe manifestations of crusarthrosis: pain, inflammation and swelling.
For this purpose, experts advise using medications from the following groups:
- non-steroidal anti-inflammatory drugs. They will relieve pain, remove swelling and inflammation. Of this group, the most commonly used are tablets, injections, and ointments. example , " Diclofenac "
- glucocorticosteroids . They are used for severe symptoms that are not relieved by NSAIDs. For quick action, they should be injected directly into the joint. Effective therapy is provided by the drugs “Hydrocortisone”, “Diprospan” ,
- chondroprotectors. These medications are needed to return and renew decaying cartilage tissue. To achieve good results, you can use drugs such as Dona, Chondroitin ,
- vitamin complexes. They help increase the protective capabilities of the human body. They can also be used for preventive purposes. Vitamins are also effective during an exacerbation. The most popular are “Milgamma”, “Neuromultivit” .