- Causes
- Symptoms
- Joint puncture
- Complications
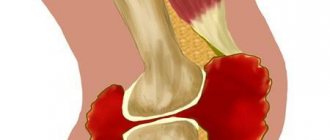
Hemarthrosis is called bleeding into a joint. It is typical for 70% of cases of traumatic knee injury. Hemarthrosis requires puncture of the joint and washing of its cavity. This is followed by immobilization of the limb and physical therapy. The presence of hemarthrosis makes it difficult to diagnose intra-articular injuries using non-invasive techniques. Therefore, for serious knee injuries with hemorrhage, diagnostic arthroscopy is often performed in the acute period of the injury.
Hemarthrosis
Hemarthrosis
- trauma – sports, domestic, professional, criminal, road traffic and any other;
- surgery – sometimes hemarthrosis occurs as a complication of arthroscopy or open surgery on the joint.
There are internal reasons that increase the likelihood of hemarthrosis. In some people, even minor trauma results in severe bleeding. First of all, the risk factors are disorders in the blood coagulation system. The cause may be a congenital deficiency of coagulation factors, acquired diseases (for example, cirrhosis of the liver), a decrease in the number of platelets in the blood (thrombocytopenic purpura, a history of severe bleeding, disseminated intravascular coagulation syndrome).
The main types of injuries that most often lead to hemarthrosis:
- meniscus damage;
- knee ligament rupture;
- damage to fatty bodies;
- intra-articular bone fractures.
Both direct (a blow to the knee) and indirect (twisted leg) injury can lead to severe damage with bleeding.
Providing first pre-medical aid
Before a person comes under the supervision of medical workers who will provide qualified treatment, it is necessary to provide the patient with first aid. To do this, several conditions must be met:
- Completely immobilize the limb using an elastic bandage or splint.
- The injured leg must be kept elevated.
- Apply cold to the damaged area.
It is strictly forbidden to give any painkillers or other medications until the patient has been examined by a doctor.
Symptoms
Hemarthrosis of the 1st degree is diagnosed after a small amount (up to 15 ml) of blood gets into the joint. But in this case the symptoms are mild. The predominant clinical picture is associated not with the hemarthrosis itself, but with the injury that led to it. A person has pain in his knee, but there is no feeling of fullness inside the joint. The patient limps when walking. Joint blockade or instability is possible.
With grade 2 hemarthrosis, more than 15 ml of blood flows into the joint. In this case, clinical symptoms associated directly with hemorrhage appear. The skin along the edges of the patella bulges, forming a “horse saddle”-shaped depression in the area where it is located. During an objective examination, the doctor palpates the knee joint and detects increased mobility of the patella. When you press on it, you feel free fluid inside the joint.
With grade 3 hemarthrosis, more than 100 ml of blood flows into the knee. The patient experiences a feeling of fullness in the joint. A symptom of balloting appears. It is determined objectively. With the patient's leg straightened, the doctor presses on the patella, after which it sinks into the joint. After the doctor releases it, the patella “floats up”. It can also become dislodged with a light blow to the thigh.
Symptoms
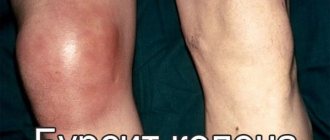
If the volume of blood spilled into the joint capsule is small, there may be no external signs at all. A person only experiences pain and discomfort - by analogy with the treatment of arthrosis or osteoarthritis of the knee, and is also forced to limit mobility. External symptoms appear if more than 40-50 ml of blood has spilled into the cavity:
- the joint swells and increases in volume;
- bruises are noticeable;
- It becomes very painful to move your leg.
Knee swelling? Fix the limb and go to a rheumatologist-orthopedic surgeon
Joint puncture
Joint puncture
This manipulation carries the risk of infection of the synovial membrane. Therefore, it is carried out with the strictest observance of asepsis and antiseptics, in a room specially equipped for this purpose. This should be a clean dressing room or small operating room. Patients with wounds that heal by secondary intention should not be served in the same room.
In the room where joint puncture is performed for hemarthrosis, everything is disinfected: walls, furniture, air. The surgeon's hands must be treated as before the operation.
In most cases, the procedure is performed with the patient lying down. Before this, the patient must undress to his underwear. If possible, he should take a shower: this will reduce the risk of infection. The area where the needle will be inserted should be shaved. If a person has long hair, it is advisable to wear a headscarf.
Executing the procedure
An orthopedic doctor palpates the joint. It determines bone landmarks, points of pain, and places where blood accumulates. The skin at the injection site is treated with antiseptics. In this case, the doctor retreats 20 cm from this zone. Iodine preparations and 70% ethyl alcohol are used for treatment. It is needed not only to destroy bacteria, but also to remove iodine residues. This substance can increase joint reactivity, increasing the risk of inflammation.
During joint puncture for hemarthrosis, the doctor follows the following principles:
Skin shift rule. The doctor inserts the needle and then moves the skin with his fingers. Thus, further injection is carried out into the joint in a place that, after the procedure is completed, will not communicate with the surface of the skin. This manipulation reduces the risk of synovitis. In addition, if the doctor injects some drugs into the joint (local anesthetics, anti-inflammatory drugs), they do not flow back because the skin returns to its original position and the wound channel has a bayonet-shaped shape.
The two-finger principle. Although the needle used to puncture the joint is quite thin, there is still a cavity inside it. It is filled with the patient's skin. With further advancement, these skin fragments enter the joint and can cause inflammatory reactions. To reduce risks, the doctor strives to ensure that as little skin as possible gets inside the needle. To do this, immediately before performing the puncture, he spreads the skin to the sides with two fingers. Its tension leads to a decrease in thickness. Accordingly, during the process of inserting the needle, a smaller volume of tissue enters it.
Pincer fixation method. Infrequently used. The only purpose of this manipulation is to distract the patient’s attention from the procedure and improve its tolerability. The doctor presses the skin at the injection site with his fingers, lifting the soft tissue. As the needle passes, the person may feel less pain. The method is sometimes used in obese patients who have increased soft tissue volume.
Anesthesia
During puncture of the knee joint, infiltration anesthesia is used to eliminate hemarthrosis. The doctor injects a local anesthetic from the same syringe with which he will subsequently suck blood from the knee. As the needle advances, lidocaine or other local anesthetic is gradually squeezed into the soft tissue, providing pain relief.
Basic principles of anesthesia:
Possible complications
Accumulated blood during prolonged stagnation tends to decompose and causes damage to joint tissues. The body’s natural reaction will be the development of inflammation in the injured joint. In addition, blood is a favorable environment for the proliferation of pathogenic microorganisms. The addition of a pustular infection threatens the development of purulent arthritis, which causes general intoxication of the body.
Inflammation may also spread to the inner lining (synovium), causing synovitis. More often, this complication accompanies the chronic course of hemarthrosis. A great danger is the formation of fibrin threads and their loss onto the intra-articular surface, which leads to the formation of scars that impede movement.
Anesthesia
Anesthesia
- the possibility of infection should be taken into account, therefore compliance with the rules of asepsis and antisepsis is mandatory;
- the skin cannot be sterile even after treatment with antiseptics, therefore, in order not to spread infection from the surface of the skin into the joint, the doctor squeezes out the first portion of the anesthetic immediately after passing through the skin (thus, the remains of the skin with bacteria are pushed out of the needle, but they get under the skin, and not inside the joint);
- for anesthesia in people with a tendency to allergies, it is better to use lidocaine;
- after withdrawing the anesthetic from the ampoule, the needle should be replaced;
- antiseptics do not kill bacteria instantly, but within 1 minute, so the doctor first lubricates the skin with iodine and alcohol, and then draws the medicine into a syringe (during this manipulation, enough time passes for the death of most microorganisms on the surface of the skin in the area through which it will be insert the needle);
- puncture of the knee can be performed through different points, but if possible it is done from the outside, since in this case the patient experiences less severe pain.
The doctor inserts the needle into the joint no more than 1-2 cm to avoid injury to the cartilage or the needle coming out of the joint cavity. An injection into the cartilage is not so much dangerous as it is painful for the patient. In addition, it can clog the needle, making pumping blood through it impossible.
After puncture of the knee, the skin puncture site is lubricated with alcohol. Then it is sealed with a napkin.
Diagnostics
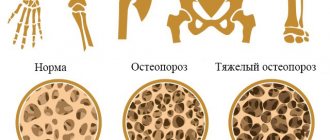
Hemarthrosis is not difficult to recognize. For an experienced specialist, it is enough to visualize clinical symptoms and know the history of previous pathology. To determine the degree of damage to bone tissue after injury, radiography is prescribed. If connective tissue injury is suspected, MRI and arthroscopy are performed.
To determine the non-traumatic form, blood clotting indicators are assessed. A consultation with a hematologist will help you correctly interpret the test result and prescribe appropriate treatment.
Five Treatment Methods
In case of a knee injury and severe pain appears after the injury, and even more so problems with movements in the knee joint, you must consult a traumatologist who will conduct an examination and prescribe treatment.
To treat hemarthrosis of the knee joint, five procedures are performed:
- Removing blood from the joint cavity using puncture or arthroscopy. During the procedure, the joint cavity is washed with a solution of novocaine and antiseptics.
- Immobilization of the knee (fixation in a stationary state) using a plaster splint (long plaster strip) for 2 weeks and limiting the load on the leg for 4 days.
- Treatment of the causes of hemarthrosis: rupture of ligaments, meniscus, intra-articular fracture (if any).
- Therapeutic gymnastics directly in the fixing bandage: tension and relaxation of the muscles of the thigh and lower leg without active movements, active movements in the hip joint.
- Physiotherapy: laser, magnetic treatment and other procedures (not earlier than a week after the injury).
Prevention of hemorrhage
To prevent the occurrence of hemarthrosis, it is sufficient to eliminate the causes that provoke its occurrence:
- if possible, be careful and avoid injury;
- during sports involving team play, during which forceful confrontation is expected (football, hockey, basketball), wear protective devices or preventive orthoses;
- in the presence of hereditary blood diseases, carry out planned treatment in a timely manner;
- Vitamin therapy courses and a balanced diet strengthen blood vessels and immunity.
After a knee injury of any nature, go to the emergency room to determine the severity of the damage in order to diagnose the accumulation of blood in the joint at the initial stage. Timely medical care and properly selected treatment predict a favorable outcome of complete recovery.