Types of polyarthritis of the joints Causes and symptoms of polyarthritis Stages of polyarthritis of the joints Treatment of polyarthritis Medicines for the treatment of polyarthritis Diet for polyarthritis
Polyarthritis
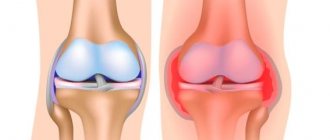
is an inflammatory disease of the musculoskeletal system that simultaneously affects 2 or more joints. With polyarthritis, several joints may suddenly become painful, or one or the other may be bothered in turn. This disease does not always affect the joints symmetrically; sometimes it can be localized in completely different parts of the body.
Polyarthritis is dangerous not only because of mobility impairments, which can lead to disability, but also because of its complications. Left untreated, it increases the risk of heart attack every year and negatively affects vision and lung function. But the question of how to cure polyarthritis and whether it can be done at all can arise before a person of any age!
Polyarthritis of the joints is an inflammatory disease that affects several joints at the same time.
Types of joint polyarthritis
Polyarthritis can affect both large and small joints of the limbs, as well as the joints of the jaw and spine. Certain types of disease may have a characteristic localization, which indirectly helps in the diagnosis of polyarthritis. For example:
- Rheumatoid polyarthritis. It is characterized by symmetrical damage to the joints, most often the wrist and interphalangeal joints, with a gradual increase in the symptoms of polyarthritis. The knee and elbow joints are often affected. Joint pain can be complemented by disorders of the nervous, cardiovascular system, vision and kidney problems.
- Reactive polyarthritis. It mainly affects the joints of the legs. The first signs of polyarthritis can appear from 2 weeks to 3 months after illness with salmonellosis, yersiniosis, mycoplasmosis, cystitis, pneumonia, bronchitis, prostatitis, pharyngitis and other infectious diseases. May be accompanied by damage to the mucous membranes and/or pain in the heart.
- Metabolic polyarthritis. It disrupts the functioning of the joints of the legs (metatarsal, ankle, knee and others), manifestations are paroxysmal in nature. Usually the disease worsens after a violation of the diet for the underlying disease.
- Infectious polyarthritis. It occurs as a result of specific infectious diseases - tuberculosis, syphilis, dysentery, brucellosis, gonorrhea - and primarily affects large joints. Pain manifests itself primarily in the shoulder, elbow, ankle, knee, and, less commonly, hip joints.
- Psoriatic polyarthritis. Despite the characteristic cause, symptoms of polyarthritis may appear before skin manifestations of the disease. It usually affects the interphalangeal joints, which gives the fingers a characteristic spindle-shaped shape.
- Idiopathic juvenile polyarthritis. Asymmetrically affects large joints, incl. cervical spine and temporomandibular.
Causes and symptoms of polyarthritis
Polyarthritis can strike a person suddenly, like a bolt from the blue, or it can grow gradually, starting with completely harmless symptoms. Up to 70% of patients who sought help were older women, and their relatives already had musculoskeletal diseases. Among the most common causes of the disease are:
- infectious diseases (dysentery, gonorrhea, tuberculosis, rubella, mumps and other infections, mainly intestinal, genitourinary);
- hereditary causes;
- metabolic disorders (gout, diabetes);
- autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, psoriasis);
- overheating, hypothermia, prolonged exposure to the sun;
- decompensated and excessive physical activity;
- overweight;
- insufficient or unbalanced diet (deficiency of protein, calcium, essential amino acids and antioxidants), as well as dehydration;
- smoking and other bad habits.
As a rule, the development of polyarthritis is promoted not by one, but by several reasons at once; in some cases, the etiology of the disease remains unclear (for example, in juvenile idiopathic polyarthritis, which occurs in children aged 16 years).
Often the symptoms of polyarthritis resemble those of rheumatoid arthritis, which most often affects women aged 30-35 years. These diseases combine pain and stiffness in the joints, increased fatigue, swelling and redness of the skin, rash over the sore spot, high body temperature, loss of appetite and body weight. However, the directions of therapy vary - that is why the treatment of polyarthritis of the joints should be selected by a doctor who is able to establish its true cause.
There are no specific signs and treatment of polyarthritis in women and men, but scientists have found that:
- women are more likely to suffer from rheumatoid arthritis because their bodies produce more antibodies;
- Metabolic, in particular gouty, polyarthritis affects men almost 20 times more often.
Diagnosis of polyarthritis, as a rule, begins with laboratory blood tests, which make it possible to determine whether the patient has a seropositive (antibodies to the body’s own cells are present in the blood) or seronegative (“wrong” antibodies are absent) form of the disease.
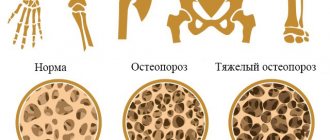
Stages of polyarthritis of joints
The division of the inflammatory process into stages in polyarthritis has a practical justification: each stage has its own risks, differences in the drug treatment of polyarthritis and the intensity of therapy.
To diagnose polyarthritis and determine the stages, X-ray examination of diseased joints, ultrasound, and, if necessary, CT and MRI are used. You may also need to take blood and joint fluid for laboratory testing and arthroscopy. Determination of biochemical signs for the treatment of polyarthritis plays a key role.
Stage 1 polyarthritis
Regardless of the cause, the symptoms of polyarthritis demonstrate minimal disease activity:
- pain is mild or moderate;
- noticeable swelling is usually absent;
- there is slight morning stiffness in the joints;
- muscle endurance decreases, which is attributed to ordinary fatigue;
- Occasionally, patients may experience seizures.
Discomfort at rest, as a rule, is not noted by patients as a pathology, so they do not think about the symptoms and treatment of polyarthritis. Signs of the disease may appear sporadically - for example, when the weather changes or after exercise - and disappear without taking medications for polyarthritis of the joints.
When visiting a doctor at the first stage of the disease, 9 out of 10 patients are cured! In those patients in whom the pathology becomes chronic, adequate treatment of polyarthritis can reduce health risks, improve quality of life, and slow down the destruction of joints.
Stage 2 polyarthritis
At this stage, obvious signs of polyarthritis are observed:
- the patient feels acute pain when moving, dull, aching or bursting pain when at rest;
- swelling;
- joint stiffness, clearly noticeable when performing everyday movements;
- increased local or general body temperature;
- muscle atrophy and deformation of the affected joints begin.
Stage 3 polyarthritis
The last stage of the disease leads to disability and incapacity for the patient, even if he receives constant drug treatment for polyarthritis. It is characterized by:
- severe pain that torments the patient even at rest and does not go away during remission;
- signs of an acute inflammatory process (fever, weight loss, decreased mood and appetite);
- serious restrictions of mobility in the joints and their deformation with swelling.
In some types of polyarthritis of the joints at this stage, serious damage to the respiratory, cardiovascular, digestive and other internal organ systems occurs.
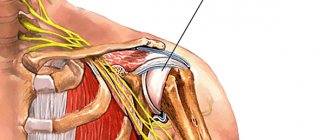
Diagnosis of shoulder arthrosis
Doctors at our clinic carry out comprehensive diagnostics. At the first stage, oriental methods are used, with the help of which both the degree of the local problem and the general condition of all body systems are determined:
- Pulse diagnostics. Used to determine the state of systems and contributes to a more accurate diagnosis.
- Load tests. Help in more accurately diagnosing a local problem.
The second stage includes hardware diagnostics:
- X-ray examination. Its advantages are the speed of research and low cost.
- Magnetic resonance imaging. A method that gives a complete understanding of the state of the ligamentous apparatus.
- Ultrasonography. Informative when the signs of the disease have become quite obvious.
Treatment of polyarthritis
Polyarthritis of the joints, which is associated with modifiable factors (lifestyle, consequences of non-chronic infectious diseases), has a high chance of a complete cure for the patient. If polyarthritis is secondary and associated with chronic diseases (rheumatoid arthritis, psoriasis), the patient requires lifelong therapy for the underlying disease and prevention of exacerbations of the joints.
Complex therapy of polyarthritis itself includes measures to eliminate pain and relieve inflammation, activate metabolic processes and regenerate cartilage tissue in diseased joints. In addition to pharmacotherapy and physiotherapy, these include control of diet and body weight, normalization of sleep and exercise, and the use of orthoses.
Before treating polyarthritis, the doctor needs to determine the stage of the inflammatory process - whether it is in the stage of exacerbation or remission. This is due to the fact that in the acute phase of the disease, massage, exercise therapy and some physiotherapeutic techniques are contraindicated and are replaced by anti-inflammatory drugs for polyarthritis of the joints.
Physiotherapy for polyarthritis of joints
In the absence of contraindications, patients with signs of polyarthritis are prescribed:
- magnetic therapy;
- laser therapy;
- acupuncture;
- electrophoresis with drugs for polyarthritis;
- amplipulse;
- thermotherapy (heating applications, cryotherapy, etc.);
- UV therapy;
- ultrasound therapy;
- UHF;
- barotherapy;
- balneological techniques (herbal, radon, bromine and other baths) and mud therapy.
Massage for polyarthritis of joints
In the absence of acute inflammation, patients with polyarthritis can attend therapeutic massage sessions, which prevent muscle atrophy and improve metabolic processes in the joint. But some massage movements can be repeated at home, on your own:
- Superficial rubbing movements (circular, back and forth) - repeat until the skin becomes noticeably warm.
- Stretching movements (for example, with the edge of the palm) designed to gently stretch muscles and ligaments without injuring them at the points of attachment to the articular heads.
- Deep kneading movements (mainly with fingertips).
Exercise therapy in the treatment of polyarthritis
Therapeutic exercises are effective for relieving inflammation, nourishing and regenerating cartilage and periarticular tissues, and reducing pain.
Exercise therapy exercises for the treatment of polyarthritis of the joints are performed daily, at least 3 times a day for 15 minutes. This helps to consolidate the results of medications and physical therapy and bring the disease into stable drug-free remission.
An individual list of exercises, taking into account the patient’s age, gender, physical fitness, stage of the disease and lifestyle, should be compiled by a specialist - exercise therapy instructor, rehabilitation specialist.
Exercise therapy for glenohumeral periarthritis
At the initial stage of treatment of glenohumeral periarthritis, patients do the following exercises from the starting position “lying”:
- They clench and unclench their fingers, shake the brush;
- Bend your arms at the wrist joint;
- Holding your arms along your body, turn your palms down and up;
- Keep your arms along the body, while inhaling, bring your hands to your shoulders, and while exhaling, lower them.
You can bend your elbows and spread your forearms to the sides, bringing the back of your hand as close as possible to the horizontal surface. The hands should be kept on the shoulders, the elbows in front of you, as you inhale, spread the elbows to the sides, and as you exhale, place them vertically again.
The following exercises for shoulder osteoarthritis are done while sitting:
- Place your hands on your waist, spread your elbows to the side and bring them towards each other at low speed;
- Hands are located at the waist, simultaneously rotate both shoulders forward and backward;
- As you inhale, bend your elbows, and as you exhale, lightly swing them back and forth;
- Place your hand behind your back and raise your palm to your shoulder blade.
Rehabilitation specialists at the Yusupov Hospital select an individual set of exercises for each patient for glenohumeral periarthritis. These exercises are suitable for treating the disease at home.
Medicines for the treatment of polyarthritis
Drug treatment of polyarthritis includes taking anti-inflammatory and painkillers, chondroprotectors, blood microcirculation correctors and angioprotectors, vitamins and minerals. Depending on the cause of the disease, effective drug treatment of polyarthritis may also require immunosuppressive, antihistamine and/or antibiotic therapy. Based on the patient’s psycho-emotional state, the doctor may also prescribe antidepressants.
Chondroprotectors for polyarthritis
These drugs for the treatment of polyarthritis are aimed at eliminating not the symptoms, but the consequences of the disease - they start the process of regeneration of synovial cartilage in the joint, slow down its decay and deformation of the joint. The effect after taking chondroprotectors occurs within 3-6 months. To maintain joints, doctors recommend lifelong use of glucosamine and chondroitin sulfate in courses of about 6 months a year.
Effective chondroprotectors include: artracam, dona, movex, chondros, structum, alflutop, artiflex, elbona, protecon, chondroitin complex and others.
Anti-inflammatory for polyarthritis
Anti-inflammatory drugs in the treatment of polyarthritis are used externally, orally, intravenously, intramuscularly or in the form of intra-articular injections (in this case they can be combined with anesthetics, hyaluronic acid preparations, antibiotics).
In the early stages, with a mild or moderate course of the disease, non-steroidal anti-inflammatory drugs for polyarthritis of the joints (NSAIDs) are prescribed: ibuprofen, ketoprofen, diclofenac, meloxicam, piroxicam, nimesulide, voltaren, indomethacin, naproxen.
If NSAIDs are not enough to cope with the symptoms of the disease, glucocorticosteroid drugs are used to treat polyarthritis: prednisolone, methylprednisolone, betamethasone, Maxitrol, Metypred, Kenalog, Clenil, hydrocortisone.
NSAIDs are often combined with gastrointestinal protective agents (for example, omeprazole).
Immunosuppressants for polyarthritis
For rheumatoid polyarthritis, the so-called basic therapy with drugs for polyarthritis that suppress the activity of the immune system. These include: methotrexate, sulfasalazine, xeloda, azathioprine, leflunomide, ftorafur and others.
Attention: taking these medications for polyarthritis of the joints must be suspended during colds and other illnesses.
Auxiliary agents in the treatment of polyarthritis
To relieve symptoms and normal nutrition of periarticular tissues, drugs that protect blood vessels and relax muscles are used in the treatment of polyarthritis of the joints.
Antispasmodics and muscle relaxants: mydocalm, papaverine, no-shpa, sirdalud (tizanidine), Novigan, baclosan, tolperisone and others.
Angioprotective drugs for polyarthritis: troxerutin, troxevasin, horse chestnut extract, detralex, actovegin, pentoxifylline.
Medical nutrition
Often the cause of polyarthritis of the joints is poor nutrition. Harmful substances, toxins, and fat deposits accumulate in the body. For this reason, getting rid of the problem will mean reviewing your diet and following the principles of the diet.
Therapeutic nutrition is aimed at reducing the level of acidity in the body and eliminating salt from the joints, which prevents cartilage tissue from being flexible.
If you include certain foods in your menu, you can expect that the symptoms of the disease will subside and the inflammation will subside. So, doctors recommend eating:
- vegetable and fruit salads;
- dairy products;
- rosehip decoction;
- boiled vegetables (especially peas, carrots, beets, asparagus);
- sorrel, lettuce;
- blueberries, black currants;
- plums, apples;
- boiled rice (it should be boiled until slimy).
Some foods and drinks will have to be eliminated completely or limited.
This includes fried meat, strong tea, coffee, liver, alcoholic drinks, beans, mushrooms, pickles, marinades, and preserves. Boiled meat and fish can be eaten no more than 2 times a week.