Non-traumatic shoulder pain associated with subacromial structures is a hot topic in the scientific community. Disputes are still raging - how exactly to classify it and what name to give it?
The term subacromial impingement syndrome (SAIS), which refers to shoulder pain when the arm is raised, was first coined in 1972 by Dr. Charles Neer. It is based on impingement (biomechanical pinching) of structures located in the subacromial space. SAIS is considered to be a symptomatic irritation of the subacromial structures between the coracoacromial arch and the head of the humerus when raising the arm above the shoulder or head. According to many experts, this is one of the most common causes of shoulder pain.
Classification
Types of acromion
Nir identified four types of shoulder impingement syndrome.
1/ First degree: age <25 years, reversible edema, tendinitis, no tears, conservative treatment.
- Moderate pain during exercise, muscle strength and range of motion remain unchanged. Swelling or bleeding may be present. This condition usually occurs in patients under 25 years of age and is often caused by overuse injuries. At this stage, the syndrome may be reversible.
2/ Second degree: 25-40 years, presence of permanent scars, tendonitis, no tears, subacromial decompression.
- Pain occurs when performing normal daily activities and is especially common at night. With this condition, the range of motion in the joint is limited. This is a more serious pathology, which is more common in patients 25-40 years old. Pathological changes include connective tissue fibrosis, as well as irreversible changes in the tendons.
3/ Third degree: age >40 years, minor rotator cuff tears, subacromial decompression and necrectomy/surgical correction.
4/ Fourth degree: age >40 years, large rotator cuff tears, subacromial decompression with surgical correction.
Nir's classification at one time served as the key to understanding the pathology of the shoulder joint. SAIS was later classified into four subtypes depending on whether it was external or internal impingement.
External impingement
Primary external impingement is associated with structural changes in the glenohumeral joint, which results in a mechanical narrowing of the subacromial space. These changes include changes in bone volume, formation of osteophytes, malalignment of bones after fractures, or proliferation of subacromial soft tissue. These pathologies can be either congenital or acquired. The shape of the acromion or scapula can play a big role in recovery and treatment after primary external impingement syndrome.
Friends, Georgy Temichev’s seminar “Diagnostics and treatment of problems of the glenohumeral complex” will take place very soon. Find out more...
Secondary external impingement is associated with abnormal scapulothoracic kinematics and altered force balance. This leads to a functional disruption of the centering of the head of the humerus, which entails a shift in the center of rotation when raising the arm. The cause of these problems is weakness of the rotator cuff muscles (functional instability) in combination with weak ligaments and the capsule of the shoulder joint (micro-instability). Typically, the obstruction occurs in the coracoacromial space due to anterior displacement of the humeral head. In primary impingement, the damage occurs in the subacromial space. Secondary impingement usually occurs in younger patients and is accompanied by pain on the front and side of the shoulder. Symptoms tend to be specific to certain activities, including those involving downward punching.
Internal impingement
Internal impingement is perhaps the most common cause of pain in the back of the shoulder in athletes with strong high serves. The cause lies in the impingement of the rotator cuff tendons (namely, the posterior surface of the supraspinatus muscle and the anterior surface of the infraspinatus muscle) between the greater tubercle of the humerus and the posterosuperior part of the labrum. Basically, this syndrome is observed with frequent movements when the hand is above the head. This position becomes pathological during maximum external rotation, with anterior capsular instability, imbalance of the muscles of the glenohumeral complex and/or excessive load on the rotator cuff muscles. All of the above together leads to loss of control over the shoulder and scapula.
These definitions and descriptions of CAIS are based on the hypothesis that irritation of the acromion leads to external abrasion of the bursa, rotator cuff, and other structures of the subacromial space. However, the pathology description later expanded to “impingement associated with shoulder pain,” reflecting the view that “impingement” represented a whole group of symptoms and possible mechanisms of pain, not just a pathological diagnosis in itself. This theory has been dominant for the past 40 years and has served as the rationale for clinical tests, conservative therapy, surgical interventions and rehabilitation protocols. However, in the last decade, the validity of this theory has been questioned from both theoretical and practical points of view. It has been suggested that the terminology used may negatively bias the patient toward conservative treatment options and physical therapy. As a result, treatment results may be worse than expected, which very often forces patients to opt for surgery.
Against the backdrop of ongoing debate over terminology and a large number of definitions with which they try to describe subacromial pain and its pathophysiology, it has been suggested that the term SAIS, after all, does not fully reflect the mechanism of the pathology. At this time, the most appropriate term chosen is “Subacromial Pain Syndrome” or SPS, which best describes the pain thought to originate in the structures located between the acromion and the head of the humerus. This term, however, does not reflect other causes of shoulder pain located outside the subacromial space.
Definition/Description
Diercks et al. define SBS as a collection of non-traumatic, unilateral shoulder problems that cause pain localized around the acromion, usually worsening during or after raising the arm. It is essentially an umbrella term that describes pain caused by any injury to any structure or structures within the subacromial space. Thus, the term includes all conditions associated with subacromial structures: subacromial bursitis, forearm calcification, biceps tendonitis, or rotator cuff tendon degeneration.
Etiology
The question of the etiology of the disease is still open. It is assumed that its mechanism may be associated with internal and external factors, as well as their combination. These include muscle imbalances and anatomical factors that affect the subacromial space, various shapes of the acromion, its anterior slope, its angle, and the lateral extension of the acromion relative to the head of the humerus. Bone changes in the inferior acromioclavicular joint or coracoacromial ligament may also affect the subacromial space.
Although it is generally accepted that several factors are involved in the pathogenesis of the disease, several important unresolved questions remain. Namely, which subacromial structure is the first to suffer as a result of pathology and what are the mechanisms that cause pain?
Features of the operation of subacromial decompression of the shoulder joint
As already mentioned, the goal of surgery is to expand the space between the cuff and the acromion, as well as to reduce the pressure in the soft tissues that lie underneath. To achieve the first, the surgeon excises a small part of the acromion itself, the second - removes the bone growths underneath it. If the acromion has a non-standard shape, which is characterized by a downward slope, a significant amount of bone tissue is excised, that is, acromioplasty is also performed: open or minimally invasive, that is, through arthroscopy. In the latter case, a special optical device is used - an arthroscope, which provides the surgeon with an overview of the space inside the joint. It itself is a tube made of medical steel containing a lens system.
It contains a video camera that transmits the image to the monitor. The operation is performed through minimal incisions, resulting in minimal trauma to healthy tissue. The result is rapid healing and a short rehabilitation period. In the process, the surgeon creates two or three incisions and inserts instruments through them into the joint cavity. He has the opportunity to fully examine all parts of the joint. During the operation, the necessary flow of fluid is provided, which is necessary to flush the joint and remove blood and damaged tissue from it.
Clinically Relevant Anatomy
Anatomy of the shoulder joint
The subacromial space is the space located under the acromion (between the upper edge of the head of the humerus and the acromial process of the scapula). This space is bounded by the acromion and coracoid process (which are part of the scapula), connected by the coracoacromial ligament.
Treatment of impingement syndrome.
Treatment of subacromial syndrome depends on the severity of clinical manifestations and the degree of development of the destructive process. If pain occurs at an early stage, it is important to rest your hand. The patient receives anti-inflammatory drug therapy by taking a course of non-steroidal anti-inflammatory drugs orally. For prolonged pain syndrome, blockades are performed with the introduction of glucocorticosteroids into the affected area. Sometimes injections of platelet-rich plasma are recommended for better regeneration of the damaged area. During the recovery period, therapeutic exercises are prescribed, aimed at returning the muscles to function. Loads are given gradually and already during the period when there is no pain syndrome. Physiotherapeutic procedures speed up the healing process and include shock wave therapy, electrophoresis, magnetic therapy, electrical myostimulation). In the second and especially third degree, when degenerative changes in muscle tendons, ligaments and bone structures are observed, surgical treatment is indicated, since conservative therapy can provide relief only for a while.
Surgical intervention is performed using arthroscopy, which is the most gentle in relation to surrounding tissues. In addition, rehabilitation after arthroscopy is much faster than after open access operations. During arthroscopy, a revision of the subacromial space is performed; at the second stage, subacromial decompression is most often performed, including the intersection of the coracoacromial ligament with anterior acromionoplasty; at the third stage, osteophytes are removed along the lower surface of the acromial process of the scapula and the integrity of the tendons is restored by suturing or plastic surgery. Rehabilitation measures after arthroscopy are prescribed after 1-2 weeks, when tissue swelling decreases. They include physical therapy. Exercises are given by a rehabilitation doctor with a gradual increase in load. Kinesio taping and the use of fixatives help regulate the inclusion of certain muscles in work. Physiotherapeutic methods accelerate the healing process and contribute to the speedy restoration of joint function.
In cases where physical therapy and medications do not bring results, you still have to resort to surgery. At the SportClinic you will be able to undergo it with the best surgeons in Russia. You will also have access to effective rehabilitation and a full range of services in the field of sports medicine.
Clinical picture
Clinical picture
This disease mainly occurs in patients over 40 years of age who suffer from constant shoulder pain. They have no previous injuries. Pain in such patients occurs when raising the arm between 70 ° and 120 °, in a “painful arc” (see figure), when forced to move the arm above the head and when lying on the affected side. Symptoms may be chronic or acute. More often than not, it is a gradual, degenerative process that causes impingement, rather than some strong external factor. This is why it is often difficult for patients to name the exact onset of symptoms.
Diagnostics
Physical examination
A detailed history and clinical examination are essential components for making a diagnosis of SBS. It should be noted that any one test is not enough to diagnose true pathology of the shoulder joint, so it is necessary to use a combination of different tests.
Read about the rotator cuff here.
The Dutch Orthopedic Association has issued guidelines for the diagnosis and treatment of subacromial pain syndrome, which recommends the following tests:
- Hawkins-Kennedy test.
- Painful arc test.
- Infraspinatus (external rotation) resistance test.
The combination of these tests has a higher prognostic value.
- If three tests are positive at once, then the probability that the patient has SBS is 10.56.
- With two positive tests, the probability is 5.03
- One positive test - 0.90.
- In the absence of positive tests, the probability of having the syndrome is 0.17.
To rule out a rotator cuff tear, the following test must be performed:
- Drop Arm Test, which helps determine the integrity of the infraspinatus muscle.
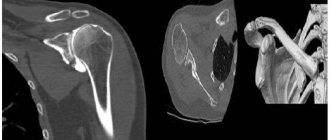
Instrumental diagnostics
X-rays can help identify anatomic changes and may also reveal calcification or arthritis of the acromioclavicular joint. It is recommended to take x-rays in three projections:
- Anterior-posterior view: The image is taken with 30 degrees of external rotation of the shoulder, which helps evaluate the shoulder joint and detect subacromial osteophytes or sclerosis of the greater tuberosity of the humerus.
- Lateral projection: with its help it is possible to see the subacromial space and differentiate the pathology.
- Axial view: Helps visualize the acromion and coracoid process, as well as calcification of the coracoacromial ligament.
It is also possible to evaluate the subacromial space. MRI can help identify complete or partial tears of the rotator cuff tendons, as well as inflammation. Ultrasound and arthrography are used when a rotator cuff tear is suspected or in complex cases.
Shoulder ultrasound is a specific and sensitive imaging modality. Its diagnostic accuracy is high and comparable to standard MRI, which allows the detection of partial or complete rotator cuff tears.
Guidelines issued by the Dutch Orthopedic Association recommend the use of ultrasound as the most useful and cost-effective imaging modality if the first period of conservative treatment fails. The association recommends combining ultrasound with conventional radiography of the shoulder joint to determine osteoarthritis, bone abnormalities and the presence/absence of calcium deposits. The guidelines also emphasize that in cases where reliable ultrasound is not available or is inconclusive, then MRI of the shoulder is indicated. MRI should also be used in patients undergoing surgical repair of a rotator cuff tear to assess the extent of retraction and fatty infiltration.
If it is necessary to exclude any intra-articular anomaly or partial damage to the rotator cuff, it is possible to conduct an MRI study with intra-articular contrast. It is preferable that the shoulder be abducted and in external rotation during the examination.
Differential diagnosis
There are a number of pathological conditions that are easily confused with subacromial pain syndrome. A thorough physical examination should rule out the following:
- Complete or partial tear of the rotator cuff.
- Superior outlet syndrome.
- Cervical spondylosis.
- Subluxation of the shoulder joint.
- Pathologies of the acromioclavicular joint.
- Adhesive capsulitis of the shoulder (“frozen shoulder”).
- Arthritis of the shoulder joint.
- Trapezius muscle paralysis.
- Calcific tendinitis.
- Subacromial bursitis.
- Arthropathy.
- Instability of the shoulder joint.
Causes of shoulder impingement syndrome
- Cervical osteochondrosis.
- Neuropathy of the suprascapular nerve.
- Arthrosis of the acromioclavicular joint.
- Adhesive form of capsulitis (humeral periarthritis, “frozen” shoulder).
- Calcification and rupture of the rotator cuff tendons.
- Pseudoparalysis of the shoulder joint.
- Arthropathy of the shoulder joint.
- Instability of the shoulder joint.
In addition, the development of shoulder joint impingement syndrome can be influenced by injuries, degenerative and deforming changes.
Treatment
Treatment depends on the patient's age, activity level, and general health. The goal of treatment is to reduce pain and restore function. The first line of treatment is conservative treatment, which should be followed for at least a year until joint function improves and returns. Surgery should only be considered if the patient does not respond to comprehensive nonoperative treatment.
Conservative treatment consists of rest, reduction of activities that trigger the syndrome, such as movements with the arms above the head, NSAIDs to relieve pain and swelling, physical therapy and injections in the subacromial area. Cortisone is often prescribed for its anti-inflammatory and pain-relieving properties, but should be used with caution and avoided if you have pain due to tendon problems.
There is no convincing evidence that surgery is more effective than conservative treatment. Surgery is indicated only if it is not possible to reduce pain and restore function with a conservative method. Depending on the nature and severity of the injury, certain surgical techniques are used, but there are no clear preferences among them.
Surgery
Surgical repair of torn tissue, especially the supraspinatus muscle, long head of the biceps, or joint capsule. It should be kept in mind that a rotator cuff tear is not an indication for surgery.
- Bursectomy or removal of the subacromial bursa of the shoulder joint.
- Subacromial decompression to increase the subacromial space by removing bone spurs or protrusions on the underside of the acromion or coracoacromial ligament.
- Acromioplasty to increase the subacromial space by removing part of the acromion.
- Arthroscopic acromioplasty is a less invasive procedure than open surgery and also requires less recovery time.
Current research suggests that there is no difference between open surgery and arthroscopic surgery in terms of shoulder function and complications. Open bunionectomy is likely to produce the same clinical outcome as bunionectomy with acromioplasty.
Physical therapy
Case Study of the Shoulder Injury Patient
There is compelling evidence that supervised nonoperative rehabilitation reduces shoulder pain and improves joint function. Unless the patient has a rupture that requires surgical repair, the first line of therapy should be conservative treatment (level of evidence: 4).
Read about the most effective exercises for the subscapularis muscle here.
Physical therapy includes:
- RICE therapy (rest, cold, elevation and compression) – used in the acute phase to reduce pain and swelling.
- Stabilization and postural correction exercises.
- Mobility exercises.
- Exercises to develop strength.
- Stretching, including capsular stretching.
- Manual therapy techniques.
- Acupuncture.
- Electrical stimulation.
- Ultrasound.
- Low-level laser therapy has a positive effect on all symptoms except muscle strength (evidence level 1b).
- Corticosteroid injections in the first 8 weeks.
- High-intensity extracorporeal shock wave therapy is not recommended in the acute phase. High-intensity shockwave therapy is more effective than low-intensity shockwave therapy (level of evidence: 2a).
In the acute period, therapy should be aimed primarily at reducing pain, after which you can move on to strength exercises. This sequence is necessary to avoid injury in the future. Exercise on its own has proven to be effective, but when combined with manual therapy, it can further improve muscle strength. Exercise is the cornerstone of treatment for subacromial impingement, but studies have found no difference between exercise at home and in a clinic (Evidence Level 1b).
Strength training should include (level of evidence 1a):
- Strengthening the rotator cuff: external rotation exercises using expanders, horizontal abduction.
- Strengthening the lower and middle portions of the trapezius muscle (push-ups, unilateral scapular rotations, bilateral external shoulder rotations, unilateral scapular depression).
- Strengthening the lower trapezius muscle is an important part of physical therapy. In patients with subacromial impingement, this portion is weaker than the middle and superior portions of the muscle (LE: 3b).
A specific rehabilitation program that includes eccentric rotator cuff strengthening exercises and eccentric and concentric exercises for the scapular stabilizers has been shown to reduce pain and improve shoulder function (Evidence Level 1b).
Soft tissue mobilization has been shown to be effective in normalizing muscle spasm and other tissue dysfunctions. Joint mobilizations are also effective for SBS to restore range of motion (LE: 3b).
The combination of physical therapy and surgery produces better clinical outcomes than physical therapy alone (level of evidence: 2b).
The movements of the rotator cuff that need to be especially carefully worked on during SBS are internal and external rotation, as well as abduction. It is important to remember that the rotator cuff not only performs a rotation function, but also stabilizes the shoulder joint. Thus, the stronger the rotator cuff muscles, the less pinching. To begin with, it is recommended to perform 10-40 repetitions 3-5 times a week and use additional weights (4-8 kg).
Patients with stage two impingement may require a formal physical therapy program. Isometric stretching can be helpful to restore range of motion. It is also recommended to perform isotonic exercises with a fixed rather than variable weight. Therefore, shoulder exercises in this case are best performed with a stable weight rather than with rubber bands. The emphasis is on repetitions rather than weight, and the exercises use light weights. Sports-specific techniques are sometimes useful, especially to improve movements such as throwing, serving, or swimming movements. In addition, physical therapy techniques such as electrogalvanic stimulation, ultrasound therapy, and transverse friction massage may be helpful (Evidence Level 2b).
Rehabilitation after subacromial decompression of the shoulder joint
The rehabilitation period after subacromial decompression of the shoulder joint is quite long. It will take at least several months for the patient to fully recover. At the same time, the operated joint itself will require physical activity as early as possible, but only if it is properly balanced. In addition, in the first days it is possible to use various physical therapy techniques that will reduce pain symptoms and swelling in the operated area. For several weeks, the patient needs to wear a special bandage that will provide the necessary support and protection to the shoulder.
Do you want to be sure that the operation will be successful? Sign up for a consultation with our clinic specialists. Call.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions