Debridement of the knee joint. This is an invasive procedure to remove pathological tissue. Using surgical instruments and equipment, an arthroscope is inserted into the joint to assess the condition of the articular surfaces of the tibia and femur. During the procedure, dense formations that interfere with the functioning of the joint are removed. At the same time, it is possible to remove growths on the bones that have arisen as a result of inflammation.
According to indications, lavage of the knee joint is performed along with debridement. This is washing the structure from microorganisms and contaminants using special sterile solutions. The doctor removes small, free pathological formations from the joint cavity. As a result, inflammation is reduced.
Debridement: the essence of the technique
With the development of degenerative pathologies in the cavity of the articular joint, there is a malnutrition of the cartilage tissue, which negatively affects its structure and makes it less elastic. Under the influence of external and internal factors, the cartilage becomes covered with microcracks, which leads to complex inflammatory processes. In such cases, pain occurs and the natural mobility of the joint is disrupted. More often, this phenomenon is observed in the area of the knee and hip joint, which is associated with their special mobility.
To eliminate negative symptoms and prevent rapid degeneration of the joint, arthroscopic debridement is used, which is carried out using an arthroscope and other manipulators. The surgical procedure allows for an extensive examination of the affected area and removal of particles from damaged structures. To improve the mobility of the joint, dead areas of cartilage, pathologically altered synovial membrane and osteophyte growths, which act as a mechanical irritant, are eliminated.
Debridement refers to modern minimally invasive methods of treating degenerative-dystrophic diseases of the musculoskeletal system.
Indications for use
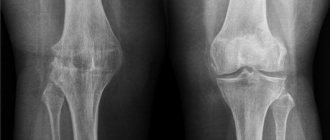
Before prescribing the procedure, the doctor collects a history of complaints, conducts an external examination of the affected joints, and also prescribes studies in the form of radiography, CT, MRI and laboratory tests of blood and synovial fluid. The main indication for the use of debridement is knee arthrosis at stages 1 and 2 of development. Sanitation of the joint is carried out in the presence of the following negative symptoms:
- pain when moving and staying in an upright position;
- stiffness and impaired mobility in the morning, which goes away after warming up;
- change in gait with manifestation of lameness;
- inability to move without aids.
The effectiveness of the technique can be seen only when the cartilaginous structure is partially damaged. Significant changes in the joint cannot be eliminated with such an operation. Timely surgical intervention eliminates negative symptoms for several years. After the expiration of the period, the procedure is repeated or a more radical type of operation is used.
Methods
The procedure is considered anemic. To carry it out, small punctures are made through which an instrument is inserted to remove pathologically altered areas of the knee joint. Depending on the technology used, there are three methods of performing the operation:
The most commonly used type of operation is mechanical.
- Mechanical. A traditional technique using an arthroscope, which has been used for many years.
- Laser. Affects the small diameter of the joint, which minimizes damage to nearby soft tissues.
- Cold plasma. It is carried out using cold plasma, which stops bleeding by affecting damaged areas of the capillaries. Cold plasma debridement of the shoulder joint is often performed, less often for implementation in the knee area.
Return to contents
Possible contraindications and complications
It is important to note that arthroscopy is not performed for the following concomitant pathologies:
- skin rashes of the pustular type in the shoulder area;
- infectious diseases with localization of the focus in the shoulder joint;
- elevated body temperature, regardless of cause;
- previously diagnosed ankylosis;
- intolerance to painkillers/anesthetics.
Any surgical intervention comes with a risk of complications. But the degree of this risk is important. With the artoscopy method, these are minor complications that can only cause some discomfort to the patient. After joint arthroscopy, swelling and redness of the soft tissues may be observed in the areas where punctures and incisions were made. However, they disappear literally after 3-5 days.
It is extremely rare that deep veins may be damaged during surgery, but this is not dangerous for the patient. We are always able to quickly provide the necessary assistance.
Pros and cons of knee debridement
The main advantages of debridement of the knee joint are the use of local anesthesia and minimal trauma to the joint and soft tissues during the operation. Such surgical intervention is an excellent alternative to eliminate the consequences of arthrosis for people who, for medical reasons, are contraindicated for more serious interventions into the joint structure.
Thanks to this treatment method, the following results can be achieved:
- remove particles of damaged cartilage, which prevents the development of inflammation;
- eliminate structural changes in cartilage tissue through gentle action;
- eliminate damage to the joint that was caused by mechanical irritants.
After such an intervention, the patient needs to control his weight.
The disadvantages include the need for additional therapeutic manipulations to maintain the therapeutic effect after the procedure. These include:
- use of a wide range of medications;
- compliance with a certain motor mode;
- use of a full course of physical rehabilitation in the form of exercise therapy, massage and physiotherapy;
- compulsory preventive sanatorium treatment;
- weight control;
- rejection of bad habits.
Benefits of Shoulder Arthroscopy
Here are the main advantages of arthroscopy over traditional “open” surgery that patients usually pay attention to:
- the patient is in the inpatient department of a medical institution for a short period of time: a maximum of 3 days, but most often the period is limited to 24 hours;
- During the operation, soft tissues are minimally injured, since incisions only 5-7 mm long are used;
- The cost of arthroscopy is quite adequate and affordable for absolutely all patients.
A more accurate diagnostic examination of the joint simply does not exist in medicine today! Arthroscopy does not allow errors, and at the same time it is possible to immediately carry out the necessary medical manipulations.
Debridement of the knee
With age, human joints are subject to degeneration, which provokes chronic diseases (arthrosis), the treatment of which uses different methods. Debridement of the knee joint is an organ-preserving surgical procedure in medical practice, which allows to slow down the development of the disease and stop symptoms. It is used on large joints of the human body - knee, shoulder, hip.
Types of Knee Replacement Surgeries
Knee replacement can be total or partial.
Total knee replacement (TKR): Surgery involves replacing both sides of the knee joint. This is the most common procedure.
The operation lasts from 1 to 3 hours. The person will experience decreased pain and improved mobility, but there will be scar tissue that may make it difficult for the knee to move.
Partial Knee Replacement (PKR): A partial replacement replaces only one side of the knee joint. Less bone is removed, so the incision is smaller.
PKR is suitable for people with damage to only one part of the knee. Post-operative recovery is easier, there is less blood loss and there is less risk of infection and blood clots.
The hospital stay and recovery period are usually shorter and there is a higher chance of natural movement.
What is debridement?
From English this term is translated as “surgical debridement of a wound.” During osteoarthritis, arthritis, and trauma, non-viable elements accumulate in the joint cavity - necrotic particles of hyaline cartilage, bone osteophytes (growths) and flakes. All of them provoke severe pain, disruption of the functional activity of the joint, up to complete immobility. Arthroscopic debridement allows, with minimal surgical intervention, to remove dead particles clogging it from the joint cavity, thereby improving a person’s quality of life.
Types of operations for gonarthrosis
Today there are several types of arthroscopic interventions. The most common ones are:
- Arthroscopic lavage and debridement is a sanitation operation during which the surgeon washes the articular cavity and removes fragments of destroyed cartilage from it.
- Chondroplasty (mosaic, coblation, abrasive) is an operation aimed at restoring damaged cartilage. Along with chondroplasty, the surgeon can remove curved menisci, change the shape of damaged ligaments and capsules, etc.
- Plasma ablation is the effect of cold on articular cartilage. Causes collagen compaction in cartilage and thereby improves its structural and functional condition.
- Laser arthroscopy - involves exposure of cartilage, subchondral bone, menisci and synovium with a special laser. This is a highly effective technique, which is still rarely used, but continues to be actively introduced into clinical practice.
For patients with impaired axial parameters of the limb, corrective osteotomy is most often performed instead of arthroscopy. The operation is more invasive, but gives a much better effect. It allows you to restore the axis of the lower limb and achieve good functional results.
Indications for knee debridement
Most often, the procedure is performed on a knee joint suffering from arthrosis. The minimally invasive procedure is also used in the area of large hip and shoulder joints. Using instrumental diagnostic methods - magnetic resonance imaging and radiography - the stage of the process is determined. The stage of destruction of cartilage tissue and the presence of pathological growths on bone tissue (osteophytes) are studied. The presence of the following symptoms is an indication for the use of debridement:
- unbearable pain in the joint area during active and night periods;
- stiffness in the morning, contracture in the joints;
- damage to cruciate ligaments, menisci;
- joint instability, habitual dislocations;
- formation of obvious lameness;
- use of additional support when moving (cane, crutch).
Debridement of the shoulder, knee and hip joints is effective only at stages 2-3 of the disease. For the 1st stage, the presence of large fragments is not typical, and for the final stage, the risk of the procedure does not justify the benefit.
How is rehabilitation carried out?
The table clearly shows the types of debridement:
| Way | Features |
| Mechanical | Special drills are used for grinding, which affects the duration of rehabilitation |
| Laser | Allows you to preserve a large number of healthy structures in the joint |
| Cold plasma | Minimal blood loss, without deep thermal tissue damage |
An arthroscope camera helps monitor all processes of the operation.
The intervention involves arthroscopy of the diseased joint under local anesthesia and includes the following steps:
- An incision in the skin over the joint.
- Inserting an arthroscope with the necessary instruments into the joint through the hole.
- Accurate assessment of the extent of damage in the bone structure.
- Identification of items to be removed.
- Removing flakes and scraps of cartilage tissue with a large-diameter needle.
- If necessary, intra-articular painless resurfacing of hyaline cartilage.
- Lavage of the joint cavity (rinsing with sterile solutions).
- Administration of drugs (NSAIDs, chondroprotectors).
- Stitching a puncture wound.
The set of therapeutic exercises must be agreed upon with a rehabilitation physician.
In the first 2-3 days after the procedure, swelling of the tissue in the incision area is considered normal. Medical advice is required in case of extensive swelling that does not disappear after 3 days. Precautionary measures include limiting the activity of the affected limb after debridement for the first time. Full range of motion is restored gradually, starting with simple exercises. The physical therapy course is individually developed by a rehabilitation physician.
Positive and negative aspects of the technique
| pros | Minuses |
| Minimally invasive method | Limited radicalism |
| Local anesthesia | Insufficient pain relief |
| Short procedure duration | Temporary fix |
| Short rehabilitation period | Possible only at the stage of gonarthrosis |
The procedure cannot cure a degenerative disease, but it significantly slows down the natural course of the disease. It is of particular importance in the treatment of joints of young, active people, athletes, and is widely used in old age, giving patients several years of pain-free functioning of the affected joint.
Debridement of the knee joint: what is it, indications and treatment
Health is a gift that cannot be measured. It cannot be purchased or received as a gift. It is priceless and incredibly desirable. Excellent health is often characteristic of a young age, when the body is full of strength and energy. It is then that all metabolic and metabolic processes work at their maximum. But the presence of trauma, a negative environment, stress or genetic predisposition can instantly change the way you feel.
So, more and more people are turning to specialists for help with the acute issue of knee pain. Yes, it is the knee joint, which is responsible for mobility and quality of life, that can fail.
Severe physical activity, injury, autoimmune and genetic diseases can deprive this extremely important joint of mobility. Fortunately, medicine does not stand still, and potions and ointments are being replaced by modern and effective methods of treatment. One of these can be called the debridement procedure.
Who might need a knee replacement?
Knee surgery may be suitable for patients who experience:
- Severe knee pain or stiffness that prevents them from performing everyday tasks and activities such as walking, climbing, getting in and out of a car, or getting up from a chair
- Moderate but constant knee pain that continues while sleeping or resting
- Chronic knee inflammation and swelling that does not improve with medication or rest
- Knee deformity where there is a noticeable arch inside or outside the knee
- Depression that occurs due to an inability to perform daily or social activities
If other available treatment options have not worked, surgery may be the best option.
Debridement of the knee joint - what is it?
Debridement means cleansing , or sanitation, in the language of a surgeon. Most often, debridement can be prescribed if arthrosis of the knee joint is detected. Since it is precisely this pathological process that causes changes in the surface of cartilage tissue. It is unlikely that it will be possible to cure the knee completely and irrevocably, but it is guaranteed to stop the destruction and restore mobility.
Debridement can be an excellent alternative to instrumental research, since with little trauma it allows a rational and thorough assessment of the degree of damage to the knee joint. The examination can be directed both locally and extensively, including the ligamentous apparatus, joint capsule, bone and cartilaginous areas.
In addition, an operation of this etiology allows:
- Repair damage caused by traumatic or mechanical impact.
- Remove loosening of cartilage tissue in the joint.
- Remove fragments of bone or cartilage tissue in chronic arthrosis.
Shoulder joint and types of arthroscopy
Arthroscopy of the shoulder joint is considered a technically difficult intervention among orthopedic traumatologists. Not all surgeons and clinics undertake it, even in Moscow, but we have extensive experience in this area, so patients with similar pathologies often come to us. Based on the results of diagnostic arthroscopy, we determine the exact location of the pathological focus, determine what treatment tactics the disease requires, and, if necessary, take biological material for laboratory testing.
Currently, we work with almost the full range of arthroscopic surgeries for a wide variety of pathologies of the shoulder joint:
- plastic surgery for injuries localized in the area of attachment of the tendon of the long head of the biceps;
- plastic surgery of various types of tendon ruptures, including chronic rupture injuries;
- removal of calcifications;
- dissection of adhesions;
- decompression of the suprascapular nerve;
- chondroplasty;
- elimination of joint instability/hypermobility;
- plastic labrum;
- osteoplastic surgery.
There are certain indications for arthroscopic interventions on the shoulder joint. To fully diagnose shoulder joint damage, an MRI examination is performed. It is important that the radiology specialists conducting the examination have sufficient experience in conducting examinations for such pathologies. The following are the main pathologies for which surgery is indicated:
- labrum injuries: Bankart injury, slap injury;
- damage or rupture of the rotator cuff;
- impingement syndrome, subacromial bursitis, supraspinatus tendonitis;
- limited mobility of the shoulder joint for no apparent reason;
- various shoulder injuries that are accompanied by tendon rupture.
Labrum injuries: Bankart injury, SLAP injury
Treatment of shoulder instability, Bankart injury
- Cost: 110,000 - 150,000 rubles.
- Duration: 30-90 minutes
- Hospitalization: 1-2 days in hospital
More details
Firm fixation of the labrum and joint capsule to the socket (glenoid) plays a key role in stabilizing the shoulder joint. A tear of the labrum in the anterior region is called a Bankart injury, and a tear in the area of the biceps tendon insertion is called a SLAP injury. There are several types of such damage. These pathologies often cause chronic pain and lead to instability of the shoulder joint or the formation of habitual shoulder dislocation. Only surgery can correct the situation.
The most effective treatment methods:
Arthroscopic refixation of the labrum (in case of Bankart injury, slap injury), tenodesis. The torn section of the articular labrum is fixed to the edge of the glenoid cavity using special anchors - absorbable or titanium.
Habitual shoulder dislocation, shoulder instability
habitual shoulder dislocation , can form . This is a condition in which joint dislocations occur with any minor injury or even sudden movement. The cause may be damage to the capsule and labrum of the joint, or defects in the articular surface of the scapula. Very often, a bone defect known as a Hill-Sachs lesion forms on the back of the humeral head.
The most effective treatment methods:
Arthroscopic stabilization of the shoulder joint. The torn parts of the labrum are fixed using anchors, and the joint capsule is additionally tightened.
Bone grafting (Latarjet operation). A part of the coracoid process, with the muscles attached to it, is transplanted into the defect area on the anterior surface of the glenoid cavity; the displaced fragment is fixed with screws.
Combined operations. Sometimes combined operations are used, when additional fixation of the joint capsule (reimplisage) in the area of the bone defect can be performed (Hill-Sachs).
Damage to the rotator cuff
Around the head of the humerus are several tendons that form the rotator cuff or rotator cuff. The cuff consists of the tendons of the supraspinatus, infraspinatus, teres minor and subscapularis muscles of the shoulder. These muscles provide both stability of the humeral head, pressing it against the glenoid cavity during abduction of the arm (initial phase) and rotation of the shoulder inward and outward. If the rotator cuff tendons (one or more) are damaged, the mechanics of the shoulder joint are disrupted, mobility restrictions occur, and pain occurs. abduction of the hand.
In case of complete tendon rupture, surgical treatment is performed - arthroscopically or minimally invasively.
The most effective treatment methods:
Rotator cuff repair
- Cost: 120,000 - 160,000 rubles.
- Duration: 30-90 minutes
- Hospitalization: 1-2 days in hospital
More details
Plasty of the rotator cuff . Arthroscopic suture or refixation of the rotator cuff tendons . The damaged tendon is isolated, stitched and fixed (refixed) to the attachment point on the head of the humerus using special anchors with a diameter of 2.5-5.5 mm and high-strength threads.
Impingement syndrome, subacromial bursitis, supraspinatus tendonitis
Part of the rotator cuff tendons passes through a narrow space formed by the head of the humerus, the tuberosities of the humerus, the inferior surface of the acromial process of the scapula, the coracoid process and the coracoacromial ligament. This space is called subacromial. This area plays an important role in arm movement, as a decrease in this space causes compression when the arm is abducted, pain and limited mobility. A typical symptom is pain when the arm is abducted 60-120 degrees.
The narrowing of the space may be a consequence of deformation of bone structures, the formation of calcifications, scarring or degenerative changes in the tendons, or bursitis.
The most effective treatment methods:
Subacromial decompression. Using special arthroscopic equipment, altered soft tissues and bursa in the subacromial space are removed; if necessary, marginal resection of the lower surface of the acromial process or the edge of the clavicle is performed.
Indications and contraindications
Most often, debridement will be prescribed by the attending physician if arthrosis of the joint is detected. Mostly the second type of this disease provides the prerequisites for prescribing this type of manipulation. Direct indications include:
- Pronounced pain during exercise and movement.
- Feeling stiff.
- Loss of mobility.
- Feelings of limping.
- Using a crutch or cane.
It is important to consider that debridement also has contraindications. Most often, the doctor will postpone the operation if there are obvious disorders of bone or fibrous etiology, or the presence of a purulent inflammatory process with the addition of an infection. The manipulation cannot be carried out if:
- There are ruptures of the ligamentous apparatus of the knee joint.
- There is damage to the capsular structure of the joint.
- Blood flow in the joint is impaired.
- There are intra-articular condylar fractures.
- There is massive hemarthrosis of the joint capsule.
Preparing for surgery
Knee arthroplasty is a major surgery, so preoperative preparation, medical consultations and physical examinations usually begin one month before the scheduled surgery date.
Preparatory and diagnostic tests will include blood tests, electrocardiograms (ECGs), and urine tests.
The operation is usually performed under general, spinal or epidural anesthesia.
During the procedure, an orthopedic surgeon will remove damaged cartilage and bone and then install a new implant made of metal, plastic, or both to restore knee function.
How is the manipulation carried out?
The intervention is carried out under anesthesia, and, importantly, under local anesthesia. an arthroscope as the main instrument , so the procedure should be more correctly called knee arthroscopy . The device is inserted through a small incision and the damaged joint is treated. First of all, minor irregularities and flakes are excised. Later, the growths - osteophytes - are removed.
Such manipulation restores the natural smoothness of the surface of the cartilage tissue, which has a beneficial effect on mobility, thereby eliminating the inflammatory process. As auxiliary procedures, lavage or additional rinsing with the use of antibacterial and anti-inflammatory drugs can be performed.
The manipulation ends with suturing. It is noteworthy that after the intervention, within a week, complete disappearance of pain and swelling is possible. Only the first days, most often 72 hours, is complete rest of the operated joint.
Therefore, when the first alarming symptoms appear in the joints, it is necessary to pay attention to health. Do not hesitate to visit a doctor and engage in self-medication, which will only increase the time for recovery. After all, it is much easier to prevent the development of the disease than to treat its advanced form and resort to radical methods.
Treatment
Conservative treatment
In almost all cases, doctors first prescribe conservative treatment. The goal of conservative treatment is to reduce pain and maintain sufficient joint function. Non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen, which can reduce swelling and pain, can be recommended for medical treatment. Various methods of physiotherapy (electrophoresis, phonophoresis, laser, etc.) are widely prescribed, which also helps reduce pain. Exercise therapy plays an important role in the conservative treatment of arthrosis, which helps preserve the functionality of the joint. In case of severe exacerbation, the use of an orthosis for a certain period of time may be recommended.
In some cases, the patient needs to change or limit physical activity, especially when it involves stress on the arm.
Cortisone injections into the elbow joint may provide temporary relief. Cortisone is a powerful anti-inflammatory drug and can be very effective in relieving pain and swelling. The effects of cortisone (or other steroids) are temporary, lasting from several weeks to months. There is a small risk of infection with any joint injection, and cortisone injections are no exception. In addition, steroids should not be administered frequently, as they themselves lead to damage to cartilage tissue.
The essence of the procedure
Most often, the debridement procedure is performed on the knees. In the process of movement, the joints experience enormous stress, as a result of which their shock-absorbing abilities are reduced and diseases arise:
- arthritis;
- arthrosis;
- gout;
- other degenerative pathologies.
When this type of illness occurs, the damaged cartilage is gradually destroyed under the influence of physical activity, and small particles peel off from it. Cartilaginous fragments fill the space between the bone joints, thereby disrupting the functionality of the lower limb and causing continuous aching pain.
Debridement of the knee joint is carried out for diagnostic examination of cartilage fragments and in order to prevent further destruction of cartilage.
The procedure is carried out using special equipment: an arthroscope and additional manipulators. Having previously made a puncture of the knee joint, a special optical device in the form of a small camera at the end of a cord is inserted into the hole. The device is inserted by a doctor into the interarticular cavity in order to examine the damaged hyaline surface and generally assess the condition of the bone articulation.
If cartilaginous debris and necrotic areas are identified, the doctor makes a second puncture and removes them from the synovial fluid with a thick surgical needle. With the help of additional manipulators, the specialist cleans out dead tissue and restores the smoothness of the surface of the cartilage as much as possible.
Arthroscopic debridement is performed under local anesthesia. This is one of the most gentle procedures in terms of surgical manipulations in the joint space. In addition, such surgical intervention makes it possible to accurately examine the intra-articular cavity and clearly determine the degree of damage to the hyaline surface.
Carrying out such an operation does not guarantee a complete cure, but the manipulations significantly increase the functional capabilities of the joint, restore the shock-absorbing properties of hyaline cartilage and stop pain in the knee area for 2-4 years.
Effectiveness of lavage
Lavage allows you to eliminate pain for a while and improves joint function by washing away dead tissue and products formed during inflammation. Since this technique does not affect the very cause of the disease, it cannot be considered a radical method of treatment. However, lavage allows you to delay surgical arthroscopy itself and gives time to prepare the body for the upcoming intervention.
There is a lot of discussion around lavage regarding the advisability of using it for certain pathologies. To make the right decision, discuss the pros and cons with a qualified doctor. At Medika, doctors with extensive experience provide consultations, receive appointments, and perform procedures. You can make an appointment with them through the request form on the website (at the top of the page there is the “Make an Appointment” button) or by calling +7(499)493-24-00.
| Rheumatologist | Price |
| Initial appointment with a rheumatologist (examination, prescribing examination and therapy) | 2000 rub. |
| Repeated appointment with a rheumatologist (examination, correction of therapy) | 3000 rub. |
| Joint puncture with injection of a drug (high-density hyaluronic acid) | 1500 rub. |
| Joint puncture with injection of a drug (low-density hyaluronic acid, alflutop) | 2000 rub. |
| Periarticular administration of the drug | 2000 rub. |
| Drug blockade of the scalene and piriformis muscles | 2000 rub. |
| Lavage of the knee joint | 5000 rub. |
When to intervene
The procedure is prescribed exclusively by a specialist and is carried out if the appropriate indicators are available. Debridement will not bring any effect in the initial stages of arthrosis development and in advanced cases of the disease. The golden mean in this matter is considered to be the 2nd stage of arthrosis, when the joint already has morphological pathologies, but the cartilage tissue is still more or less preserved.
List of symptoms in the presence of which sanitation of the knee joint is indicated:
- pain in the knee area during prolonged stay in a static position or measured walking;
- a feeling of quickly passing stiffness of the limb after sleep;
- the appearance of lameness when moving;
- needle-shaped growth of bone tissue in the articular area;
- meniscal damage;
- synovial hyperplasia;
The indication for surgery is the need to use supporting objects when moving.
What is knee replacement and why is it beneficial?
When articular cartilage becomes damaged or wears out, pain occurs and limited range of motion occurs in the joint. The joint space narrows, bone growths appear in the form of osteophytes, synovitis, range of motion sharply decreases to varying degrees and pain occurs when putting pressure on the leg; in later stages of arthrosis, deformities of the lower extremities appear visible to the naked eye.
Endoprosthetics allows you to completely get rid of joint pain.
Postoperative period
After surgery, the patient should be in a state of complete immobilization for some time.
Even minor movements are not recommended, since the areas where surgical manipulations were performed can become inflamed and cause relapse. After 2–3 days, the surgical tract (hole) heals completely. It takes more time for the joint to recover. It all depends on the degree of damage and the extent of surgical intervention.
Rehabilitation after surgery involves performing physical therapy to restore joint function. The load on the knee increases gradually and is selected individually by the doctor. Following all the recommendations of specialists will allow you to restore mobility to your knee joints.
Postoperative rehabilitation
In the postoperative period, it is recommended to limit the load, for which a plaster splint, crutches (no more than 1-2 weeks) or a fixator are used. After the stitches are removed, the patient undergoes an active rehabilitation program, including various types of exercise therapy, physiotherapy and other measures aimed at reducing swelling and restoring motor functions. If you follow the recommendations of a rehabilitation doctor, within two months patients fully recover and return to their usual active life.
Return to section: Joint arthroscopy