Plano-valgus foot deformity in a child is a pathologically acquired foot defect. This diagnosis is made in 70-80% of children. The pathology appears several months after the child begins to walk. Under the weight of the body, the foot flattens and the heel deviates outward. In rare cases, the anomaly will be congenital.
The generally accepted opinion is that in children under 3-4 years of age, plano-valgus flatfoot is physiological. The area of the longitudinal arch is filled with fatty tissue, which will disappear over time. Therefore, doctors most often make a diagnosis after this age has passed, which leads to changes that are difficult to correct. As a rule, the anomaly progresses slowly, over many years, without showing any special symptoms. Advanced flat-valgus foot deformity leads to valgus (X-shaped) positioning of the child’s legs, deformation of the ankle and knee joints, twisting of the pelvis, and curvature of the spine.
Causes leading to foot deformation
To date, the causes of the development of congenital valgus or varus of the foot have not been precisely established. According to scientists, a certain role is played by the lack of macro- and microelements in the body of a pregnant woman, especially calcium and vitamin D. The presence of the fetus in a breech position, multiple pregnancies, and oligohydramnios also increase the risk of congenital deformities of the feet and ankle joints. A healthy lifestyle is important, which the expectant mother should adhere to throughout all three trimesters.
Acquired variants of the pathology develop due to improper functioning of the musculoskeletal system or its underdevelopment. More often the disease is diagnosed in children with the following characteristics:
- were born prematurely (premature) or to mothers whose pregnancy had complications;
- received birth or other injuries, for example, a dislocated hip;
- have been or are suffering from diseases that cause changes in cartilage, bone, connective or muscle tissue, for example, rickets (vitamin D deficiency) or cerebral palsy (cerebral palsy);
- wore a cast on the lower limb for a long time;
- have weak muscles and ligaments, in particular due to lack of adequate physical activity;
- wear uncomfortable shoes that do not fit;
- suffered serious infectious diseases, especially in the first year of life;
- suffer from excess weight;
- have a genetic predisposition to the development of this pathology.
- got on their feet early and began to walk independently, by hand or with the help of special devices (walkers, etc.).
Often, varus and valgus acquired deformities of children's feet are formed due to the fault of parents. Many fathers and mothers strive to quickly put the baby in an upright position and see his first steps, “forcibly” putting him on his feet. This is a serious mistake, since the child must decide for himself when it is time for him to walk. It is also important for the baby to create all the conditions so that his naturally flat soles begin to develop correctly.
Deformation of the lower extremities in a child may be one of the manifestations of poor posture, which develops due to other reasons (injury to the neck or base of the skull during childbirth). In such cases, a visit to an osteopath will form the basis of treatment.
Depending on the causative factor, the following types of varus and valgus curvature of the lower extremities are distinguished:
- post-traumatic (after various injuries);
- structural (due to developmental anomalies of the musculoskeletal system);
- static (due to poor posture);
- spastic (the result of malfunctions of the nervous system);
- paralytic (complication of encephalitis, polio, etc.);
- compensatory (due to the structural features of the legs);
- rachitic (consequence of rickets);
- correctional (the result of incorrect treatment of other diseases of the lower extremities).
Only an orthopedic doctor can correctly determine the cause of the pathology and its degree.
Distal osteotomy
The most common surgical method for correcting hallux valgus deformity is distal osteotomy. The operation takes place in several stages:
First stage
Exostoexotomy or removal of the “bone”. In untreated cases, this stage may be the only one. Through a small skin incision or even without an incision, endoscopically, the exostosis itself (bone) and the inflamed joint capsule are removed.
Second phase.
Remote osteotomy. Using an artificial fracture, the position of the first metatarsal bone is leveled. The fracture site is secured with titanium screws. They are removed a month later, after the bone has completely healed.
Third stage.
Dissection of the muscle responsible for abducting the thumb.
Fourth and final stage.
Securing the thumb in a physiological position.
Severity and types of disease
Hallux valgus develops gradually, going through four stages of development:
- First degree. The deviation from the vertical axis is no more than 15 degrees. Timely correction leads to complete cure.
- Second degree. The lower part of the legs is turned out 15-20 degrees. Complex conservative treatment gives a good result, completely eliminating the defect.
- Third degree. The deviation from the axis is 20-30 degrees. Therapy includes a number of activities and lasts several months and even years.
- Fourth degree. The deformation angle exceeds 30 degrees. Conservative treatment does not always give a positive result, so in approximately 7% of cases surgical correction is performed.
Varus curvature has three degrees of severity:
| Degree of damage | Heel angle in degrees | Arch angle | Longitudinal arch height |
| 1 | up to 15 | up to 150 | 15-20 mm |
| 2 | up to 20 | 150-160 | 10 mm |
| 3 | more than 20 | 160-180 | less than 10 mm |
Preparation for procedures and list of contraindications
Preparation for procedures requires compliance with the rules of treatment:
- the expected thermal effects are not recommended for menstruating women;
- The skin must be washed clean and should not be lubricated with cream;
- It is better not to come to physiotherapy after physical work, on an empty stomach or immediately after eating;
- to avoid worry, empty your bladder before the session;
- inform the physiotherapist about the medications you are taking and allergic reactions; some may need to be discontinued until the end of physiotherapy;
- in complex treatment with intravenous procedures and massage, physiotherapy is performed first;
- You should not drink alcoholic beverages (including beer) during treatment; during acupuncture you should not eat spicy foods with spices;
- During the procedure, the patient lies in a relaxed, calm position.
When referring to a physiotherapy room, the doctor takes into account the patient’s age, concomitant diseases, and test results.
General contraindications for physiotherapy:
- signs of a malignant or benign tumor, condition after surgical treatment for cancer;
- blood and immune diseases, decreased clotting;
- individual hypersensitivity to paraffin, galvanic currents;
- purulent skin lesions at the site of exposure, skin diseases;
- increased body temperature;
- sudden changes in blood pressure;
- pregnancy (with acupuncture - only the second half);
- tuberculosis and infectious diseases (hepatitis, AIDS, sexually transmitted diseases);
- thrombophlebitis;
- a pacemaker in a patient is a contraindication to electrophoresis and acupuncture;
- mental disorders, drug addiction (if there is discomfort, there is a danger of inappropriate behavior);
- pain syndrome of unknown origin.
Clinical picture
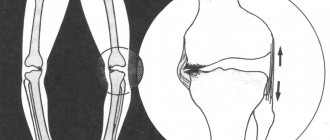
Valgus most often begins to manifest itself in the first year of a child’s life and is often combined with valgus deformity of the knee joints. It is characterized by an X-shaped curvature of the legs and a decrease in the height of the arches of the feet. If you bring your knees together and then straighten them, the distance between your ankles will exceed 4-5 cm. Being on a completely flat surface, the inside of the lower leg falls inward, and the toes and heel “look” outward. A flat-valgus foot develops with almost complete flattening of its natural arches.
Varus also begins to manifest itself in early childhood. With this pathology, the baby’s legs are O-shaped, resembling a wheel. The axis and dome of the foot are bent, with the main load falling on the outer edge of the sole. However, varus of the foot, like valgus, can be isolated and not combined with deformation of the entire lower limb.
Both deformities can be congenital or acquired. In the first case, pathological changes will be observed already during the period of intrauterine development of the fetus. A child is born with a defect. Acquired foot deformities begin to form after the baby is finally on his feet. As a rule, with foot valgus, parents notice that when the baby walks, he does not step on the entire sole, but only on its inner part.
The curvature of one lower limb may be more pronounced than the other and be combined with flat feet. If planovalgus feet are not treated, the pathology is likely to progress over time. The physiological position of the legs will change, provoking the development of diseases of the spine and large joints. Over time, poor posture will appear, which can develop into such a serious disease as scoliosis or kyphoscoliosis.
Foot valgus can be combined and even be a consequence of varus of the knee joints.
Therefore, it is so important to promptly identify defects of the lower extremities and pay attention to any signs of the disease. Parents may notice that the child's gait is unsteady and awkward, causing discomfort and pain. Swelling of the knee and ankle joints often appears. When examining the shoes, it is clear that they wear unevenly, with a lot of wear on one side of the sole.
Children with varus and valgus often complain of fatigue after walking, pain in the legs and spine, cramps in the calf muscles, and even headaches. They cannot fully run, jump, perform physical exercises or play sports. Because of this, many children develop complexes and a reluctance to go to physical education or kindergarten. Sometimes the result is depression.
Myths about surgery to remove hallux valgus
There are many myths among people regarding surgical removal of a bunion. Let's dispel some of them.
You cannot have surgery if you have arthritis or arthrosis. In fact, these diseases are considered relative contraindications. The operation is possible, the doctor will just treat you with more attention.
It is useless to operate: the bone will soon grow anyway. With a high-quality intervention, the probability of re-development of hallux valgus deformity tends to zero. Relapses occur, but are extremely rare.
You will have to sit for a long time without moving and wear a cast. Modern technologies make it possible to move independently within a few hours after the procedure. The bones are held together by special structures, so there is no need for plaster.
Diagnostics
Make an appointment Biketova Alexandra Viktorovna Osteopathic doctor Specializes in the diagnosis and treatment of pain syndromes in the cervical, thoracic, lumbar spine, chest, shoulder girdle and pelvic area, in the joints of the arms, legs, pain in the foot and heel area, numbness or swelling of the extremities, pain syndromes after operations and injuries of various ages, dysfunction of internal organs with and without pain syndrome. Consultation from 2000 rub.
If a child’s heel constantly falls in when standing and when walking, or there are other signs of deformation of the lower extremities, you should consult an orthopedic doctor.
The doctor interviews and examines the patient and prescribes standard research methods:
- radiography of ankle joints;
- podometry (the ratio of the height of the foot to its length as a percentage);
- computer plantography (sole imprint).
According to indications, additional examinations are carried out (determining the level of calcium and vitamin D in the blood, ultrasound of the knee joints, radiography of the spine, etc.). If necessary, the patient is referred for consultation to related specialists (neurologist, endocrinologist, etc.).
Operations for Hallux Valgus
Currently, a huge number of different methods of surgical treatment of Hallux Valgus are known, which indicates an unresolved problem and the absence of a universal method for treating this deformity. The most widely used techniques involve performing various osteotomies of the metatarsal bone and the main phalanx of the first toe. These techniques often make it possible to achieve the desired correction of deformity in Hallux Valgus, and to allow the patient to leave the hospital bed in a short time after surgery. In most cases, when using modern treatment methods, patients do not have plaster immobilization of their feet and there is no need to use additional support - crutches.
Patient Irina, 47 years old. Photos of feet before and after Hallux Valgus treatment
Patient Olga, 62 years old. Photos of feet before and after Hallux Valgus treatment
Video reviews about the treatment of toe deformities in our center
Patient Saurina E.L. — surgery for Hallux Valgus Patient Burkova E.D. — surgery for Hallux Valgus Patient Shestakova S. — surgery for bunions Zdorina T.V. 45 years old - removal of bones on the legs
Video about treatment of Hallux Valgus
Pavel Zhadan about the treatment of Hallux Valgus on the TVC channel
On April 18, 2013, the TVC channel aired the program “Doctor I” in which the orthopedic traumatologist P.L. Zhadan took part. The program touched upon the topic of treatment of flat feet and one of the most common orthopedic pathologies of the forefoot - hallux valgus. The program covered the causes of static foot deformities, prevention and modern methods of treating patients with this orthopedic pathology. We recommend watching the full version of the program on our website.
Treatment of varus and valgus deformities
Hallux valgus and varus deformity of the foot in children usually requires long-term complex treatment. The sooner it starts, the better the prognosis. The main goal of conservative therapy is to create a correct arch of the foot by strengthening the ligamentous-muscular framework. Classic treatment methods include:
- Exercise therapy and gymnastics with exercises for the legs, in particular, with the help of various objects;
- massotherapy;
- plastering;
- water procedures (foot baths, swimming);
- use of orthopedic shoes and insoles;
- the use of special mats, balls and similar objects;
- physiotherapeutic procedures (magnetic therapy, applications with ozokerite and others);
- osteopathy.
Sometimes orthopedic splints, bandages and other fixing devices are used to eliminate the defect. In some cases, specialists turn to alternative methods, for example, kinesiotaping of the lower limb. In case of severe clinical manifestations, symptomatic therapy is prescribed (painkillers, hormonal and other drugs). If the measures taken are ineffective, surgical intervention is resorted to.
As a rule, varus and valgus feet in children respond well to conservative treatment.
Forecasts
The formation of the foot occurs before the age of 12, so by this time it is possible to correct it, getting rid of problems. The sooner the disease is noticed and treatment begins, massage and other procedures are carried out, the greater the likelihood that the defect can be eliminated and troubles avoided.
With late detection and the beginning of correction, the risks of complications are much greater, and prognoses in moderate or severe condition are not always comforting and often end in surgical intervention.
Prevention of pathology
In order for the child’s leg to form correctly, parents should take the following actions:
- choose the right shoes for your baby, strictly in size;
- exclude any causes that may provoke the appearance of deformation;
- provide the child with adequate nutrition, a normal daily routine, and adequate physical activity including walking barefoot on any uneven surfaces;
- equip a wall bars or its equivalent in the children's room.
If parents notice that the baby’s leg is tilting to one side, or there are other signs of deformation, they should immediately consult with an orthopedic doctor.