What is hallux valgus?
Hallux valgus is a pathological curvature of the metatarsophalangeal joint of the first toe, which leads to further deformation of the other toes. In this case, the head of the metatarsal bone deviates greatly, and a protruding lump forms in the area of the lateral surface of the foot near the big toe.
Such a growth, without timely treatment, can be accompanied by pain and inflammation of the surrounding tissues, causes rapid fatigue of the legs, disrupts gait and provokes severe curvature of the spine.
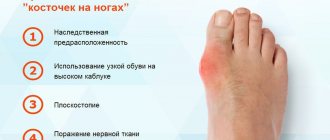
Causes of hallux valgus
Doctors identify several possible causes for the development of hallux valgus:
- hereditary predisposition;
- high load on the foot structures due to the patient’s excess weight;
- arthrosis of the joints;
- hormonal changes in the body due to menopause, pregnancy and endocrine diseases (for example, diabetes);
- long-term wearing of narrow, uncomfortable high-heeled shoes;
- high professional loads on the feet – professional sports, ballet, etc.);
- injuries and mechanical damage to the foot.
Sometimes pathology develops against the background of a combination of several of the reasons listed above.
In children, hallux valgus deformity develops due to imperfections of the tendon-ligament system and pathologies of the musculoskeletal system. The first manifestations of the pathology become noticeable to parents already by 10-12 months, when the baby tries to take his first steps. Another provoking factor may be muscle hypotension in a child.
Medical examination
Your doctor will start with a thorough physical examination of your child.
If your child is under 2 years of age, is in good health, and has symmetrical arching (the same curve in both legs), then your doctor will likely say that no further testing is needed at this time.
However, if your doctor notices that one leg is more bent than the other, he or she may recommend taking an X-ray of the lower leg. An X-ray of your child's legs while standing may show signs of Blount's disease or rickets.
If your child is older than 2 1/2 years old at the first visit and has symmetrical leg bending, your doctor will likely recommend an X-ray. Your child is more likely to have Blount's disease or rickets at this age. If an X-ray shows signs of rickets, your doctor will order blood tests to confirm the presence of the disease.
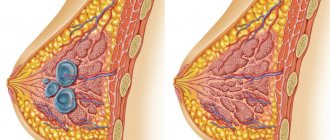
Symptoms of hallux valgus
The most obvious symptom of the development of hallux valgus is the formation of a protruding bone on the side of the foot near the big toe. In addition to this manifestation, the patient has the following symptoms:
- strong deviation of the thumb from the axis outward;
- hammertoe deformity of other toes;
- pronounced flat feet;
- severe pain in the foot, first when walking, and later at rest;
- fast fatiguability;
- inability to wear usual shoes;
- development of inflammatory processes of soft tissues and pustular skin lesions in the bone area.
Most often, patients ignore the symptoms of hallux valgus for a long time and consult a doctor only when it becomes impossible to choose suitable shoes due to a protruding bunion. At this stage of deformation, treatment with conservative methods is no longer effective. Only surgery will help eliminate the pathology.
Diagnosis of hallux valgus
An experienced orthopedic traumatologist can make a diagnosis simply by examining the foot with pathology and palpating the tissues. The joint tissue is dense, and any touch can cause pain to the patient. To confirm the diagnosis and determine the severity of hallux valgus, radiography of the feet is performed in 3 projections. Sometimes magnetic resonance imaging and plantography (footprints to identify flat feet) are used as additional diagnostic techniques.
Operation
If conservative therapy does not bring the expected results or the deformity is quite serious, then surgery is performed - corrective osteotomy. During surgery, the surgeon cuts out a bone fragment from the tibia and attaches it to the lower leg using bolts and clamps. Then osteosynthesis is performed, always using the Ilizarov apparatus.
After the operation, a long period of rehabilitation and recovery begins. The device has been worn for a long time. The duration of wearing the device is determined by the severity of the deformity. Usually this is about 2 months. The device is removed only in medical institutions by specialists. In this case, general or local anesthesia can be used.
Varus curvature is treated with great success only in the early stages of the development of the pathology. Therefore, at the first symptoms of the disease, it is necessary without hesitation to refer to the appropriate specialists for examination and diagnosis, as well as to quickly eliminate the cause of the pathology and prescribe adequate treatment.
How to prevent the appearance of a bulging bunion?
Prevention of pathology involves following simple rules:
- Attentive attention to the condition of the feet - when the first signs of increased fatigue, discomfort and inflammation of the feet appear, you must immediately contact an orthopedic traumatologist. By diagnosing the disease in the early stages, you can avoid surgery and restore the health of your feet using conservative treatment methods.
- Wearing comfortable shoes - experts recommend choosing shoes very carefully, in strict accordance with your foot size. It is also important to avoid prolonged wearing of uncomfortable shoes with pointed narrow toes and high thin heels (above 7 cm). Wearing shoes made of non-breathable synthetic materials can also accelerate the development of various foot pathologies.
- The use of orthopedic insoles - special insoles help reduce the load on the forefoot, evenly distribute the person’s weight and soften mechanical shocks.
- Regular rest - if the patient’s professional activity involves long periods of standing, it is very important to provide the feet with proper rest.
What is varus deformity of the foot in a child?
Varus deformity is a pathology of the foot that causes deformation of the middle part of the legs with outward deviation. In this case, the patient has a characteristic O-shape of the legs. This pathology develops against the background of improper distribution of loads on the joints of the body - knee, hip, etc. The main factor provoking the pathology is compression of the internal meniscus.
This, in turn, reduces the internal condyle of the femoral bones, but enlarges the external one, which increases the load on the knee joint. With varus deformity of the foot, its outer part is in an overloaded state, which leads to further distortion of other parts of the body and curvature of the spine.
The pathology usually develops in childhood. The O-shaped shins are also popularly called clubfoot. In the absence of timely treatment, varus deformity of the foot can lead not only to severe diseases of the musculoskeletal system, but also to psychological problems in the child.
Therapeutic rehabilitation of children in the first year of life
Therapeutic physical education (PT) for children with congenital clubfoot is indicated from the first days of life against the background of general orthopedic treatment. It is at the age of 7-10 days that it is possible to effectively influence the ligamentous-muscular system of a small child.
An integrated approach to exercise therapy includes the gradual impact of corrective plaster casts. The so-called positional treatment is carried out, which is supported by a special massage. After removing the cast, the massage therapist performs gymnastics for the feet and legs, and then re-fixes the position with a corrective splint.
A set of massage procedures should ensure complete relaxation of the muscles of the foot and lower leg. For this purpose, stroking, vibration, kneading, shaking the muscles, and stretching the tendons of the heels are used.
After a relaxing massage, muscle tone decreases, and the massage therapist conducts the next stage of therapeutic rehabilitation - physical gymnastics:
- The starting position of the child is lying on his back . The goal is to eliminate external adduction of the foot. We consider the work of a massage therapist with the right leg. The ankle is pressed with the left hand, with the first finger on the outer ankle and the second on the inner ankle, so that the baby’s heel lies in the palm of the massage therapist. Grasping the foot with your right hand, the first finger on the outer edge, the bent second finger of the masseur on the back of the limb, and the third finger on the inner surface, we move the child’s foot outward. The same is done with the left.
- The starting position is the same . The goal is to eliminate rotation of the foot relative to the longitudinal axis. The massage therapist covers the child’s right foot with his right hand, placing the first toe on the sole and the others on the back. With the second hand, grasping the heel firmly fixes it. The massage is performed by pressing the first finger from bottom to top on the outer edge of the baby’s limb, and from top to bottom the massage works on the inner edge.
- The starting position does not change . The goal is to eliminate plantar flexion. The masseur's right hand presses the child's left shin to the table, resting the first and second fingers on the ankle. The massage therapist's left hand presses the sole of the foot with the palm moving from bottom to top.
This complex of physical therapy and massage with repetition of each movement 3-5 times can be carried out independently.
Parents only need to undergo training from a massage therapist-physical therapy instructor to engage in physical education with their child at home every day for five sessions.
Another effective therapeutic and preventive intervention will be swimming and water gymnastics. The described massage procedures can be performed in a bath at a water temperature of 36-37 ºС. Warm, comfortable water will promote spastic muscle relaxation.
Causes of development of varus foot deformity
The pathology may be congenital or acquired. The cause of acquired varus deformity of the foot in adulthood is usually Paget's disease, accompanied by damage to the tibia and femur. Prolonged immobilization of the limbs after severe injuries can also lead to the formation of pathology.
Most often, varus deformity is congenital and manifests itself in early childhood. The following additional factors lead to aggravation of the condition:
- the child wearing uncomfortable shoes that compress the foot;
- transmission of severe infectious diseases, including influenza;
- severe forms of vitamin deficiency, primarily associated with a lack of vitamin D and calcium in the body;
- pathologies of bones and joints;
- severe endocrine diseases;
- excessive stress on the legs;
- injuries and mechanical damage to leg tissue.
Rickets
Rickets
is a disease in children that affects the bones and causes bowed legs and other bone deformities. Children with rickets do not get enough calcium, phosphorus or vitamin D, which are important for healthy bone growth.
Dietary rickets is unusual in developed countries because many foods, including dairy, are fortified with vitamin D. Rickets can also be caused by a genetic abnormality that prevents vitamin D from being absorbed properly. This form of rickets can be inherited.
Symptoms of foot varus deformity
Symptoms of varus deformity can develop very slowly, which leads to a long, uncontrolled course of the disease. Due to improper distribution of the load on the spine and joints, this can lead to severe pathologies of the musculoskeletal system.
Symptoms of varus deformity that can be seen visually:
- external changes in the shape of the legs - O-shaped shin;
- the formation of a characteristic varus foot - the inner arch is high, and the heel of the foot is deviated inward;
- changes in gait, frequent loss of balance and falls;
- foot fatigue syndrome;
- discomfort when putting on and wearing shoes.
If such symptoms appear in a child, you should consult an orthopedic traumatologist as soon as possible.
Dislocation in the knee joint
Congenital pathology of dislocation in the knee joint and, as a consequence, varus deformity of the tibia in children is a rather rare orthopedic disease.
According to statistics, pathology is 3 times more likely to be detected with unilateral deformation than with bilateral O-shaped curvature of the lower extremities.
In girls, orthopedic congenital manifestations also occur 3 times more often than in boys. Varus deformity of the tibia is observed when the proximal end of the tibia is displaced forward.
The causes of the clinical condition are considered to be congenital dystrophy or a disorder of cellular metabolism in the quadriceps femoris muscle as a result of intrauterine damage to the osteoarticular structure of the fetus.
According to some medical experts, this intrauterine situation occurs due to the incorrect position of the fetus in the mother's womb, when the hip joints are bent and the knee joints, on the contrary, are straightened.
Diagnosis and prevention of varus foot deformity
Usually a visual examination is sufficient to make a diagnosis. If the specialist needs additional information, an x-ray examination of the lower extremities is prescribed. Another informative study for varus foot deformity is magnetic resonance imaging.
The following rules help prevent the development of varus deformity:
- wearing comfortable shoes that match your foot size;
- complete nutrition containing all the vitamins and microelements the body needs;
- preventing overwork of the lower extremities;
- timely visit to an orthopedist for preventive purposes.
Treatment and rehabilitation of hallux valgus
Treatment of hallux valgus in the initial stages of bunion formation can be carried out using conservative methods - therapeutic exercises, physiotherapy, wearing orthopedic shoes, adherence to a work-rest regime. If the pathology develops in adulthood, treatment involves surgery.
Surgery to remove a bunion can be performed in two ways:
Classic surgical technique
In this case, the operation is performed under general anesthesia or under epidural anesthesia. The specialist cuts through the soft tissue, gains access to bone and joint structures and removes the growth on the bone. In some cases, the surgeon has to partially remove the phalanx of the big toe or even perform prosthetics of the foot joints. In this case, the patient's own joints are excised and replaced with prostheses.
Rehabilitation after surgery is complex and lengthy. The patient cannot walk for the first days after surgery. Then, for several months, the patient cannot lean on the operated leg. The patient moves only with the help of crutches or a stick.
To speed up the recovery of motor activity, therapeutic exercises, physiotherapy and massage are used. Only after a few months (4-6) the patient can return to normal life and wear familiar shoes. At the same time, experts recommend that such patients give preference to orthopedic shoes and avoid heels and models with narrow toes.
Laser technique for removing a bunion on the leg
Experts consider the laser method of treating hallux valgus to be the most gentle and minimally invasive. The operation can be performed under spinal and intravenous anesthesia, which reduces the overall burden on the body.
The surgeon makes a small tissue incision in the area where the protruding bone forms and removes the growth using a directed laser beam. The laser evaporates cells layer by layer, forming a healthy shape of bone and joint structures. After the operation, several small cosmetic sutures are placed at the incision site, which are removed 10-12 days after the operation.
An important advantage of the laser method for removing hallux valgus is the absence of the risk of bleeding due to coagulation of blood vessels under the influence of the laser beam. In addition, the laser has bactericidal activity, which prevents infection of the wound surface.
Recovery after laser treatment of a bunion on the leg is much easier and faster than after classical surgery. Already on the second day the patient can walk without crutches and additional support.
After 2-3 weeks, wearing shoes without heels is allowed, and after 2 months the patient can return to normal physical activity. Moreover, due to the low invasiveness of the surgical method, the tissues quickly heal and are restored, excluding relapse of the pathology.
Department of Traumatology and Orthopedics
article in PDF format
ON THE. Gear1, A.M. Matsakyan2, V.G. Protsko3
1Federal State Autonomous Educational Institution of Higher Education First Moscow State Medical University named after. THEM. Sechenov (Sechenov University) Ministry of Health of the Russian Federation, Moscow 2GKB named after. A.K. Eramishantsev DZM, Moscow 3GKB named after. S.S. Yudina DZM, Moscow
Summary: Currently, varus deformity of the feet is considered one of the most common diseases of the foot and ankle joint. With this type of deformity, the foot has a characteristic hemilateral curvature, which is accompanied by inward deviation of the forefoot and the development of clubfoot.
The purpose of this study is to improve the results of surgical treatment, analyze the system of surgical treatment techniques and develop an algorithm for selecting the most optimal surgical treatment options for the 3rd stage of development of polovarus foot deformity.
We have summarized the clinical experience of surgical treatment of 145 patients with grade 3 polovarus foot deformity, who underwent 177 surgical interventions.
Analysis of the long-term results of surgical treatment showed that an individual approach to such severe deformities, depending on the involvement of the foot, a combination of operations on both bones and soft tissues, ensured a favorable course of the postoperative period and an earlier start of rehabilitation.
Key words: polovarus deformity, osteotomy, arthrodesis, foot.
SURGICAL METHODS OF CORRECTION VARUS DEFORMITY OF THE FOOT 3 DEGREES
Shesternya NA1, Matsakyan AM2, Protsko VG3
1I.M. Sechenov First Moscow State Medical University (Sechenov University), Ministry of Health of Russia 2Municipal Clinical Hospital named after AK Eramishancev, Moskow 3Municipal Clinical Hospital named after SS Yudin
Summary: Currently, varus deformity of the foot is one of the most common in the structure of diseases of the foot and ankle. With this type of foot deformities has a characteristic curvature that is accompanied by deviation of the forefoot inside and to the development of clubfoot. e purpose of this study is to improve the results of surgical treatment, the analysis of methods of surgical treatment and testing of the algorithm for choosing the best options in the surgical treatment of 3rd stage of development proviruses of deformity. We summarized the clinical experience of surgical treatment of 145 patients with a varus feet deformity of 3 degrees, which made 177 surgical interventions. Analysis of remote results of surgical treatment showed that an individual approach in such severe deformities, depending on the involvement of the foot, the combination of operations on the bones and so tissues, provided a favorable postoperative period and an earlier start of rehabilitation.
Key words: varus deformity, osteotomy, arthrodesis, foot.
Introduction
Currently, varus deformity of the feet is considered one of the most common diseases of the foot and ankle joint [1, 4, 10]. With this type of deformity, the foot has a characteristic planovarus curvature, which is accompanied by inward deviation of the forefoot and the development of clubfoot. In addition, this type of deformity is characterized by an O-shaped shape of the legs, in which the legs have an external convexity, and in the most severe cases, an outward displacement of the thigh develops [3, 5, 7, 9].
Varus deformity of the feet can be either congenital or acquired. The main causes of varus deformity of the feet are various metabolic disorders, as well as various diseases of the skeletal system, as a result of which the strength of bone tissue is impaired [2, 6, 8].
The complex anatomical and functional features of the foot and the high incidence of polovarus deformity in the population determine the relevance of the development of surgical methods for treating this type of pathology. This paper presents our experience in the surgical treatment of grade 3 polovarus foot deformity.
Characteristics of patients and surgical interventions performed
We have summarized the clinical experience of surgical treatment of 145 patients with grade 3 polovarus foot deformity, who underwent 177 surgical interventions. The characteristics of the operated patients by gender and age are shown in Table 1.
All patients underwent comprehensive diagnostic measures, which included a clinical examination and radiography. A number of patients underwent electroneuromyography as part of an additional examination. In addition, the study of neurological status, MRI results, myelography, arteriography, and genetic research helped substantiate the diagnosis for most patients.
When choosing a method of surgical treatment, the criteria given in Table 2 were used.
Depending on the location and nature of the polovarus deformity, different types of surgical interventions were performed (Table 3).
Metatarsal V-shaped osteotomy
The hollow foot in the middle section at the level of the talonavicular and calcaneal-cuboid joints or at the level of the navicular-cuneiform joint (depending on the degree of rigidity of the deformity) was subjected to surgical intervention: plantar fasciotomy in combination with calcaneal osteotomy or metatarsal osteotomy. This procedure made it possible to restore optimal support to the foot.
An anterior wedge osteotomy of the tarsal region was also performed. The technique of this operation was described by Japas. It is important that the tip of the sharp wedge is at the level of the highest point of the arch of the foot deformity. This usually occurs on the scaphoid bone. In this case, the side of the wedge on the medial side passes through the first sphenoid bone, and on the lateral side - through the third sphenoid and cuboid, respectively. Bone tissue is not excised. The proximal edge of the distal foot was sunk plantar while the metatarsal heads were elevated dorsally, correcting the deformity and lengthening the plantar surface. Hindfoot deformity has been corrected in some cases by Dwyer osteotomy or triple arthrodesis.
The operation in some cases is supplemented by resection arthrodesis of the calcaneocuboid joint and plastic surgery of the posterior tibial tendon. Below is a variant of a V-shaped metatarsal osteotomy in combination with a calcaneal osteotomy.
Patient Shch., born in 1971. Case history No. 9852. Diagnosis: Polovarus deformity of the left foot. Arthrosis of the subtalar joint.
The operation was performed on June 4, 2013. Anesthesia was spinal. The operation was performed under a pneumatic tourniquet. Access to the calcaneus is from the outer side, 6 cm long. An oblique osteotomy of the calcaneus was performed using an oscillatory saw. Then the calcaneal tuberosity was lateralized by 1 cm. The calcaneal bone fragment was fixed with Ikos screws.
In the projection of the scaphoid bone, a longitudinal soft tissue incision 4 cm long was made. The talonavicular and scaphoid-sphenoid joints were isolated. A V-shaped osteotomy was performed and fixed with shape memory clamps. The wounds are sutured layer by layer (Fig. 1-5).
Resection arthrodesis of the calcaneocuboid joint
Resection arthrodesis of the calcaneocuboid joint is the operation of choice for severe varus deformity of the feet. Due to resection, a bone tissue defect appears, the forefoot shifts outward, as a result of which the longitudinal arch of the foot drops.
A longitudinal incision is made in the area of the calcaneocuboid joint, and the bones are exposed using a blunt or sharp method. Next, a wedge-shaped osteotomy is performed using an oscillatory saw. Options for fixation after resection can be different: screws, shape memory clamps (Fig. 6, 7).
Resection of the calcaneocuboid joint, removal of the scaphoid, triple arthrodesis
The third option for osteotomy of bones in the metatarsal part of the foot is a combination of resection of the calcaneocuboid with removal of the navicular bone and triple arthrodesis. All this makes it possible to form a normal arch of the foot and rigid fixation in the osteotomy areas (Fig. 8, 9).
Metatarsal osteotomies in combination with soft tissue operations
In stage 3 foot deformity, metatarsal osteotomies often have to be supplemented with soft tissue operations. The big problem at this stage is the tibialis posterior tendon. Usually it is highly developed, thickened in diameter, and strongly stretched. We lengthened this tendon, both openly and endoscopically, and transplanted the tendon to a more advantageous position to correct the deformity. We have received a patent for endoscopic operations on this tendon. With endoscopy, it is possible to perform tendon lengthening, debridement to eliminate tendovaginitis, minimally invasive tendon release, etc.
A) open lengthening of the tibialis posterior tendon
The stages of open lengthening of the tibialis posterior tendon are illustrated in Figures 10 and 11.
B) Endoscopic lengthening of the tibialis posterior tendon
We have developed a technology for endoscopic lengthening of the tibialis posterior tendon (Fig. 12-16). The advantages of this operation technique include reducing the risk of complications due to the low invasiveness of the operation and the small size of the wounds (in known techniques, an incision of 7-10 cm is made, which increases the risk of soft tissue trauma). In the developed technique, the incision does not exceed 3 cm, which significantly improves the conditions for wound healing and rehabilitation; reducing rehabilitation time due to stable static stabilization. Since with transposition of the tendon and fixation in the bone according to the developed method, the stability of fixation of the talonavicular joint is much higher, the load on the leg in the postoperative period began after 2-3 weeks, while when performing the operation using traditional methods, the load is possible only after 4-5 weeks.
Operation technique
1. A minimal incision (3-4 cm) is made in the area of attachment of the posterior tibial tendon to the scaphoid bone, the tendon is visualized, and then an endoscope is inserted.
2. Under endoscopic control, the tendon is visualized over a length of about 5 cm.
3. The tendon is bifurcated along its entire length using a puncture needle (divided in half), after which one part of the tendon in the proximal section is cut off with a scalpel.
4. Using an arthroscopic hook, the severed half of the tendon is brought out into the wound.
After this, the tendon is sutured with a Z-shaped seam, and its lengthening by 3-4 cm is achieved.
B) Minimally invasive tendon transfer of the tibialis posterior muscle to the dorsum of the foot
In this case, the SZBBM is endoscopically isolated for 5-6 cm, after which the tendon is brought out to the anterior surface of the leg.
Next, the attachment site is formed on the dorsum of the foot, after which the tendon is subcutaneously brought to a new attachment site in the area of the wedge-shaped bones and fixed with an anchor or biodegradable screw. This operation can be performed in combination with various metatarsal osteotomies.
For paresis of the peroneal muscles, the transfer of the tendon of the tibialis posterior muscle to the dorsum of the foot was combined with the transfer and suturing of the tendon of the peroneus longus muscle to it (Bridle operation) (Fig. 19).
results
Treatment results were assessed 12 months or more after surgery (Table 4).
Clinical evaluation criteria: range of motion of the foot, limb function, pain and patient satisfaction. The dependence of the treatment result for grade 3 polovarus foot deformity was noted. on the severity of the midfoot deformity, heel supination, on the degree of damage to the tendon complex, as well as the gender and occupation of the patients. The surgical technique and the adequacy of its application were important.
It is important to note that it is initially impossible to obtain ideal foot function with grade 3 deformity. Our goal was to restore the support ability of the foot, relieve pain, and make it easier to select shoes.
Note that in most cases (70%) the results of surgical treatment were assessed as excellent or good. 2.3% of unsatisfactory results were associated with the initial severity of foot deformity and technical difficulties during operations, as well as patient violation of the postoperative treatment regimen.
Conclusion
Analysis of long-term results of surgical treatment showed that an individual approach to such severe deformities, depending on the involvement of the foot, a combination of operations on both bones and soft tissues, ensured a favorable course of the postoperative period and an earlier start of rehabilitation.
Thus, a differential approach to the choice of surgical intervention technique for polovarus foot deformity is accompanied, in general, by good and excellent results of surgical treatment.
For citation
Matsakyan A.M., Shesternya N.A., Protsko V.G. Surgical methods for correcting grade 3 polovarus deformity of the foot // Department of Traumatology and Orthopedics. No4(30). 2021. p.-48.
Matsakyan AM, Shesternya NA, Protsko VG Surgical methods of correction of varus deformity of the foot 3 degrees // e Department of Traumatology and Orthopedics. No4(30). 2021. p.-48.
List of references/References
1. Zyryanov S.Ya. Result of replacement of bone and soft tissue defects of the hindfoot in post-traumatic flatfoot / Zyryanov S.Ya., Soldatov Yu.P., Zyryanov S.S. // Genius of orthopedics. 2011.-No4. - With. 126-127. .
2. Kozhevnikov O.V. Comparative assessment of the results of complex and conservative treatment of planovalgus foot deformity in children / Kozhevnikov O.V., Kosov I.S., Ivanov A.V., Gribova I.V., Bolotov A.V. // Bulletin of Traumatology and Orthopedics named after. N.N. Priorova. 2015.-No2. - With. 22-24. .
3. Koryshkov N.A. Surgical correction of the pathological position of the foot and ankle joint / Koryshkov N.A., Levin A.N., Khodzhiev A.S., Sobolev K.A. // Bulletin of Traumatology and Orthopedics named after. N.N. Priorova. 2013.-No.1. - With. 74-75. .
4. Privalov A.M. Surgical correction of severe secondary deformity of the forefoot / Privalov A.M. // Bulletin of Traumatology and Orthopedics named after. N.N. Priorova. 2014.-No.1. - With. 84-85. .
5. Reutov A.I. Features of orthograde standing in patients with post-traumatic osteoarthritis of the ankle and talocalcaneal joints / Reutov A.I., Davydov O.D., Ustyuzhaninova E.V. // Genius of orthopedics. 2013.-No4. - With. 48-52. [Reutov AI Peculiar properties of orthograde standing in patients with posttraumatic osteoarthrosis of the ankle and talocalcaneal joints. / Reutov AI, Davydov OD, Ustyuzhaninova EV // Genii ortopedii. 2013.-No4. – s. 48-52. RUS].
6. Reutov A.I. Classification of the functional state of the musculoskeletal system in patients with shortening and deformities of the lower extremities / Reutov A.I. // Vestn. traumatology and orthopedics of the Urals. 2012.-No3-4. - With. 65-69. . Usoltsev I.V. Surgical treatment of severe forefoot deformity / Usoltsev I.V., Leonova S.N., Kosareva M.A. // Bulletin of Traumatology and Orthopedics named after. N.N. Priorova. 2015. -No3. - With. 84. [Usol'tsev IV Operativnoe lechenie tyazheloi deformatsii perednego otdela stopy / Usol'tsev IV, Leonova SN, Kosareva MA // Vestnik travmatologii i ortopedii im. NN Priorova. 2015.-No3. – s. 84. RUS].
7. Shchurov V.A. Functional state of patients with varus deformity of the lower extremities of various etiologies / Shchurov V.A., Novikov K.I., Dolganova T.I. // Genius of orthopedics. 2012. - No.3. - With. 122-125. .
9. Patrick N. E ects of Medial Displacement Calcaneal Osteotomy and Calcaneal Z Osteotomy on Subtalar Joint Pressures: A Cadaveric Flat-foot Model / Patrick N, Lewis GS, Roush EP, Kunselman AR, Cain JD // J Foot Ankle Surg. 2021.-No6. - R. 1175-1179. PMID: 27545512.
10. Wiewiorski M. Computed Tomographic Evaluation of Joint Geometry in Patients With End-Stage AnkleOsteoarthritis / Wiewiorski M, Hoechel S, Anderson AE, Nowakowski AM, DeOrio JK, Easley ME, Nunley JA, Valderrabano V, Barg A // Foot Ankle Int. 2021. - No6. - R. 644-651. doi: 10.1177/1071100716629777 PMID: 26843547.
11. Koryshkov N.A., Levin A.N., Kuzmin V.I. Tactics for the treatment of equine excavatus deformity of the feet in adults // Department of Traumatology and Orthopedics. 2021.No4(20). pp. 37-43 [.., Levin AN, Kuzmin VI // e Department of Traumatology and Orthopedics. 2021. No4(20). p.37-43 RUS].
Author information
Shesternya Nikolay Andreevich – Doctor of Medical Sciences, Professor of the Department of Traumatology and Orthopedics of the Institute of Postgraduate Education. Email: [email protected]
Matsakyan Artak Matsakovich – City Clinical Hospital named after. A.K. Eramishantseva DZM, Moscow. E-mail, Moscow, 115612, st. Brateevskaya, 23-1-55, Tel. +7 (915)141 11 44.
Protsko Viktor Gennadievich – State Clinical Hospital named after. S.S. Yudina DZM, Moscow. Email
Information about authors
Shesternya Nikolaj Andreevich – PhD, prof. of the Department of Trauma and Otrhopedics of Sechenov University, IM Sechenov First Moscow State Medical University (Sechenov University), Ministry of Health of Russia,
Matsakyan Artak Macakovich – Municipal Clinical Hospital named a er AK Eramishancev, st. Brateevskaya, 23-1-55, Moskow, Russia, 115612, Phone +7 (915) 141 11 44,
Protsko Viktor Gennadievich – Municipal Clinical Hospital named a er SS Yudina, Moscow