We can talk about pain in the arm (brachialgia) with glenohumeral periarthrosis and epicondylosis (dystrophic form of brachialgia), with the syndromes of the anterior scalene, pectoralis minor muscle and shoulder-hand syndrome (vascular-neural form of brachialgia), with compression-radicular syndromes (compressive-radicular form of brachialgia), irritation from the spinal motion segment (sclerotomy form of brachialgia). However, it is advisable to diagnose the syndrome itself, and not the form of brachialgia. This is both more specific and more informative for treatment. We should talk about brachialgia when there is pain and dystrophic disorders in the arm, but it is not possible to identify a defined syndrome. Thus, vertebrogenic reflex brachialgia syndrome is diagnosed in the absence of other specific compression or reflex symptom complexes of osteochondrosis.
Referred pain can spread from the cervical spine to the entire arm and to individual parts of it. The same reflected - reflex - can be not only pain phenomena, but also muscular-tonic, neurodystrophic and neurovascular changes in the arm area. Since all these changes are accompanied by pain, it is convenient to define them as brachialgia.
This term also emphasizes that we are not talking about radiculargia, not about neuralgia, but about a pain syndrome in the arm area, which cannot be associated with damage to any individual roots or nerves. We are talking about changes in the tissues of the hand themselves, accompanied by pain and soreness. although their initial source is the cervical region, that is, the vertebral focus. Many forms of brachialgia associated with the cervical dystrophic process of the spine can occur independently of it under the influence of local macro- and microtrauma.
General information
In the medical literature, shoulder-hand syndrome occurs under various names:
- Steinbrocker syndrome
- cervico-vertebral syndrome,
- glenohumeral arthritis,
- subacromial bursitis,
- cervicobrachial syndrome,
- cervical rib syndrome,
- scalenus syndrome,
- abduction syndrome,
- sympathetic trophoneurosis, etc.
In the development of the syndrome, great importance is attached to infection (influenza), intoxication, metabolic disorders, endocrine disorders, prolonged microtrauma, and physical stress. Probably, the development of this syndrome is based on neurovascular reflex mechanisms that arise as a result of the combined influence of various etiological factors.
The onset of the disease is acute or subacute. Pain in the shoulder joints occurs both during movement and at rest, especially at night. The pain radiates to the shoulder blade, neck, head, arm. Spontaneous pain often occurs at night. Swelling, pain, and limited movement appear in the joint area. Usually after 1-2 months the hand becomes involved in the pathological process. The local temperature rises periodically. Skin color is purple with a bluish tint. Movements are significantly limited. On palpation, fluctuation and pain are noted. The consequence of swelling is deformation of the fingers. In the area under the brachial plexus, in the supraclavicular fossa, in the upper edge of the scapula, where the suprascapular nerve passes, pain is detected. Due to severe pain in the shoulder joint, restriction of movements occurs (initially adduction and internal rotation).
Epicondylosis
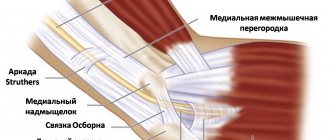
Sometimes pathological impulses are aimed at the areas of the epicondyles of the shoulder. With healthy tissues in this zone, the degenerative peripheral process may not be realized in this zone. Nevertheless, in the practice of treating cervical vertebrogenic syndromes, it occurs quite often, since in the area of the external epicondyle of the shoulder there are relatively vulnerable osteo-fibrous tissues. They are both bradytrophic and very, very overloaded, especially with repeated jerky movements of pro- and supination. Trophism is more quickly disrupted at the site of attachment to bony protrusions. Of course, they are the most vulnerable.
The clinical picture of epicondylosis is poor in local symptoms. The main symptom is pain and tenderness in the area of the epicondyle, most often the external one, but not itself, but the more distal zone of attachment of the brachioradialis muscle to it; spontaneous cerebral pain is very intense, often with a burning tinge. They intensify with jerking movements in the elbow or hand, with rotation of the forearm, especially with an outstretched arm, for example when fencing, playing tennis, while preparing chops, when working with a hammer or sledgehammer. Characteristic muscle weakness is detected by the following techniques. Thompsen's sign: when trying to hold a clenched fist in a position of dorsiflexion, the hand quickly drops.
Welsh's sign: simultaneous extension and supination of the forearms on the affected side is delayed. Dynamometry reveals weakness on the affected side. The pain intensifies when you place your hand behind your lower back.
So, epicondylosis in cervical vertebrogenic pathology is part of a wide range of neurodystrophic phenomena in the places of attachment of fibrous tissue to bone protrusions. These phenomena occur under the influence of impulses from the affected spine or (less often) other lesions of nearby tissues. The formation of one or another pathological syndrome is determined by the background state of the periphery, where the substrate was prepared. And this is created by local micro- and macrotraumas, proprioimpulses during jerking movements and overexertion. The experience of sports medicine clearly indicates the significance of the corresponding overloads (“tennis elbow”, “fencing epicondylosis”). All overloads are asymptomatic until the “attraction” of pathological impulses from the altered receptors of the spine occurs in a given dominant focus.
Causes
The syndrome does not arise just like that, but its appearance is just a reflex reaction of the body during myocardial infarction, traumatic damage to the shoulder and other joints of the arm, or spinal osteochondrosis. The main factor in the appearance is a violation of trophism or ischemia of certain areas of the spinal cord. Sometimes the syndrome can appear several years after injury or injury.
The disease begins to manifest itself after 50–60 years and very rarely occurs at a young age. It is especially common as one of the manifestations of osteochondrosis, so patients with this disease should be regularly examined in order to identify the first signs at the earliest stage.
A sore shoulder can become impingement syndrome
Many people suffer from shoulder pain. Faced with this, many people “sin” their joints, sometimes requiring treatment of the back muscles.
Meanwhile, such pain is not always inflammation and joint disease. Sometimes this indicates negative changes in the moving zone. This area is located between the acromion and the cuff of the shoulder joint. What do the changes mean? The space under the acromion is minimized. As a result, inflammation occurs. The affected ozone is the joint capsule. And all this is called impingement syndrome.
What kind of painful syndrome is this: the most common causes of the disease
IS is a serious disease. It has its reasons. For the syndrome to develop, the following negative phenomena must be present. So, the reason may be a person’s professional activity. At risk are people who carry heavy physical loads, those who are often forced to hold their arms above their heads. This is a specialty such as installers, painters, finishers.
Athletes playing volleyball, basketball, badminton. If a person is involved in strength sports, pressing dumbbells or discs, this can also be the cause of the disease.
Impingement may occur as a result of accidents, tendon injuries, arthrosis of the shoulder joint, or calcific tendinitis.
If a person has to raise his arm above his head slightly to the side, he may feel unpleasant, strong painful sensations. And if he needs to do work with his hands raised, then this becomes completely impossible. Because the victim is in extreme pain.
For the distance between the rotator cuff and the acromion to narrow and cause pain, the development of symptoms and certain factors are required. Today doctors talk about the types of impingement syndrome into which the disease is divided.
Functional. If the work of the brachial muscle extends to the shoulder cuff, IS begins to appear. After all, muscle control is not ensured. And although there are no muscle diseases, they are healthy, nevertheless, the syndrome develops.
Structural. The narrowing of the distance may also appear due to other changes. With this type, changes occur in tendons, ligaments, and bones. They suffer from joint capsules. The cause may be chronic inflammation or thickening of the ligaments. Also - subacromial spurs can be affected, as well as wear and tear of the acromioclavicular joint.
The disease and its symptoms
There are a lot of tendons in the human shoulder that are closely connected to each other. The largest number of them is located under the acromion. And painful sensations may appear if you move your hand one way or another.
Tendons become pinched or ruptured – the person experiences pain. This can happen due to intense physical activity and certain postures (arms above your head).
Inflammation persists and other symptoms may occur.
If the synovial bursa between the rotator and acromion is irritated, the person will experience pain at night. And these sensations will greatly torment the patient, depriving him of sleep in a certain position.
Also, a sore shoulder will limit a person’s movements. The shoulder will move poorly and cause discomfort until the symptoms go away. In medicine, this condition is called frozen shoulder. And such pain can become chronic.
Treatment of the inflammatory process
If the disease is at an early stage, then several measures are sufficient:
Firstly, these are gymnastics and exercises aimed at prevention. Of course, you will need painkillers and drugs that act to extinguish the inflammatory process. You need to do injections.
A sore shoulder needs rest and rest; you should not make painful movements: lifting and twisting your arms.
You can't start a disease. If symptoms appear and the disease is diagnosed, immediate treatment measures must be taken. If this is not done, it will be difficult to sleep at night, the disease will become chronic, and it will be difficult for the person to rotate his arm or lift it. Hands become weak. Doctors may observe rotator cuff tears and joint stiffness.
If the disease develops, prompt surgical assistance will be needed.
The final treatment will be prescribed by specialists.
They analyze the causes, possible and optimal treatment methods. Doctors may prescribe conservative treatment. This may also include physical therapy, shock wave and ultrasound treatments. Doctors may also recommend courses of massage and thermotherapy. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Symptoms of shoulder-hand syndrome
Symptoms of shoulder-hand syndrome (Steinbrocker syndrome) are:
- severe, burning pain in the shoulder and hand, not relieved by analgesics,
- reflex contracture of the muscles of the shoulder and wrist joints with pronounced autonomic-trophic disorders, especially in the hand area.
- the skin on the hand is swollen, shiny, smooth, sometimes with erythema on the palm or acrocyanosis of the hand and fingers.
Over time, muscle atrophy, flexor contracture of the fingers, osteoporosis of the hand (Sudeck atrophy) develop, and partial ankylosis of the shoulder joint is formed.
Clinical picture
The disease begins to develop gradually and most often is one of the manifestations of glenohumeral perarithrosis. The shoulder joint is primarily affected - patients complain of its stiffness. After this, the pathological process is diagnosed in the hand area. It also happens the other way around - the hand is affected first, then the shoulder. And finally, in very rare cases they are affected at the same time.
The main symptom is severe pain that does not go away even after taking strong analgesics. The second equally important symptom is contracture of the muscles of the shoulder and wrist joints, and sometimes the hand.
Stages of the disease
The first stage lasts from 3 months to six months. It is characterized by the following symptoms:
- Shoulder pain.
- Pain in the hand.
- Severe and constant tension in the forearm muscles.
- Restricted mobility of the joints of the affected hand.
- Stiffness of the hand and fingers.
- Tendon reflexes on the hand are increased, well-defined swelling appears, and acrocyanosis may appear - a blue tint to the skin of the fingers.
The second stage can last up to 6 months. At the same time, pain and swelling become less significant, and sometimes disappear completely. However, trophic disorders begin to appear. The coolness of the hand is noteworthy. X-ray examination reveals signs of osteoporosis.
The third stage sometimes lasts for several years. Here the main symptom is contracture, which turns into stiffness of the shoulder and fingers, and this is an irreversible process. There is muscle atrophy, osteoporosis, and a strong decrease in the local temperature of the skin of the hand.
Diagnostics
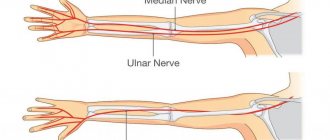
Pain, numbness, pins and needles and disturbances in arm movement can be caused not only by compression of the nerves in these bone canals. There are also diseases of the brachial plexus, spinal hernias, muscle tightness and other conditions that cause pain in the arms. Therefore, the most reasonable thing is to immediately contact a specialist, and not try to figure it out on your own.
Diagnosis of pain in the arm may take 2-3 days. First of all, this is an examination by a neurologist, as well as conventional clinical methods (tests, X-rays, MRI) and special techniques that allow you to accurately determine the extent of nerve damage - electromyography and electroneurography.
These methods examine the electrical activity of muscles and the speed of transmission of nerve impulses. By combining the results of both methods, one can understand whether the nerve has retained its function or has degenerated and been replaced by connective tissue. The treatment method depends on the results of the examination.
What can a doctor do?
There is no specific treatment for Steinbrocker syndrome. It is based on novocaine blockades of the anterior scalene muscle and stellate ganglion. Sometimes ganglion blockers are added to Novocaine - gangleron, pentamin, benzohexonium.
At the initial stage, phonophoresis with hydrocortisone, which must be alternated with electrophoresis with nicotinic acid, helps to relieve symptoms. Finlepsin is prescribed, or intramuscular administration of B vitamins. Proserin is prescribed according to a specific and long-developed scheme. Sometimes additional antihistamines and decongestants are required. Some patients benefit from acupuncture.
Treatment
A radical way to treat tunnel syndrome is surgery, when the diameter of the canal is artificially increased. If the time for surgery is missed, or it is undesirable for other reasons, various conservative methods are used - medication, elastic fixators and orthoses, changing the locomotor stereotype or retraining for correct movements. The treatment that will give the best result for a particular person is used.
Neurologists and orthopedic surgeons at our clinic have extensive practical experience; they will be able to relieve you within a few days of pain that has tormented you for years. Diagnostic equipment allows you to find out the smallest details that have been bothering you for a long time. Treatment in our clinic eliminates carpal tunnel syndrome forever.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Main types
There are primary (at the level of the outlet of the supraspinatus muscle) and secondary (at another level) impingement syndrome.
Primary impingement syndrome
Occurs when mechanical irritation of the supraspinatus muscle in a narrow space is associated with:
- congenital deformation of the acromion process;
- thickening of the muscle at the anterior edge of the acromion;
- the presence of osteophyte of the acromioclavicular joint;
- changes in bone shape after injury;
- acromio-clavicular arthrosis.
Secondary impingement.
It appears with a relative decrease in the subacromial space due to:
- chronic bursitis;
- an increase in the size of the rotator cuff due to spasm or inflammation;
- displacement of the greater tubercle of the humerus due to injury;
- ossification of the rotator cuff;
- so-called instability of the shoulder joint.
There are also three stages of damage to the rotator cuff muscles in subacromial syndrome, which determine the treatment tactics for their infringement:
- The first stage is characterized by swelling and hemorrhages in the tendons. At the same time, there is no violation of their integrity. It occurs in young athletes and responds well to treatment if treated in a timely manner.
- The second, in addition to tendon thickening, is characterized by signs of chronic inflammation, fibrosis, the presence of microtraumas, and tears. Depending on the reason, the issue of surgery is decided.
- The third demonstrates complete tendon ruptures, degenerative bone lesions - the acromion and the greater tubercle of the humerus; presence of osteophytes. Occurs in patients over 40 years of age. In this situation, surgical intervention is necessary.
Kinds
There are only two types of impingement syndrome: primary and secondary.
- Primary impingement syndrome is irritation of the shoulder muscles due to injuries, osteophytes, and congenital deformities.
- Secondary impingement syndrome - develops when the acromial space is narrowed after ligament rupture or other injury, with chronic bursitis.
With this disease, it is important not to miss the first symptoms of damage to the shoulder tissue. The earlier treatment is started, the better the prognosis. A severe form of the disease leads to loss of function of the affected shoulder. At the first stage, tissue swelling and internal hemorrhages occur, which are treated with conservative methods. Inflammation provokes the development of tendinitis and fibrous tissue - this second stage does not go away without surgical intervention. If left untreated, a severe form develops with a rupture of the rotator cuff or tendon, and a bone spur grows, making movement of the arm almost impossible. Therapy is long and not always successful.