Types of osteomas
Diagnosis of osteoma involves differentiation from similar neoplasms and determination of its type in order to select subsequent treatment.
Tumors are divided by number, type of tissue they are made of, method of germination and complexity of structure. Each of them can be located in different parts of the musculoskeletal system and provoke different symptoms. Based on the number of tumors, they are divided into single (solitary) and multiple, and based on their composition into solid, spongy and medullary. The first consist entirely of bone tissue without bone marrow, the second of spongy substance, and the third of bone marrow cavities. Tumors originate from different tissues (bone or connective) and because of this they have different names:
- hyperplastic – consist exclusively of bone (osteomas and osteoid osteomas),
- heteroplastic - osteophytes, composed of different tissues.
Osteomas are composed of normal bone tissue, are localized on the bones of the skull, and often put pressure on neighboring organs, such as the eyes. Osteoid osteomas consist of osteogenic tissue penetrated by blood vessels, bone membranes, areas of destroyed bone tissue, and are localized anywhere, in 50% of cases - on the tibia. At the initial stage of development of the disease, there are no symptoms, and then a flat, thin infiltrate appears (if we talk about epiphyseal osteoma, it accumulates in the joint). If in children this type of tumor occurs in the bone growth zone, then one limb will increase in length.
Osteophytes are also divided into 2 types - ectostoses, which grow from above (the skull, face, pelvic bones are the favorite places for their localization), and enostoses, internal, growing into the medullary canal. Exostoses have the shape of a hemisphere, cauliflower, thorn, or mushroom. One of the features of osteophytes (heteroplastic osteomas) is that they appear on the diaphragm, lining of the heart, brain tissue, etc.
Classification
1. Primary tumors of the spine: Vascular - hemangioma, hemangioendothelioma, hemangiosarcoma. Cartilaginous - osteochondroma, chondroma, chondrosarcoma. Bone-forming – osteoid osteoma, osteoblastoma, osteosarcoma. Giant cell tumor – osteoclastoma. Mixed bone tumors - Ewing's sarcoma. Bone marrow – multiple myeloma, lymphoma. Tumor-like processes – aneurysmal bone cyst, eosinophilic granuloma. 2. Secondary tumors of the spine.
Causes
The cause of osteoma is said to be heredity, but its appearance and progression can also be facilitated by certain diseases, including gout, syphilis and rheumatism (the trigger is often trauma, especially repeated trauma). The pathology of calcium metabolism sometimes causes the development of inert tumors, the pathological development of embryonic cells can lead to the development of growths, and when localized in the nasal sinuses - a purulent complication or inflammation, puncture of the maxillary sinus. Ectostoses can form during puberty.
Clinical manifestations
Typical symptoms:
- Diffuse pain syndrome, without precise localization
- Salicylates are highly effective in relieving pain
- Damage to the spine is combined with its curvature (scoliosis, kyphoscoliosis, lordosis, torticollis) and is accompanied by pain
- In the presence of a pathological curvature of the spine, the concave part of the curvature faces the lesion
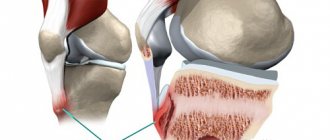
- Symptoms of intra-articular osteoid osteoma are similar to arthritis and osteoarthritis.
Symptoms
The signs of osteomas depend on the location, are not similar to each other, and are sometimes difficult to differentiate due to symptoms similar to other common diseases. It is easier to make a diagnosis in the presence of convex external tumors that are visible to the naked eye.
If the tumor is located on the bones of the head, depending on the location, symptoms are observed:
- on the posterior wall of the frontal sinus - intracranial pressure, headaches (do not go away), size from 2 to 30 mm;
- on the lower wall of the frontal sinus - moving the eye forward;
- on the frontal bone (internal plates) - memory problems, headaches, seizures with convulsions, intracranial pressure;
- in the nasal cavity - difficulty breathing through the nose, decreased sense of smell, problems with the eyes (drooping eyelid, double vision, decreased vision);
- on the occipital bone - pain in the head, sometimes epileptic seizures;
- on the parietal and temporal bone - noticeable, but does not cause painful symptoms;
- on the lower jaw (lateral branch or posterior side) - when compressing the soft tissues of the muscles, they can lead to asymmetry and dysfunction, the edges of the tumor are smooth, and the shape is oval or round.
In addition to the bones of the skull, the tumor also affects the bones of other parts of the musculoskeletal system, respectively, symptoms of osteoma and pain appear at its location:
- thigh bones - muscle pain, worse at night, swelling in the legs, altered gait;
- knee joint - makes movement difficult;
- vertebral arch or its process – the formation of scoliosis, symptoms of spinal compression, pain.
Pain due to osteophytes is eliminated completely or partially with the help of analgesics, however, if there are regular repeated attacks of pain, difficulty moving, or the appearance of visible lumps, you should immediately consult a doctor to avoid complications.
Description example:
In the arch of the C7 vertebra, a focus of tissue intensity (iso-hypointense by T1, slightly hyperintense by STIR) of irregular oval shape, size ... cm, with unclear contours, perifocal edema of the adjacent bone tissue and paravertebral soft tissues, without signs of destruction of the cortex, inhomogeneous contrast enhancement is determined.
CONCLUSION: MR picture of a focal space-occupying lesion of the C7 vertebral arch (differential diagnosis of osteomyelitis and space-occupying lesion), MSCT is recommended.
Diagnostics
Diagnosis of the tumor is carried out to determine its type and location in order to select tactics for treating osteoma. As part of its implementation, X-ray and CT are used. The most informative is a 3D reconstruction; it shows all the details and outlines, as well as the extent of damage to surrounding tissues. In the process, it is important to differentiate osteoma from chronic Brody’s abscess, organized periosteal callus, osteochondrosis dissecans, osteogenic sarcoma, osteoperiostitis and other diseases.
Before prescribing an x-ray or tomography, the doctor conducts an examination and identifies:
- presence of pain when pressing;
- location;
- growth rate;
- functionality of the tissue that has been affected.
Using X-rays, a specialist detects the number of tumors, their structure, location, and the degree of bone destruction. It should be noted that on an x-ray the exostosis looks smaller than in reality, since its upper cartilaginous layer is not visible. In children it reaches a thickness of several centimeters. The benign nature of the tumor is indicated by correct geometry and structure, a clear contour, a small degree of calcification and growth at a low rate.
List of used literature and sources
1. Kornienko, V.N. – Diagnostic neuroradiology. Volume 4 – V. N. Kornienko, I. N. Pronin / Moscow, 2012 – 487 pp. 2. General guidelines for radiology. Editor Holger Petterssob, MD. Russian edition: RA “Spas”, 1996. 3. Trufanov G. E. Radiation diagnosis of tumors and tumor-like diseases of the spine and spinal cord / G. E. Trufanov, T. E. Rameshvili, N. I. Dergunova. – St. Petersburg: ELBI-SPb, 2011 – 384 p. 4. Trufanov, G. E. Magnetic resonance imaging (a guide for doctors) / Ed. prof. G. E Trufanov and Ph.D. V. A. Fokina. – St. Petersburg: FOLIANT Publishing House LLC, 2007. – 688 p.
Treatment
Removal of osteoma is indicated if it compresses neighboring organs, is visible visually, that is, acts as a cosmetic defect (especially on the face and head), changes the shape of bones, reduces mobility, leads to scoliosis, and causes pain. Most often, tumors are removed from the sinuses, ear canal, jaws, knee and hip joints.
If the tumor does not manifest itself in any way and does not cause discomfort, the doctor observes it and evaluates its growth rate. A small osteoma that has stopped growing does not need to be removed or treated.
The operation to remove the tumor is performed by maxillofacial surgeons or neurosurgeons. During the operation, the doctor cuts the tissue, removes the growth and part of the bone/tissue around it to avoid relapse.
The doctor will suggest removing the osteoma in the following ways:
- complete excision – used for tumors in the sphenoid sinus;
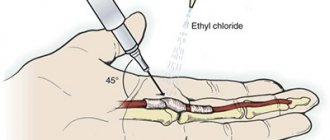
- curettage - an incision in the skin, removal of a tumor, cleansing the lesion by curettage;
- endoscopic removal - suitable for small tumors with a difficult approach, used using computed tomography to monitor the progress of the operation and a radiofrequency probe, takes about 2 hours.
Tumor recurrence occurs in 10% of cases due to incomplete removal. To exclude this possibility, you need to choose a good clinic and specialist.
What is osteoid osteoma and why does it develop?
- The name uses the term osteoid, or in other words, bone tissue before minerals are laid into it, which means that this tumor can develop in any part of the bone - in the cortical layer, in the spongy substance or under the periosteum.
- Osteoid osteoma is a benign osteogenic (bone-forming) tumor.
- 4-11% of all benign bone tumors
- Usually diagnosed during adolescence
- Affects men twice as often as women
- Osteoids are predominantly formed diaphyseal/metaphyseal in long tubular bones (65%), phalanges (20%) or spine (10%)
- Lesions may occur in the hip joint
- Multicentric or multifocal osteoid osteoma occurs extremely rarely.
Causes:
- Small (less than 1 cm), painful tumor composed of osteoblasts
- High degree of ossification
- In the central part there is a highly vascularized core (in the presence of calcification - “mature” osteoid osteoma)
- Reactive formation of new bone tissue around the lesion
- Core histology: highly vascularized loose connective tissue with bands of proliferative trabecular bone tissue of irregular shape, active osteoblasts without signs of atypia
Classification by location:
— Cortical (80%).
- Intra-articular or periarticular (mainly the neck of the femur, bones of the hands and feet, spine).
— Subperiosteal (mainly the intertrochanteric region of the femur, bones of the hands, feet, especially the neck of the talus).
Is osteoma dangerous?
Speaking about the dangers of osteoma, one should note first of all the compression of neighboring organs and symptoms that cause inconvenience to the patient. If the tumor does not manifest itself and does not grow, it can be left in place. A neoplasm of this kind never develops into malignant – there is no need to be afraid of cancer. Tumors on the head should be treated with particular care - they not only cause unpleasant symptoms, but can also lead to a brain abscess. As a rule, they are removed surgically.
Which method of diagnosing osteoid osteoma to choose: MRI, CT, X-ray, ultrasound
Selection Methods
- X-ray examination
- Radionuclide research
- CT
- MRI.
What will X-rays of limb bones show with osteoma?
- A focus of osteolysis in the cortical bone the size of a grain of rice, surrounded by a zone of sclerosis
- Often the cortical layer is significantly thickened
- With intra-articular osteoid osteoma, sclerosis may be absent
- Effusion is detected in the joint cavity
- In case of damage to the vertebrae, pathological smoothing is observed.
a, b Osteoid-osteoma in the concave part of the femoral neck, with its base on the cortical layer. The patient has typical clinical symptoms with pain at night, and a good response to aspirin: a ) X-ray examination. A focus of osteolysis with a diameter of 8 mm with erosion of the cortical layer (arrow); b ) CT scan, coronal reconstruction. Small calcifications in the lesion area.
In what cases is a CT scan of the limb performed for osteoid osteoma of the bone?
- CT makes it possible to more clearly identify a focus of varying degrees of mineralization (absent, dotted, ring-shaped or, rarely, homogeneous)
- After administration of a contrast agent, the nucleus quickly and intensively accumulates the contrast agent
- Sclerotic changes in surrounding tissues.
What will MRI images of bones show in osteoma?
- On T1-weighted image, the nucleus is isointense to the muscles, slightly hyperintense on T2-weighted image.
- The accumulation of contrast material after contrast agent administration is particularly well determined on T1-weighted sequences with suppression of the MR signal from adipose tissue
- Fat-suppressed T2-weighted or short T1 inversion recovery (STIR) sequences show widespread bone marrow edema
- This may be a sign of osteoid osteoma if combined with characteristic clinical symptoms (young age, spontaneous pain, mainly at night, absence of trauma)
- Intra-articular osteoid osteoma often occurs in combination with synovitis and effusion in the joint cavity.
a, b Osteoid-osteoma of a club-shaped bone. History: persistent pain; long-term complaints without establishing an accurate diagnosis: a) MRI, STIR . Severe swelling extends to almost the entire bone. b ) Hypointense lesion on T1-weighted sequence.
Why is scintigraphy performed if osteoid osteoma is suspected?
- A characteristic feature of “double density”: a highly active central area is surrounded by a less active zone with a lower level of radionuclide accumulation.
Effective treatment of osteoid osteoma of the spine in Israel, at the Top Ichilov clinic
Treatment of osteoid osteoma of the spine is only surgical.
Considering that all spinal surgeries are high-risk surgical interventions, it is better to undergo treatment in highly specialized clinics. The Top Ichilov Medical Center employs high-level professionals who have a wide range of operations on the spinal column. In addition, the clinic’s neurosurgeons are actively engaged in scientific activities and developing new methods of surgical interventions. All spine surgeries in Top Ikhilov are performed using the latest endoscopic and laser equipment. This method of minimally invasive intervention allows you to completely remove the tumor and return the patient to a full life in the shortest possible time. The Top Ichilov Clinic uses the following modern methods of treating spinal osteoid osteoma:
- Endoscopic, low-traumatic, incision-free surgical techniques
- Advanced radiosurgery
- Subsequent spinal stabilization
Treatment of spinal cord tumors and spinal tumors can be combined and include surgical methods, radiotherapy, chemotherapy, and hormonal therapy.