Currently, such a pathology as osteochondropathy of the tibial tuberosity is quite common. Young people suffer from this disease. The disease is often diagnosed in individuals involved in a certain type of activity (football players, basketball players, track and field athletes and other athletes).
The second name for this pathology is Schlatter's disease. The disease is dangerous because it has a chronic, progressive course and, in the absence of proper therapy, can cause a person to lose their ability to work. What are the etiology, clinical picture and treatment of Schlatter's disease?
Causes of the disease
Schlatter's disease is a non-inflammatory disease accompanied by necrosis of bone tissue.
This pathology most often develops on one leg, although there are cases of it occurring on both. It is usually observed in children and adolescents aged ten to eighteen years, when bones are at their most intense stage of growth. It can be found much more often in boys. The disease often develops for no apparent reason (in some cases it is possible to trace a connection with bruises and injuries).
The causes of the development of the disease are often the following factors:
- direct injuries: fractures and dislocations of the patella or tibia, damage to the knee joint;
- permanent microtraumas of the knee associated with sports.
Get prices from the Israeli Ministry of Health
Enter your data and get the price list on Viber, WhatsApp or Telegram
According to medical statistics, Osgood Schlatter disease affects about 20% of teenagers actively involved in sports and only 5% of those who are not involved in sports.
The risk group includes children who engage in the following sports:
- basketball;
- volleyball;
- hockey;
- football;
- gymnastics;
- acrobatics;
- figure skating;
- ballet;
- struggle;
- weightlifting.
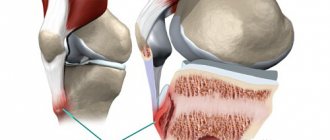
As a result of overloads, constant microtraumas of the knees, as well as excessive tension of the patellar ligaments that occur during contractions of the quadriceps femoris muscle, there is a disturbance in the blood supply in the area of the tibia, or more precisely, in the area of its tuberosity. It is accompanied by minor hemorrhages, rupture of the fibers of the patellar ligaments, an aseptic inflammatory process in the bags, as well as changes in the necrotic nature of the tibial tuberosity.
Features of Schlatter's disease
Osteochondropathy of the tibial tuberosity is a disease of non-inflammatory origin, characterized by destruction (necrosis) of the bone tuberosity. The tibia forms the skeleton of the lower limbs. It is located in the lower leg area (between the knee and foot). This is one of the largest bones in the human body. Next to it is the fibula. The tuberosity is located at the top of the anterior edge of the bone. The quadriceps femoris muscle is attached to it. This disease has been known for about a century and is part of a special group of diseases called osteochondropathy.
Schlatter's disease is most often diagnosed in people aged 10 to 18 years. Boys suffer from this disease much more often than girls.
This is due to a more active lifestyle of people, an addiction to sports games, which often leads to bone trauma.
The process most often affects both bones. Unilateral lesions are less common. Often there is a combined lesion of the tibia and spine. The disease occurs in a chronic form. At the same time, the percentage of benign course of the disease is high.
Etiological factors
Osteochondropathy of the tibial tuberosity most often develops against the background of trauma. The latter may be due to:
- playing sports (football, volleyball, hockey, basketball);
- choreography classes;
- regular blows to the shin area.
The risk group includes children and adolescents who actively engage in sports. About 20% of all teenage athletes suffer from this pathology. Schlatter's disease can also occur in children who do not lead a similar lifestyle. The cause in this case may be domestic injuries.
In recent years, girls have increasingly become interested in gymnastics, figure skating, choreography, and fitness. Therefore, they are also at risk.
Permanent injuries lead to disruption of the nutrition of the tuberosity of the tibia. This is facilitated by contraction of the quadriceps muscle. All tubular bones have so-called growth zones. Children experience active growth of bones that are not yet fully developed. Regular injuries can cause avulsion fractures. These fractures soon heal, and a bone growth forms in this place. Over time, this causes characteristic symptoms in children and adolescents.
Clinical manifestations
Schlatter's disease has rather sparse symptoms. In the early stages, patients may not present any complaints. The most common symptom is pain. It has the following features:
- localized in the area of the tibia closer to the knee;
- weak at first, but gradually intensifies;
- becomes more intense with active movements;
- worsens when kneeling;
- subsides at rest;
- often combined with swelling in the knee area.
Objective signs of the disease include severe tissue swelling at the site of the lesion and bone tenderness on palpation. The disease is non-infectious, so general symptoms such as increased body temperature are not observed. Unlike a fracture or bruise, there is no pronounced hyperemia at the site of bone damage. In some patients, the disease progresses in waves. In this case, an exacerbation in the form of pain can be provoked by intense physical activity (jumping, running, squats).
Symptoms and course of the disease
Schlatter's disease is characterized by a gradual, asymptomatic onset. Patients, as a rule, do not associate the occurrence of the disease with a knee injury.
The main symptoms of Osgood-Schlatter disease include:
- swelling and tenderness in the area of the tibial tuberosity, just below the kneecap;
- pain in the knees, which intensifies after physical activity, especially when running, jumping and climbing stairs - and decreases with rest;
- Tightness of the surrounding muscles, especially the thigh muscles (quadriceps).
Pain varies depending on each individual. Some may only have mild pain when doing certain activities, especially running or jumping. For others, the pain can be constant and debilitating. Typically, Osgood-Schlatter disease occurs in only one knee, but sometimes it can occur in both knees. The discomfort may last from several weeks to several months and may recur until the child stops growing.
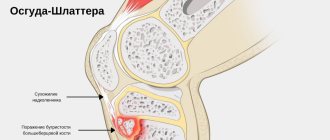
When examining the knee, swelling is noted, smoothing the contours of the tibial tuberosity. Palpation in the area of the tuberosity reveals local soreness and swelling, which has a densely elastic consistency. A hard protrusion is palpated through the swelling.
Schlatter's disease has a chronic course, sometimes there is a wavy course with pronounced periods of exacerbation. The disease lasts from 1 to 2 years and often leads to recovery of the patient after the end of bone growth (at approximately the age of 17-19 years).
Complications of Osgood-Schlatter disease are rare. These may include chronic pain or localized swelling that responds well to cold compresses and anti-inflammatory medications. Often, even after the symptoms have disappeared, a bone lump may remain on the lower leg in the area of the swelling. This lump may persist to varying degrees throughout the child's life, but it does not usually impair the function of the knee.
In the advanced state of the disease, muscle wasting may develop in the affected limb, which will lead and will manifest itself through minor restrictions in the movements of the knee joint.
Although many doctors claim that Schlatter’s disease can go away on its own after a certain period of time, practice shows exactly the opposite (with rare exceptions). Therefore, if a child complains of constant pain in the knee joint or has a slight swelling of the knee, it is necessary to immediately consult a doctor.
Osteochondropathy of the tibial tuberosity[edit | edit code]
This disease (Osgood-Schlatter disease)
first described by Osgood (USA) and Schlatter (Switzerland) in 1903. In the scientific literature, the disease is known as aseptic necrosis of the tibial tuberosity, tibial apophysitis, Laub disease, Lanelong-Osgood-Schlatter disease.
It occurs quite often, affecting mainly boys aged 13-15 years, of strong build, involved in sports, often on both sides (on both legs). The basis of the disease is a violation of the ossification processes of the tibial tuberosity. Osteochondropathy often develops for no apparent reason. However, sometimes a connection can be made with re-injury or increased function of the quadriceps muscle (for example, during sports or ballet). In some adolescents, changes in the tibial tuberosity are combined with those in the spine, characteristic of osteochondropathy.
Clinical picture[edit | edit code]
Above the tuberosity of the tibia, swelling, swelling, thickening and bulging of the cartilage, pain on palpation, as well as support on the knee joint, occur at the time of bending and moving the limb forward. Movements in the knee joint are especially painful after physical activity.
X-ray examination[edit | edit code]
When radiographically diagnosing Osgood-Schlatter disease, it is necessary to keep in mind the many variants of normal ossification of the tibial apophysis. Most often, it ossifies in the form of a trunk-shaped process at the age of 10-13 years, but there are variants with additional small ossification nuclei. The fusion of the apophysis with the metaphysis occurs at the age of 16-18 years.
In osteochondropathy, irregular, unclear contours of the tuberosity and its fragmentation into several sequester-like fragments are determined.
When diagnosing, one should always take into account the discrepancy between the significant bulging of the tuberosity on clinical examination and the almost normal size of the apophysis on radiographs. Preference should be given to clinical data.
The process proceeds favorably and ends with the restoration of the structure of the apophysis. The function of the knee joint is not affected. The disease should be differentiated from infrapatellar bursitis, osteomyelitis, and cartilaginous tumor.
Treatment[edit | edit code]
First of all, it is necessary to eliminate any overloads and create relative rest, up to short-term immobilization. Treatment is based on physiotherapeutic methods (magnetic therapy, electrophoresis with calcium and novocaine, balneotherapy and mud therapy). Surgical treatment, as a rule, is not used, with the exception of isolated cases of tuberosity separation during increased physical activity. Painful osteochondral bodies that have become detached as a result of the disease can also be removed surgically.
Athletes at particular risk are young people, aged 13-18 years, of both sexes, especially those involved in cross-country sports.
The question of the possibility of admission to sports is decided individually. Jumping exercises and running are absolutely contraindicated. When using them, the tuberosity may be torn off along with the ligament.
Osteochondropathy of the tibial tuberosity goes away on its own. Ice application and stretching of the quadriceps, hamstrings, and calf muscles are indicated to relieve symptoms. NSAIDs are prescribed for pain relief, and sometimes it is necessary to change the training program. In some cases, to eliminate inflammation and pain, a plaster cast is applied for 2-3 weeks. In addition to the described plan, it is advisable to strengthen the hamstrings and quadriceps muscles. If it is necessary to frequently rest your knee on a hard surface (for example, in volleyball), the tibial tuberosity is protected with a knee pad.
Forecast[edit | edit code]
Osteochondropathy of the tibial tuberosity is not associated with a significant risk of deforming osteoarthritis. There are reports of tuberosity fractures associated with osteochondropathy, but no statistically significant relationship has been identified between them. In this regard, restriction of physical activity due to osteochondropathy is inappropriate.
Very rarely, fragments of the tuberosity do not grow together, and one of them, in contact with the patellar ligament, constantly irritates it. In such cases, excision of the fragment may be recommended.
Return to sports[edit | edit code]
The only thing that limits physical activity is pain. Osteochondropathy of the tibial tuberosity resolves spontaneously, and sports activities aggravate the patient’s condition.
Treatment of the disease
Osgood-Schlatter disease usually resolves on its own, and symptoms disappear after bone growth has completed. If the symptoms are severe, then treatment is prescribed.
Conservative treatment
Patients with Schlatter's disease usually undergo outpatient conservative treatment with a surgeon, traumatologist or orthopedist. First of all, it is necessary to eliminate physical activity and ensure the maximum possible rest of the affected knee joint. In severe cases, it is possible to apply a fixing bandage to the joint.
The basis of drug treatment for Schlatter's disease is anti-inflammatory and painkillers.
Physiotherapeutic methods are also widely used: mud therapy, magnetic therapy, UHF, shock wave therapy, paraffin therapy, massage of the lower limb. To restore damaged areas of the tibia, calcium electrophoresis is performed.
Physical therapy classes include a set of exercises aimed at stretching the hamstrings and quadriceps femoris muscles. Their result is a decrease in the tension of the patellar ligament, which attaches to the tibia. To stabilize the knee joint, the treatment complex also includes exercises that strengthen the thigh muscles.
After a course of treatment for Schlatter's disease, it is necessary to limit the load on the knee joint. The patient should avoid jumping, running, kneeling, and squatting. It is better to change traumatic sports to more gentle ones, for example, swimming in a pool.
Surgery
With severe destruction of bone tissue in the area of the head of the tibia, surgical treatment of Schlatter's disease is possible. The operation consists of removing bone growths, necrotic foci and suturing a bone graft that fixes the tibial tuberosity, which allows healing of the avulsion fracture and complete restoration of the function of the knee joint.
After surgery, a course of physical therapy and medication is required. You can play sports only six months after the operation.
Medical Scientific and Practical Center for Vertebrology and Neuroorthopedics, Professor M.L. Kurganov
Osteochondropathies are a group of diseases that occur in childhood and adolescence due to malnutrition of bone tissue . In the area of the bone, the blood supply is disrupted and areas of necrosis appear. The disease most often occurs in the epiphyses and apophyses of the tubular bones of the arms, legs and vertebrae. The epiphysis is the site of bone tissue growth. Apophysis is a protrusion of bones near the growth plate to which muscles and ligaments are attached. Usually this is the terminal part of a long tubular bone. The disease is chronic and often develops in the lower extremities , which are under greater load. Most osteochondropathy has a hereditary basis.
Legg-Calvé-Perthes disease.
Legg-Calvé-Perthes disease or chondropathy of the femoral head is also called juvenile osteochondrosis of the femoral head. Boys aged 4 to 12 years are more likely to get sick. Usually, injury to the hip joint area occurs first, then the blood supply to the femoral head is disrupted.
First, necrosis of areas of the bone tissue of the femoral head occurs. This can be seen on an x-ray. In the second stage of the disease, the head of the femur is flattened under the influence of heavy load. The next stage is called the fragmentation stage. In this case, resorption of areas of necrotic bone tissue occurs. In the absence of treatment, the fourth stage occurs - osteosclerosis. The femoral head is restored, but its normal shape is changed. The final stage, with insufficient treatment, is deforming arthrosis of the hip joint with disruption of its function.
At the beginning of the disease, there are practically no complaints. Then pain appears in the hip joint, which radiates to the knee. Pain often occurs after exercise and disappears after rest and at night. The child may not pay attention to the pain and not complain. Gradually, restriction of movements in the hip joint occurs. During this period, you may notice weight loss in the thigh on the affected side, caused by muscle atrophy. X-rays are taken to make a diagnosis. Radiologically, five stages of the disease are distinguished, corresponding to changes in the femoral head.
Treatment can be surgical or conservative. Conservative treatment includes mandatory bed rest. The patient is forbidden to even sit in order to eliminate the load on the head of the femur. Skeletal traction is applied to both hips. Daily massage of the lower extremities and physiotherapeutic treatment are prescribed. Surgical treatment consists of performing various osteoplastic operations. The types of surgical interventions depend on the stage of the disease.
Keller's disease. This is chondropathy of the bones of the foot. There are Keller disease I and Keller disease II.
Keller disease I is a chondropathy of the navicular bone of the foot. The disease develops in childhood from 4 to 12 years. The patient experiences pain and swelling of the upper (dorsal) surface of the foot above the navicular bone. The pain intensifies while walking. The child is limping. To clarify the diagnosis, x-rays of the foot bones are taken. A change in the shape of the scaphoid bone and its fragmentation are detected.
Treatment consists of unloading the foot. A plaster cast is applied for 4-6 weeks. After the cast is removed, physical therapy and physiotherapeutic procedures are prescribed, which are combined with reducing the load on the foot. For 1-2 years, the child must wear orthopedic shoes.
Keller disease II is a chondropathy of the metatarsal heads. The second metatarsal bone is most often affected by the disease. The patient experiences pain in the affected area. The pain increases sharply when walking, especially barefoot on uneven surfaces and wearing shoes with soft soles. Shortening of the fingers may occur. When palpated, a sharp pain in the bases of the fingers is detected. The heads of the metatarsal bones increase in size. The diagnosis and stage of the disease are clarified using x-rays.
Treatment of Keller II disease is conservative. The foot is unloaded. To do this, a plaster boot is applied for one month. Then the child must wear orthopedic shoes, since there is a high risk of developing flat feet. Massage, physiotherapeutic procedures, and therapeutic exercises are used. The disease lasts 2-3 years. In the absence of a good effect from conservative therapy and the development of severe deforming arthrosis of the joint, surgical treatment is prescribed.
Kienbeck's disease.
This is chondropathy of the lunate bone of the hand. It manifests itself by the development of aseptic necrosis in this bone. The disease develops in men 25-40 years old after major injuries or prolonged microtraumatization of the hand, when working with heavy physical load on the hands. The patient experiences discomfort in the hand and constant pain, which intensifies with exercise and movement. Swelling occurs at the base of the hand. Limitation of mobility in the wrist joint gradually develops. Limitation of joint mobility in turn causes a decrease in the work of the forearm muscles and their atrophy. The diagnosis is confirmed using x-ray examination.
Treatment of Kienböck's disease. The load on the bone is limited. To do this, a plaster cast is applied for 2-3 months. After removing the cast, massage, physiotherapeutic procedures, and physical therapy are prescribed. When severe deforming arthrosis develops, surgical treatment is used.
Schlatter's disease or Ostgood-Schlatter disease.
Schlatter's disease occurs in boys from 12 to 16 years old, especially in those who play sports, dance sports, and ballet. Under increased load, chondropathy of the tibial tuberosity develops. The tibial tuberosity is located on its anterior surface, below the patella. The quadriceps femoris muscle is attached to the tibial tuberosity.
In young men, the process of ossification of the tibial tuberosity is not yet completed, and it is separated from the tibia proper by a cartilaginous zone. With constant load on the tuberosity, the blood supply is disrupted, and areas of the tuberosity undergo necrosis and then restoration. By the age of 18, the tuberosity fuses with the tibia and recovery begins. The patient complains of pain below the patella and swelling. The pain intensifies when the quadriceps muscle is tense, when climbing stairs, or squatting.
The diagnosis is confirmed by x-ray. Treatment consists of eliminating the load on the quadriceps femoris muscle. Warmth and physiotherapeutic procedures are prescribed. If the pain is severe, a plaster cast is applied. Occasionally, it is necessary to use surgical methods, which involve surgical removal of a fragment of the tibial tuberosity.
Osteochondropathies of the vertebral bodies
Calvet's disease.
Calvet disease is chondropathy of the vertebral body. Most often, the disease affects the lower thoracic or upper lumbar vertebrae. Boys from 7 to 14 years old are affected. The patient experiences pain in the area of the affected vertebra or in the thoracic and lumbar spine. Upon examination, you can detect a protruding spinous process of the diseased vertebra. When palpating the spinous process, the pain intensifies. An x-ray reveals a sharp decrease in the height of this vertebra and its expansion.
Treatment of Calve's disease is conservative. Bed rest is prescribed in a special position on the bed to reduce the load on the vertebra. Physical therapy is used, which consists of a set of exercises to strengthen the back muscles to create a muscle corset. After this, the patient must wear a special corset for several years. Surgical treatment is prescribed in the absence of effect from conservative therapy and progressive spinal deformity.
Kümmel's disease.
Kümmel's disease or Kümmel-Verneuil disease is a traumatic aseptic (non-microbial) inflammation of the vertebral body (spondylitis). The cause of this disease is vertebral trauma, which leads to the development of areas of necrosis in the vertebral body. The patient experiences pain in the area of the injured vertebra, which goes away after 10-14 days. After this, a period of false prosperity begins, sometimes lasting up to several years. Then pain appears again in the area of the injured vertebra. The patient may not remember the previous injury. The pain appears first in the spine, then radiates to the intercostal spaces. An X-ray examination reveals a wedge-shaped vertebra.
Treatment consists of unloading the spine. For this purpose, bed rest is prescribed for 1 month. The bed should be hard. A cushion is placed under the thoracic region. Then physiotherapeutic treatment and exercise therapy are prescribed.
Scheuermann-Mau disease.
Scheuermann-Mau disease, Schmorl's disease, chondropathic kyphosis, juvenile kyphosis, apophysitis of the vertebral bodies (inflammation of the places where muscles attach to the vertebra) or chondropathy of the apophyses of the thoracic vertebrae are different names for the same disease. With this disease, the 7-10 thoracic vertebrae are most often affected. The disease occurs in boys from 11 to 18 years old. The patient complains of back pain and fatigue of the back muscles with normal activity. On examination, increased thoracic kyphosis is detected (curvature of the spine in the thoracic region with a convexity posteriorly). X-rays reveal changes in the shape of the vertebrae. Normal vertebrae in the thoracic region look like bricks, with smooth edges. With Scheuermann-Mau disease, the vertebrae in the lower thoracic region become wedge-shaped.
Treatment consists of physical therapy, massage, underwater traction, and swimming. Occasionally, in cases of severe postural disorders, surgical treatment is used.
Diagnosis of the disease
Diagnosis of Osgood-Schlatter disease is carried out by a specialist doctor (orthopedist). For diagnosis, the history of the disease is of great importance and the doctor needs the following information:
- Detailed description of the child's symptoms.
- Relationship between symptoms and physical activity.
- Information about past medical problems (especially previous injuries).
- Information about medical problems in the family.
- All medications and nutritional supplements that the child takes.
To diagnose Osgood-Schlatter disease, the doctor will examine the child's knee joint, which will determine the presence of swelling, tenderness, and redness. In addition, range of motion in the knee and hip will be assessed.
To make an accurate diagnosis, it is necessary to conduct an X-ray examination of the joints of the affected limb, which most often reveals a slight increase in the area of the tibia tuberosity and separation of the apophysis (bone process) from it.
X-ray examination also allows you to determine the stage of development of this disease.
To obtain more complete information, the doctor may prescribe diagnostic methods such as computer thermography, magnetic resonance imaging and ultrasonography. Densitometry is also used to obtain data on the structure of bone tissue. Laboratory diagnostics are prescribed to exclude the infectious nature of damage to the knee joint (specific and nonspecific arthritis). It includes a clinical blood test, a blood test for C-reactive protein and rheumatoid factor, and PCR studies.
In the initial period, Schlatter's disease is characterized by a radiographic picture of flattening of the soft cover of the tibial tuberosity and raising of the lower border of the clearing, corresponding to the adipose tissue located in the anterior part of the knee joint. The latter is due to an increase in the volume of the subpatellar bursa as a result of its aseptic inflammation. There are no changes in the nuclei (or nucleus) of ossification of the tibial tuberosity at the onset of Schlatter's disease.
Over time, radiologically, a displacement of the ossification nuclei forward and upward by 2 to 5 mm is noted. The trabecular structure of the nuclei may be blurred and their contours uneven. Gradual resorption of displaced nuclei is possible. But more often they merge with the main part of the ossification nucleus to form a bone conglomerate, the base of which is the tibial tuberosity, and the apex is a spine-like protrusion, clearly visualized on a lateral radiograph and palpated in the area of the tuberosity.
Differential diagnosis of Schlatter's disease must be carried out with a fracture of the tibia, syphilis, tuberculosis, osteomyelitis, and tumor processes.
Diagnostic measures
Osteochondropathy of the tibial tuberosity can be identified on the basis of an external examination, characteristic clinical data and an x-ray picture. Patient information is of no small importance in making a diagnosis. The age and gender of the patient are taken into account. Diagnostics includes:
- collection of anamnesis of illness and life;
- examination of the lower extremities;
- palpation;
- X-ray examination;
- Ultrasound;
- general and biochemical blood tests.
Currently, computed tomography and magnetic resonance imaging are increasingly used to detect pathology of the skeletal system. It is advisable to carry out instrumental research several times to determine whether the disease is progressing or not. In the early stages, X-ray examination can reveal flattening of the soft cover in the area of the tuberosity of the bone, as well as signs of enlargement of the knee joint bursa. As the disease progresses, a spine-like protrusion is identified.
As for laboratory testing, it is necessary to exclude other diseases, in particular rheumatoid arthritis. With the latter, rheumatoid factor is detected in the blood. As a diagnostic test, a PCR study can be performed to exclude joint damage of infectious origin. The doctor must carry out a differential diagnosis with other diseases (osteomyelitis, rheumatoid arthritis, fractures, bone tuberculosis, syphilis).
Prices
| Disease | Approximate price, $ |
| Prices for diagnosing childhood arthritis | 2 000 — 3 000 |
| Prices for diagnosing childhood epilepsy | 3 100 — 4 900 |
| Prices for pediatric neurosurgery | 30 000 |
| Prices for treatment of childhood epilepsy | 3 750 — 5 450 |
| Prices for treatment of umbilical hernia in children | 9 710 |
| Disease | Approximate price, $ |
| Prices for hip replacement | 23 100 |
| Prices for clubfoot treatment | 25 300 |
| Prices for Hallux Valgus treatment | 7 980 |
| Prices for knee joint restoration | 13 580 — 27 710 |
| Prices for scoliosis treatment | 9 190 — 66 910 |
| Prices for knee replacement | 28 200 |
| Prices for treatment of intervertebral hernia | 35 320 — 47 370 |