The gluteal region has a complex anatomy. Pain and dysfunction in this area can be a manifestation of various conditions, such as sacroiliac joint dysfunction, gluteus maximus tendinopathy, lumbar radiculopathy, and piriformis syndrome. The scientific literature has examined the involvement of various structures in the development of symptoms.
Deep gluteal pain syndrome (DGS) is defined as pain or numbness in the buttock, hip, or posterior thigh region with radiating or radicular pain along the sciatic nerve. This condition is characterized by:
- It is not discogenic.
- Associated with damage to the sciatic nerve.
- Pinched nerve in the deep gluteal space. The most common sites of entrapment are: piriformis muscle (67.8%), greater sciatic foramen (6%), sciatic tunnel (4.7%).
OHSS is an umbrella term that represents a collection of different conditions with similar and overlapping symptoms.
Pinched pudendal nerve
The sacrotuberous ligament arises from the ischial tuberosity and attaches to the sacrum and coccyx, while the sacrospinous ligament lies at a 90-degree angle to it, deeper to the sacrotuberous ligament and attaches to the ischium. The thickness of these ligaments can lead to pinching of the pudendal nerve, called Alcock's canal syndrome or cyclist's syndrome.
In addition to pain in the gluteal region, symptoms of pudendal neuralgia include sexual dysfunction, rectal pain, fecal incontinence, and urinary incontinence. Thus, a pinched pudendal nerve can significantly impact quality of life.
This may be caused by prolonged sitting, especially when riding a bicycle, or a recent change of bicycle saddle. Symptoms are typically worsened by sitting, but sitting on the toilet has been reported to relieve pain by relieving pressure on the nerve.
Diagnostic methods
Due to the variety of factors that cause pain in the ischial bones, it is quite difficult to establish a correct diagnosis. To determine why pain occurs when sitting, the following methods are used:
- examination of the patient, collection of anamnesis;
- X-ray examination of the pelvic area in several projections;
- Ultrasound of the affected area;
- angiography;
- CT, MRI;
- laboratory diagnostics.
To determine the causative agent of infectious diseases of bone tissue, bacteriological examination of punctates or purulent contents of pathological cavities is performed.
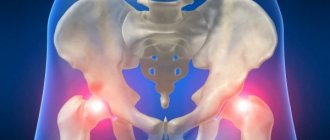
Ischiofemoral impingement syndrome
After hip surgery, especially after total hip replacement, some patients complain of pain in the back of the leg and deep pain in the buttock, especially with hip extension and adduction. Ischiofemoral pain is a rare cause of hip pain, first described in three patients after total hip arthroplasty and proximal femoral osteotomy.
The ischiofemoral space is a very small space bordering the ischial tuberosity and the lesser trochanter. Tightness and inflammation of the quadratus femoris muscle (such as with bursitis) can cause this space to narrow and affect the nociceptive structures in this area. One study (Gollwitzer, 2017) found that symptoms were associated with a decrease in the distance between the bony edges of the ischium and femur, measured using axial magnetic resonance imaging (MRI) sequences.
Symptoms:
- Deeply localized pain in the buttock, sometimes radiating to the knee.
- When running, short steps are less painful than long steps. This is due to a narrowing of the ischiofemoral space during hip extension and adduction due to an increase in step length.
- Facet-type pain at L3-4 or L4-5, which can be confused with a lower back problem. Low back pain may be associated with decreased hip extension.
- Pain due to ischiofemoral impingement syndrome intensifies with terminal (at the end of the amplitude) hip extension and adduction.
- Pain on palpation of the ischium during passive provocative movements.
- A clicking, crunching, or locking sensation in the hip joint when walking at a fast pace, caused by the lesser trochanter being forced around the ischium.
Physical examination findings are not conclusive regarding the diagnosis of ischiofemoral impingement syndrome. A combination of passive hip extension, adduction, and external rotation is used to provoke symptoms.
The long stride test (walking with long strides) has a sensitivity of 92% and a specificity of 82%.
Indirect causes of pain in the pelvic bones
The pelvic region, to which the ischium belongs, is located at the base of the spinal column, serves as the attachment point for the legs to the body, and is a container and support for internal organs and the fetus during pregnancy. In the process of life, this department is subjected to high loads. The following causes of pain in the ischium have an indirect effect:
- intense loads caused by work or sports activities, especially if the body is not adapted to such training;
- lack of physical activity, prolonged stay in a motionless position;
- excess body weight;
- overwork, stressful situations;
- smoking, drinking alcohol, drugs and certain medications;
- metabolic disorders;
- loads and restructuring of the pelvic apparatus in pregnant women;
- frequent hypothermia, exposure to drafts;
- lack of vitamins and microelements important for the normal state of the musculoskeletal system.
Lesions of the ischial tuberosities cause pain when sitting. They are support points and take on the bulk of the body. The buttock area can hurt if you are underweight due to the thin layer of fat and muscle tissue between the bone bends and the surface of the stool.
Hamstring tendinopathy
Hamstrings start at the ischial tuberosity (very close to the sciatic nerve). Proximal hamstring tendinopathy is common among long-distance runners and athletes performing sagittal plane exercises (eg, sprinting, hurdles) or change-of-direction exercises such as soccer and hockey movements.
Symptoms:
- History of repeated flexion loads. During flexion movements such as deadlifts and other flexion activities, the proximal hamstring tendon is subjected to tensile loading at its insertion on the ischial tuberosity.
- Deep localized pain in the area of the ischial tuberosity.
- The pain is worse when sitting, driving, lifting heavy objects, and running uphill. This occurs due to shear forces between the hamstring attachment and the ischial tuberosity as hip flexion increases. During running, force peaks in the late swing phase and has a second peak in the early stance phase.
- Positive straight leg raise test.
- A positive stoop test, which indicates sciatic nerve compression but does not rule out hamstring tendinopathy.
- Thickening on palpation around the ischial tuberosity.
Pain assessment should be performed as stress assessment tests are performed:
- Transition from a bridge with one leg bent at the knee to a bridge with a long lever.
- Deadlift on one leg.
- Three passive stretch tests (flexed-knee stretch, modified flexed-knee stretch, and Puranen-Orava test) have moderate to high validity and high sensitivity and specificity for diagnosing proximal hamstring tendinopathy.
Diseases that cause pain in the ischium and their characteristic symptoms
Pain syndrome when sitting is expressed when there is direct damage to the bone tissue of the tuberosities or when diseases of other anatomical structures spread to them. The absolute causes of pain in the ischial bones are:
- fractures, avulsions of bone fragments;
- tumors: osteogenic sarcomas, hemangioma;
- osteochondropathy;
- infectious diseases: tuberculosis, syphilis, osteomyelitis;
- diseases of the blood system - leukemia;
- sciatic bursitis - inflammation of the joint capsule.
One of the most common causes of bone pain is fractures resulting from injuries, falls, or compression of the pelvic bones. A separation of the ischial tuberosity can occur with a sharp contraction of the adductor muscle attached to it. The pain in such cases is stronger when moving the lower limb. Hematomas appear when large blood vessels are damaged by bone fragments.
Hemangioma of the ischium is a rare benign tumor. It most often affects the vertebrae and flat bones of the skull, followed by the bone tissue of the pelvis and lower extremities. The appearance of angiomatous nodes causes swelling or club-shaped thickening of the bone tissue, the periosteum rises. The development of neoplasms is asymptomatic and is detected accidentally during an X-ray examination. Symptoms appear when the tumor spreads and grows, leading to pathological fractures.
Osteosarcoma is a malignant tumor of bone cells characterized by rapid development and early spread of metastases. When the ischium is affected, it manifests itself as a dull pain near the hip joint. Further growth of the tumor is accompanied by lameness, sharp pain even with complete rest, and intensifies at night.
Aseptic osteochondropathy of the ischium is a non-infectious disease accompanied by necrosis of the cancellous bone that forms the posteroinferior part of the acetabulum. This leads to deformation of the ischium and destruction of the joint (Legg-Calvé-Perthes disease). Characteristic signs become pronounced at later stages. There is pain radiating to the knee, the joint loses normal mobility. There is atrophy of the muscle bundles of the lower leg and thigh, due to which the leg is shortened by 2-4 centimeters.
Severe pain in the pelvic region occurs as a result of infectious lesions of bone tissue. Hematogenous osteomyelitis of bones develops in the presence of purulent foci in the body and the spread of monocultures or associations of microbes with the bloodstream.
Post-traumatic osteomyelitis occurs due to the penetration of pathogenic microorganisms into the ischium as a complication of fractures, operations, or due to the activation of hidden foci of infection.
Osteomyelitis disease occurs with purulent-necrotic lesions of bone tissue, the formation of multiple purulent leaks in the pelvic area. The acute form of the disease occurs with signs of intoxication: chills, vomiting, headache, loss of consciousness. Local pain syndrome is pronounced, swelling of the thigh, redness of the skin, and limited movement of the limb appear. In the chronic form of osteomyelitis, the patient feels better, the pain is aching, there are no symptoms of intoxication, fistulas appear through which pus is separated.
Hematopoietic disorders in the form of malignant bone marrow tumors occur with acute pain in the bones of various locations and lead to pathological fractures. With multiple myeloma, hypercalcemia is observed, the appearance of a large amount of protein in the urine.
Inflammation of the sciatic bursa, located at the ischial tuberosity, is accompanied by throbbing pain in the right or left hip joint when bending the leg at the knee. Further development of the disease leads to the spread of the inflammatory process to nearby tissues, the pain intensifies, the entire thigh area burns and burns, especially when sitting on a hard surface.
Grade
First of all, pathology of the lumbar spine should be excluded. Physical examination includes palpation, assessment of the pelvic girdle and sacroiliac joints, and an active straight leg raise test.
Patients with sciatic nerve entrapment often have a history of previous trauma, pain with sitting, radicular leg pain, and paresthesias.
A positive March test or active straight leg raise test indicates poor control and inadequate load transfer, but neither differentiates the pathological structure.
Total range of motion and the FADIR test are used to rule out hip osteoarthritis. In addition, a negative FADIR allows the exclusion of intra-articular pathology, such as labrum damage.
A positive FABER test provokes sciatic nerve symptoms because in this position the nerve slides along the posterior border of the greater trochanter. If you experience pain in the greater trochanter during this test, it is most likely due to gluteus maximus tendinopathy.
If the patient feels pain deep in the buttock, then most likely this is compression or irritation of the piriformis muscle or one of the “deep six” muscles.
Patients with deep gluteal pain syndrome may present with altered nerve conduction tests, reflex changes, muscle weakness, and tenderness that make it difficult to differentiate the lumbar spine from the gluteal region.
The combination of a seated piriformis stretch test with an active piriformis test has a sensitivity of 91% and a specificity of 80% (Martin, 2014).
Palpation skills can be helpful in differentiating the location of pain and soft tissue texture. Use the ischial tuberosity as a reference point when attempting to reproduce the patient's pain by palpation to understand the likely source of the symptoms.
Basic therapy methods
Treatment for ischium pain when sitting is determined based on clinical manifestations and examination results of the patient. For this, depending on the case, conservative or surgical methods of therapy are used.
Drug treatment includes taking painkillers, anti-inflammatory, and antimicrobial agents. Elimination of pain often requires correction of hormonal levels and restoration of the balance of vitamins and microelements in the body.
Surgical treatment through resection of the ischium does not have a significant effect on the functioning of the lower limb, so patients do not require special rehabilitation measures. If the hip joint is not involved in the pathological process, recovery takes about a month. After 2.5-3 months, operated patients stop using orthopedic aids and begin to move independently.
Even seemingly insignificant pain in the sit bones while sitting can be a symptom of a serious illness. In order to identify pathology in the early stages of development, establish a correct diagnosis and start treatment in a timely manner, you should consult a doctor.
Differential diagnosis
The following table presents conditions that may have symptoms similar to OHSS.
- Reactive hamstring tendon, bursitis. Running uphill, deadlifting, lifting boxes/other bending load, feeling like one is sitting on a boggy mass.
- Non-discogenic sciatic nerve entrapment. Radicular pain in the leg when flexing the hip.
- Pudendal neuralgia. Increased cycling time or changing saddles is accompanied by pain. Sitting on the toilet relieves pain.
- Ischiofemoral impingement syndrome, pain in the lumbar region, pain in the sacroiliac joint, pain when extending the hip or increasing step length. History of hip injury or surgery.
- Tendinopathy of the gluteus maximus, obturator or gemellus muscles. Limping after sitting for a long time.
Mistakes in diagnosing coxarthrosis: what arthrosis of the hip joint is often confused with - coxarthrosis
A competent doctor, having studied x-rays and examined a patient suffering from arthrosis of the hip joint , can easily make the correct diagnosis already at the first consultation. That is, diagnosing this disease is usually not particularly difficult.
It is all the more surprising that in fact, the correct diagnosis is made on time only in half of the cases, and even less often. For example, often in patients who actually suffer from coxarthrosis, doctors manage not to notice arthrosis of the hip joint for several years, trying to blame all the ailments of the sufferer on problems with the lower back, on some diseases of the internal organs (for example, in women - on inflammation of the appendages, and in men - for mythical prostatitis), etc.
Conversely, it very often happens that a patient is diagnosed with “arthrosis of the hip joint” and is even sentenced to undergo joint replacement surgery in cases where there is no trace of arthrosis, and pain in the hip area is caused by something else - for example, harmless tendon inflammation or lumbar problems!
As a result, the patient then lives for a long time under the hanging sword of Damocles of the upcoming joint replacement operation, often without even realizing that he does not need the operation at all!
In order to somehow reduce this wave of general incompetence, below I will talk about those sores that are most often mistaken for arthrosis of the hip joint. And if the information offered helps at least a dozen patients save their joints and their nerves, I will already consider that I wrote this book not in vain. So:
Inflammation of the femoral tendons - trochanteritis
Perhaps the largest number of diagnostic errors when coxarthrosis is suspected is associated with trochanteritis. About a third of my patients who were diagnosed with “arthrosis of the hip joints” before our meeting did not actually have arthrosis - they just had inflammation of the femoral tendons. Although recognizing this harmless thing is not so difficult.
Trochanteritis can be either unilateral, when only one leg becomes ill, or bilateral, when the tendons on both legs become inflamed. Women get sick much more often than men, and the peak incidence occurs during menopausal changes in the body, when tendon and muscle tissue weakens. Although there are cases when young women also become ill with trochanteritis, more often after overload or injury.
Trochanteritis develops quite quickly, within 3–15 days, usually after physical exertion, carrying heavy objects, or long walking (especially on uneven terrain, climbing or descending a mountain). Also, inflammation of the femoral tendons can be triggered by injury (falling on the side, blow to the thigh) or hypothermia, a cold. Sometimes the hip tendons become inflamed after the flu.
Trochanteritis manifests itself as attacks of pain on the outer surface of the thigh - the “breeches” area. Pain occurs most often when walking or lying down on the affected side. The pain from the very beginning is quite intense, but unlike coxarthrosis, with trochanteritis there is no shortening of the leg and there is no restriction of movement in the hip joint. The leg can be easily moved to the side and rotates freely in all directions.
A person suffering from trochanteritis can freely cross his legs, tie his shoelaces without difficulty, and can easily sit “astride” on a chair, spreading his legs wide apart - unlike a person suffering from coxarthrosis, for whom these actions are difficult or not possible at all.
It is precisely this full mobility of the hip joints that should help both the doctor and the patient understand that the latter most likely does not have arthrosis, and the diagnostic search should be conducted in a different direction.
Note from Dr. Evdokimenko. Why some doctors manage to mistake tendon pain in the “breeches” area for coxarthrosis, given that the mobility of the hip joint remains ideal during trochanteritis, I don’t understand. Perhaps errors arise due to the fact that such doctors usually do not “condescend” to personally examine the patient and do not check the mobility of his joints. Moreover, they are poorly aware of the X-ray signs of arthrosis.
So, one of my patients in two clinics in a row was diagnosed with stage III coxarthrosis, and the woman was sentenced to joint replacement surgery, although the mobility of her joints was ideal. And on the x-rays there was not even the slightest hint of arthrosis! What was more here - incompetence or meanness, the desire to make money from the operation, I don’t know. But the patient said that neither in those clinics nor in the district clinic, during the year of her illness, no one even looked at her leg.
More details about inflammation of the femoral tendons are described in Dr. Evdokimenko’s book “Arthritis.”
Piriformis syndrome and radicular syndrome resulting from injuries to the lumbar spine
They are also often mistaken for coxarthrosis. But although the symptoms of the diseases are somewhat similar, a competent specialist can easily distinguish one from the other. Unlike arthrosis, with radicular syndrome and piriformis muscle syndrome, pain usually occurs abruptly, most often within 1–2 days, after lifting a heavy object, an unsuccessful movement, a sharp turn in an inclination, or after a strong mental experience or stress. In many cases, the attack is preceded by acute or chronic pain in the lower back.
In 80% of cases, the pain spreads to only one leg, and only in 20% of cases both legs are affected.
The greatest intensity of pain in piriformis syndrome is observed in the buttock area; pain in the lumbar region can also be quite severe, but may be insignificant or absent altogether.
With radicular syndrome, the pain usually extends lower. It goes from the buttock or thigh, along the back or side surface of the leg (along the “straps”) to the heel or toes. But in 90% of cases, the lower back hardly hurts or hurts just a little.
The pain can be severe both during the day and at night. Sometimes it is difficult for the patient to find a comfortable position at night, and sometimes the sick person wakes up from pain at 3-4 am. However, in half of the patients, pain occurs only when moving and walking.
In this case, there is no restriction of movement in the hip joint when rotating the leg. The leg is easily moved to the side and rotates in full. A person suffering from piriformis muscle syndrome or radicular syndrome, like a person suffering from trochanteritis, can easily sit “astride” on a chair, spreading his legs wide apart - unlike a person suffering from coxarthrosis, for whom this action will be difficult or not possible at all.
But with piriformis syndrome and radicular syndrome, acute pain often occurs in the lower back or hip (especially along the back of the thigh) when trying to lift a straight leg or bend forward while standing with straight legs. With coxarthrosis, such movements almost never cause sharp pain - unless arthrosis is combined with lumbar problems.
Arthritis
Some types of arthritis also lead to damage to the hip joints. And although this happens quite rarely, we must remember it.
In the most typical cases, the hip joints with arthritis are affected almost last, much later than other joints. And then the differential diagnosis between arthritis and coxarthrosis is not difficult - after all, by the time the hip joints become inflamed, the patient usually already knows that he has arthritis, and most often knows which one.
However, with certain types of ankylosing spondylitis and with some rare variants of reactive arthritis, inflammation of the hip joints may precede other manifestations of the disease, or even be the only symptom of the disease. And then it can be incredibly difficult to make a correct diagnosis - such inflammation of the hip joints is very easy to mistake for arthrosis. In such cases, even a competent doctor can make a mistake.
But there are still some “special” signs that make it possible to distinguish arthritic inflammation of the hip joints from arthrosis. Firstly, these types of arthritis usually affect young people, aged 15 to 40 years. And coxarthrosis, as you know, usually begins at an older age (if you do not take into account traumatic and “sports” arthrosis).
Secondly, unlike arthrosis, with arthritis pain usually reaches its greatest intensity at night, around 3–4 am. The intensity of such pain is usually very high; the pain does not decrease with a change in body position, as happens, say, with trochanteritis. When moving and walking, pain, unlike arthrosis, on the contrary, most often decreases somewhat, rather than increases. By the evening, after the sick person has “dispersed”, the pain may disappear altogether - only to flare up with renewed vigor at night, in the morning.
Another warning sign that may indicate the arthritic nature of joint inflammation is morning stiffness in the entire body and joints, which occurs immediately after waking up and then goes away within an hour or during the first half of the day. Such stiffness is typical specifically for inflammatory diseases, primarily for ankylosing spondylitis and polymyalgia rheumatica.
More details about the different types of arthritis are described in Dr. Evdokimenko’s book “Arthritis.”
Polymyalgia rheumatica
Polymyalgia rheumatica is a rather rare disease, which nevertheless cannot be discounted. Women over 50 years of age are more likely to get sick. In 90% of cases, the disease begins after suffering severe stress or a severe cold (flu).
The disease develops quite quickly, within 3–20 days. As a rule, the first symptoms of the disease are pronounced symmetrical (that is, the same on the right and left and right) stiffness and pain in the hips (the pain does not go below the knees) and in the shoulder joints.
Painful sensations are accompanied by rapidly increasing incredible weakness of the patient. Such patients are brought to the doctor literally “under arms”, but not because of pain, but precisely because of weakness. It is this extreme weakness that is the “calling card” that makes it easy to distinguish polymyalgia from most other diseases, and in particular from coxarthrosis.
Often weakness and pain with polymyalgia rheumatica are accompanied by decreased appetite, weight loss, and increased body temperature. Occasionally, the listed symptoms are accompanied by daily severe headaches, most often affecting only one half of the head - the right or left. Such pain usually “shoots” in the temple, parietal region, and in the eye area.
More details about polymyalgia rheumatica are described in Dr. Evdokimenko’s book “Arthritis”.
Article by Dr. Evdokimenko© for the book “Arthrosis”, published in 2003. Edited 2011. All rights reserved.
READ MORE:
- Symptoms of coxarthrosis
- What is arthrosis of the hip joint (coxarthrosis) often confused with?
- Causes of arthrosis of the hip joint (coxarthrosis)
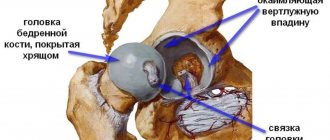
- Structure of the hip joint
- Changes in the hip joint with coxarthrosis
- Examination of a patient with arthrosis of the hip joint
- X-ray diagnosis of coxarthrosis: the most common mistakes
- Treatment of arthrosis of the hip joint: prospects
- Surgical treatment of arthrosis of the hip joint
- Therapeutic treatment of arthrosis of the hip joint
- Our best exercises for the treatment of coxarthrosis
All articles by Dr. Evdokimenko
Treatment
Principles
- It is recommended to differentiate the source of pain using knowledge and assessment skills.
- Educate your patient about the anatomy and possible causes of symptoms.
- Addressing chronic pain factors using a biopsychosocial approach.
- Load management.
Hamstring tendinopathy
- Avoid deadlifts and other bending exercises.
- Avoid hamstring stretches, such as straightening your leg to 90 degrees of hip flexion.
Sciatic nerve damage
- When driving, move your car seat closer to the steering wheel to relieve tension on the sciatic nerve.
- For runners, reducing your stride length may be necessary to relieve symptoms.
Pudendal nerve damage
- You may need to refer the patient to a physical therapist who specializes in women's or men's health to help manage symptoms such as rectal pain, fecal incontinence, or urinary incontinence.
- Refer patients over 50 years of age to a gynecologist to understand their hormonal status. Lifestyle changes and weight loss are also recommended.
General recommendations
- Weight control.
- Lifestyle changes.
- Sleep hygiene.
- To give up smoking.
Myofascial release and manual therapy, combined with appropriate rehabilitation and specialist consultation, are useful clinical tools in the treatment of deep gluteal pain syndrome.
Image-guided anesthetic blocks or steroid injections may also be effective.
Exercises
Principles for selecting exercises:
- Try limiting exercise to 15 or 20 minutes per day to improve patient compliance and adherence.
- Avoid stretching at the beginning of treatment for tendinopathy to reduce the strain on the tendon and possibly return to it later when the pain has subsided.
- When treating tendinopathy, aim to keep pain below 5 on a scale of 10 and not worsen for 24 hours afterwards, especially when performing functional exercises such as step-ups, single-leg squats, dynamic lunges and split squats. .
- When performing the piriformis stretch with the hip flexed at 90 degrees, the hip should be externally rotated. The piriformis muscle is an abductor and external rotator of the hip below 45-60 degrees of hip flexion, but functions as an internal rotator above 60 degrees of hip flexion.
- Combine exercises with neurodynamic techniques such as sciatic nerve glides.
- Recommend glute strengthening in the form of bird-dog exercises, split squats, and functional loading exercises.
- Progressive loading with emphasis on hip extensors, abductors and external rotators.