- Treatment of coxarthrosis in our clinic
- Conservative treatment of coxarthrosis
- Treatment of coxarthrosis using UVT
- How is the treatment procedure for coxarthrosis carried out?
- Side effects in the treatment of coxarthrosis
- Coxarthrosis - information about the disease
- Clinic and diagnosis of coxarthrosis
- Conservative methods of treating coxarthrosis
- Shock wave therapy in the treatment of coxarthrosis
- SWT in the treatment of coxarthrosis: a review of scientific literature
- conclusions
Treatment of coxarthrosis in our clinic
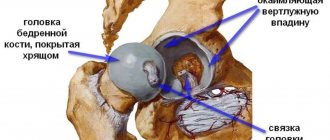
Our clinic has been successfully treating coxarthrosis for quite a long time, using an integrated approach. Coxarthrosis is a degenerative-dystrophic disease of the hip joint, which affects the articular joints of the femur at the point of its articulation with the acetabulum of the pelvis. As a result, the cartilage tissue is gradually destroyed, the joint capsule and ligaments are involved in the inflammatory process, and bone growths appear. All this leads to pain and swelling of the joint.
Causes of coxarthrosis: joint injuries, congenital anomalies of joint development, aseptic necrosis of the femoral head, heredity and hormonal changes, systemic autoimmune diseases.
The main symptoms of cosarthrosis : pain and crunching in the joint area, limited mobility, lameness when walking.
The diagnosis is made by an orthopedic doctor or surgeon based on complaints, medical history, examination and x-ray examination of the hip joint. Sometimes an MRI is prescribed.
Contraindications to surgery for coxarthrosis
Surgical interventions for coxarthrosis have a large number of contraindications, including:
- pregnancy, breastfeeding,
- joint infection,
- bleeding disorder,
- severe diseases of the blood, heart, liver, kidneys,
- cardiac, respiratory failure,
- 3-degree obesity,
- serious muscle changes in the area of prosthetics and a number of other contraindications that the doctor must warn about.
Conservative treatment of coxarthrosis
We use both classical conservative approaches in the treatment of coxarthrosis and use new treatment methods. It is impossible to stop the progression of the disease or slow down its course at stages II and III; medical care is palliative in nature - reducing the severity of symptoms. Patients are prescribed a course of exercise therapy, weight correction, and physiotherapeutic procedures. Injections of hormonal drugs give mixed results, and they also have many side effects.
Many years of experience show the ineffectiveness of conservative therapy for coxarthrosis, so patients are often offered surgery - a complete replacement of the hip joint. It is highly effective, but postoperative complications often occur. In addition, this is an expensive procedure.
In recent years, researchers in different countries have reported the benefits of shock wave therapy in the treatment of patients with coxarthrosis. We use shock wave therapy as one of the methods as part of complex therapy.
Content
- Morbidity statistics
- Causes of coxarthrosis
- Symptoms of the disease
- Stages of osteoarthritis
- initial stage
- Stage 2
- Stage 3
- Stage 4
- Diagnostic methods
- Treatment methods
- Drug therapy
- Physiotherapy
- Injection methods
- Contraindications to treatment
- New methods of treating coxarthrosis
- Duration of treatment
- Which doctor should I contact?
- Treatment methods used at the Stoparthrosis clinic
- Why do they contact us?
- Reviews from our patients
- Sign up for treatment
Coxarthrosis develops as a result of damage to the articular cartilage of the hip joint, caused by the combined effects of genetic, metabolic, biochemical and mechanical factors on the joint tissue.
Treatment of coxarthrosis using UVT
In our clinic, focused and radial shock wave therapy is used to treat coxarthrosis as part of a comprehensive treatment. According to recent scientific publications and our practice, the UVT method has established itself as part of a complex treatment, giving good results in combination with conservative methods.
A patient visiting our clinic for the first time undergoes an initial appointment with an orthopedist-traumatologist. The patient's complaints and medical history are analyzed and an X-ray or MRI of the joint is performed.
A complex treatment is prescribed, which includes, along with other methods, a course of UVT procedures, usually from 5 to 10 procedures with an interval of 3 to 7 days.
The interval between procedures is individual and can be reduced if there are no side effects and the procedures are well tolerated. The duration of the procedure is from 20 to 40 minutes. (in some cases more).
How is the treatment procedure for coxarthrosis carried out?
The UVT procedure is part of a complex treatment and is aimed at relieving the most disturbing symptoms - pain, swelling, and limited mobility in the joint.
According to scientific articles on the treatment of coxarthrosis, a good positive effect was noted in stopping degenerative changes, reducing pain and swelling, and mobility of tissues around the joint. The procedure affects the articular joints of the femur at the point of its articulation with the acetabulum of the pelvis, all tissues adjacent to the joint, including muscles and their attachments, which often cause pain.
The procedure itself is performed in combination using focused and radial applicators. Radial shock wave is most often used at the beginning of the procedure. The radial wave is used not only when working in the joint area, but also with adjacent regions, since the pathological process often affects adjacent tissues. The radial applicator targets tissue at shallow depths and results in many beneficial long-term “tissue” effects (reduced inflammation, capillary sprouting, stem cell influx, etc.). These effects do not appear immediately, but after a fairly long period of time - from 3 weeks, and develop over several months, leading to deep tissue regeneration.
After the radial wave, a focused wave is used, which penetrates deep into the tissue, reaching the area of pain, and causing loosening, analgesic and anti-inflammatory effects. At the same time, the doctor carefully directs the focal spot area of the device to the affected areas; when working with pain syndrome, it is important to get to the places of greatest pain, from which the procedure may cause some discomfort, which does not harm health in any way and should be perceived as a benefit. Thus, the effect of a focused wave is usually instantaneous, and increases with each procedure, and is aimed mainly at relieving bothersome symptoms (pain, tightness), while a radial wave has a regenerative effect, stopping degenerative changes in the joint itself, which is usually noticeable starting from the 3rd week of treatment onwards.
Coxarthrosis. Hip replacement
The main indication for hip replacement is arthrosis deformans (coxarthrosis).
Hip replacement is a fairly frequently performed operation. On average, 1 adult out of 1000 needs it annually. For example, for Moscow this is about 8000 - 9000 patients per year. Although, it should be noted, there are still no clear and reliable statistics on this matter.
For patients, the main thing in hip replacement surgery is, perhaps, that the indications for the operation are determined not so much by the surgeon as by the patient himself. And the main thing here is the loss of the previous quality of life, which, in the vast majority of cases, together with the diagnosis, is an indication for hip replacement. Of course, the doctor’s tasks are defined and unchanged - to make a diagnosis, select the appropriate set of artificial joints for a particular person, tell the patient about all possible treatment methods, and perform an operation. Only surgery allows, in this case, to restore the seemingly forever lost quality of life.
- Causes and types of deforming arthrosis of the hip joint
In order to select an adequate set of endoprosthesis, the doctor needs to know the cause of the development of arthrosis. Most often this is:
Dysplasia (dysplastic coxarthrosis).
Dysplasia is abnormal development, underdevelopment of the components of the hip joint. More often - the acetabulum. Purely mechanically (although the pathological processes are deeper), the acetabulum takes on a greater load, since its dimensions are smaller than normal. As a result, early wear of the articular cartilage of both the socket and the head of the femur occurs. As a result, the joint itself quickly becomes unusable. The extreme degree of dysplasia is a congenital subluxation or even dislocation of the hip, which for some reason was not corrected in childhood. Such patients are often encountered today. Dysplastic coxarthrosis is often accompanied by limb shortening. Orthopedists at the Ilyinskaya Hospital are experts in this difficult issue – endoprosthetics for severe dysplasia of the hip joint, including those with shortened limbs. Of course, you need to understand that shortening is a serious problem. After all, when a limb is shortened for a long time, the muscle that is normally tense and not tense when the length of the leg is lost degenerates into connective tissue. And the stability of the joint, in fact the absence of lameness, depends not only on the correct ratio of bones (elements of the endoprosthesis) in the joint, but also on muscle strength. If a patient does not agree to undergo joint replacement surgery for a long time, the shortening increases over the years. The surgeon restores the length, but the lameness remains because the muscle component does not work. In this case, the muscles are no longer able to support the joint in a stable position. You need to know this. You need to remember this.
Joint injury, fracture (post-traumatic coxarthrosis).
The name says it all: the patient has a history of trauma. This is usually a fracture of the neck, head of the femur or acetabulum. In this case, often, even with timely and adequate surgical treatment, the elements of the joint are destroyed. As a result of this process, indications for hip replacement arise.
Aseptic necrosis.
It develops both in childhood (Perthes disease) and in adults. As a result of a number of interrelated pathological processes, instead of living bone tissue of the femoral head, dead bone tissue is formed. As a rule, there are no clinical manifestations of aseptic necrosis in adults, and there are no pain sensations or they are minimal. In areas of bone necrosis, empty spaces called cysts form over time. Due to the load, the cartilage above the cysts begins to break, at which point pain appears. As a result of these microfractures, deformation of the femoral head develops and congruence in the joint is lost.
Post-infectious coxarthrosis.
Today there are fewer such coxarthrosis. But they still occur as a consequence of a hematogenous inflammatory disease or purulent complications of a previous surgical intervention. Previously, joint tuberculosis was a fairly common cause. Endoprosthesis replacement for post-infectious coxarthrosis is a rather difficult task, since the inflammatory process can recur if the joint components are incorrectly selected.
Coxarthrosis that developed against the background of rheumatic diseases.
This group includes all rheumatoid arthritis, psoriatic, gouty arthritis, ankylosing spondylitis and other diseases, the outcome or manifestation of which in many cases is deformation of the femoral head and acetabulum with loss of both congruence and cartilaginous cover. A feature of endoprosthetics in such cases is that coxarthrosis is accompanied in these patients by osteoporosis, on the one hand, and on the other hand, damage to internal organs and systems with the development of concomitant diseases. This requires a combination of the surgical skill of an orthopedist with a comprehensive general therapeutic approach to pre- and postoperative patient management. This is exactly the approach that the doctors at Ilyinskaya Hospital demonstrate.
Idiopathic (primary) coxarthrosis.
This means that the specific cause of coxarthrosis in this particular case could not be determined. This condition is common and with age the number of primary coxarthrosis only increases. In this case, without any obvious reason, a completely healthy person experiences pain in the hip joint, often radiating down the thigh to the knee joint and below. An X-ray examination reveals deforming arthrosis of the hip joint. It is believed that metabolic disorders, excess weight and inflammatory reactions as such play a large role in the development of idiopathic coxarthrosis. In this case, the cartilage is mechanically erased, and the products of its breakdown cause aseptic (microbial-free) inflammation, which aggravates the situation. It is not for nothing that the word “arthrosis” practically never appears in English terminology. This is always “arthritis”, that is, inflammation.
- What is an endoprosthesis and what components does it consist of?
The main working component of the hip joint endoprosthesis is the so-called friction pair: the head and the socket element in which this head rotates. These components can be different: ceramics-ceramics (high-strength ceramics), ceramics-polyethylene, medical steel-polyethylene. Each friction pair has its own indications and contraindications. Not long ago, a metal-to-metal friction couple was popular. However, it has shown its low effectiveness and even the ability to cause some concomitant diseases. At the moment, we are not focusing on this friction pair in hip replacement.
Hip endoprosthesis
Image source: shutterstock.com/Alex Mit
And so, a friction pair is an artificial head and an artificial element of the acetabulum, providing the possibility of movement in the joint. However, in order to secure the head to the thigh, a leg is needed. In this case, the leg, like a rasp rod, is installed in the canal of the femur. And the head is already put on the leg. The stem can be installed either by press-fit or with bone cement. It is on this basis that cemented, cementless and combined (mixed) endoprosthetics are distinguished. Bone cement is a material similar in composition to chemically cured dental fillings. In this case, it fills the canal in the femur. While the cement has not hardened, a leg is installed in the canal, then the cement hardens. One of the infrequent but occurring complications associated specifically with cementing is a sharp increase in temperature and pressure in the medullary canal of the femur. This occurs at the moment the cement hardens, due to which an increase in the patient’s body temperature and even microembolism is possible. Therefore, where the use of cement can be avoided, we avoid it. Where this is not possible, our hospital’s anesthesiologists provide reliable drug protection for the patient during and after surgery.
The second component of the friction pair - the so-called liner - is installed in the cup, which, in turn, is attached to the acetabulum. There are cups that do not require the use of an insert. The cup can also be installed using press-fit (tight fit) or with bone cement. Bone cement for the acetabulum has to be used more often when we perform revision arthroplasty rather than primary arthroplasty. This is what one of the assembled artificial uncemented hip joint layouts looks like:
Installed hip endoprosthesis
Image source: shutterstock.com/Alex Mit
- Types of endoprosthetics
There are primary and revision endoprosthetics:
Primary endoprosthetics
– this is an endoprosthetics operation, as the name suggests, performed on a patient for the first time. Most often, during this operation, the patient is in a position either on his back or on his side, rarely on his stomach. It depends on the preferences of the surgeon, on the characteristics of coxarthrosis, on individual anatomy, on the characteristics of the chosen prosthesis, and so on. On average, the operation lasts from 40 minutes to one and a half hours.
Revision endoprosthetics.
The endoprosthetic operation has already been performed (possibly quite successfully), but 20-25 years have passed since then, the prosthesis has worn out, and it is necessary to replace either the entire endoprosthesis or its individual components. However, if the previous endoprosthesis was installed with obvious technical and technological errors, then revision endoprosthetics is also performed. Revision endoprosthetics is the highest class of surgery. Powerful resuscitation and anesthesiological support and an integrated approach to pre-, intraoperative and postoperative patient management are required. To carry out such operations, you need serious, expensive equipment, which is equipped in the wards and operating rooms of the Ilyinsk Hospital.
- Pain relief during and after surgery
The recognized worldwide safe standard of pain relief during hip replacement surgery is spinal anesthesia. However, in some cases other types of pain relief are possible. Anesthesiologists at the Ilyinskaya Hospital have the full range of necessary benefits and are equipped with the most high-tech equipment to perform any type of anesthesia that the patient requires. In the postoperative period, proper management is carried out by the “hospital pain service” - a unique unit of our hospital that is able to cope with pain of any severity.
- Postoperative rehabilitation
Postoperative rehabilitation is an issue that always worries our patients. But their worries are largely unfounded. If the process is not started, and coxarthrosis has developed for a relatively short time, then the required rehabilitation efforts are not so great. But still very necessary. Our rehabilitation specialists will help the patient get back on his feet, start walking with the help of a walker or crutches, use hygiene products, teach him to walk up the stairs, explain the rules of behavior and, ultimately, help restore lost muscle strength. If the process is quite advanced, or the operation is revision, then the efforts of the rehabilitation team can hardly be overestimated. Our hospital has an excellent rehabilitation room and qualified rehabilitation specialists. There are even special wards in which you can comfortably stay specifically for in-depth and long-term rehabilitation.
Coxarthrosis - information about the disease
Coxarthrosis is a severe degenerative-dystrophic disease of the hip joint, which affects the articular joints of the femur at the point of its articulation with the acetabulum of the pelvis. As a result, the cartilage tissue is gradually destroyed, the joint capsule and ligaments are involved in the inflammatory process, and bone growths appear. All this leads to pain and swelling of the joint.
Causes and factors for the development of coxarthrosis:
- joint injuries, both acute and chronic;
- congenital anomalies of the development of the hip joint (dysplasia) or other parts of the lower extremities (shortened legs, foot deformities);
- aseptic necrosis - non-infectious death of the tissue of the femoral head;
- sedentary lifestyle and excess weight of the patient;
- hereditary predisposition;
- hormonal changes, for example in women after 40 years;
- systemic diseases (rheumatoid arthritis);
- idiopathic arthrosis (arthrosis of unknown etiology).
Clinic and diagnosis of coxarthrosis
Main symptoms of the disease:
- pain in the joint area. Occurs in the initial stage during physical activity, in the late afternoon after a working day. Over time, when surrounding tissues are involved in the process, pain bothers the patient even at rest;
- crunching in the joint when moving;
- limitation of joint mobility;
- lameness when walking.
The diagnosis of the disease is made by an orthopedic doctor based on the clinic, X-ray or MRI data.
Rice. 1. Coxarthrosis according to radiography
Stages of development of coxarthrosis:
- Stage I. The pain only bothers me during exertion. Restrictions in movement and changes on radiographs are minor.
- Stage II. The pain occurs at rest. Movement restrictions are pronounced. The x-ray reveals moderate changes - narrowing of the joint space, bone growths are visible.
- Stage III. The pain is almost constant. Restrictions in movement are significant, severe stiffness, the joint is swollen, the limb is shortened. On the radiograph, the joint space is not determined; significant bone growths are noted. At this stage, the joint is virtually destroyed.
Rice. 2. Stages of arthrosis of the hip joint (coxarthrosis)
Morbidity statistics
Women suffer more often than men; patients in the older age group (50-70 years) predominate. The highest incidence rates were recorded in North America (m. 1.6% - 2.5% f.), the lowest in East Asia (0.4% - 0.3%, respectively). Overweight people are more susceptible to coxarthrosis than others due to constant overload of the joint.
The disease progresses gradually over several years. Cartilage does not have nerve fibers, so the pain is moderate, the disease begins with discomfort and fatigue. A person experiences difficulty getting up from a chair, bed, sofa, and has difficulty climbing stairs. Prolonged sitting causes painful steps after standing up; relief comes after a few steps, when the person disperses. Walking for a long time during the day causes noticeable pain in the evening, which subsides after rest.
Conservative methods of treating coxarthrosis
Medical care for patients with coxarthrosis of the hip joint is palliative. It is impossible to stop the progression of the disease or slow down its course at stages II and III. All a doctor can do is reduce the severity of symptoms. Patients are prescribed a course of exercise therapy, weight correction, and physiotherapeutic procedures. Injections of hormonal drugs give mixed results, and they also have many side effects.
Many years of experience show the ineffectiveness of conservative therapy for coxarthrosis, so patients are often offered surgery - a complete replacement of the hip joint. It is highly effective, but postoperative complications often occur. In addition, this is an expensive procedure. In the last few decades, shock wave therapy (SWT) has been used for coxarthrosis.
Shock wave therapy in the treatment of coxarthrosis
The SWT procedure itself is one of the methods of complex treatment (along with conservative methods) and is performed in combination using a focused and radial applicator. A radial shock wave is most often used at the beginning of the procedure, a focused one at the end. With a focused wave, the effect is usually instantaneous, and increases with each procedure, and is aimed mainly at relieving bothersome symptoms, while with a radial wave, the effect is regenerative, stopping degenerative changes in the joint itself, usually noticeable from the 3rd week of treatment onwards. . A separate task is the partial destruction of bone growths as a consequence of degenerative changes in the joint, using powerful focused shock wave therapy.
In general, these effects help reduce inflammation, accelerate tissue repair and regeneration, destroy bone growths, reduce pain and normalize joint function.
Rehabilitation after surgery for coxarthrosis
Rehabilitation after endoprosthetics usually takes from six months to 8 months. It can be accelerated using the methods of oriental medicine and physical therapy.
Massage helps to increase blood flow to the operated area, activate the processes of healing, restoration, fusion and engraftment. With the help of moxotherapy, the body's regenerative reserves are mobilized. Herbal medicine reduces inflammation. Acupuncture has an analgesic effect. The combined use of massage and acupuncture helps reduce swelling, improve lymph movement, and relieve tension.
How to use class=”aligncenter” width=”992″ height=”247″[/img]
or call +7 Moscow
Free consultation Survey, examination, pulse diagnostics from 30 minutes
Diagnostics Ultrasound, MRI, Laboratory tests (as prescribed)
Treatment Individual plan
SWT in the treatment of coxarthrosis: a review of scientific literature
Italian scientists investigated the biochemical and molecular mechanisms of the effect of shock waves on human cartilage cells. They carried out their work on a cell culture specially bred for this purpose. They noted that when exposed to shock waves, the progressive dedifferentiation of bone cells slows down significantly.
Brazilian researchers studied the effect of shock wave therapy on the effectiveness of treatment of coxarthrosis in dogs. For their work, they selected 30 animals with bilateral lesions of the hip joints. All studied individuals received 3 shock wave treatment sessions with an interval of 1 week. One joint was selected for exposure, and the second was not subjected to therapy, in order to then compare the effectiveness of the chosen technique.
After completion of the course of treatment, an increase in the vertical force for the affected limb was noted from 2 to 12.7% of the animal’s body weight. Limb strength levels also increased by 2% of body weight. Dog owners also noted a decrease in pain and lameness in their pets during walks.
The authors of the study concluded that the use of shockwave therapy for coxarthrosis is effective.
conclusions
Coxarthrosis is a serious disease that destroys the hip joint and leads to disability. Due to the widespread prevalence and low effectiveness of conservative therapy, the disease has become not only a medical, but also a social problem. The percentage of disability due to coxarthrosis is one of the consistently high rates in orthopedics.
In recent years, endoprosthetics have become increasingly used in the treatment of the disease. However, the high cost of the operation and long rehabilitation after it do not contribute to its widespread implementation.
One of the new effective techniques, as part of the complex treatment of coxarthrosis, is shock wave therapy. Due to the positive effect on tissue, shock waves lead to a decrease in the intensity of pain, partial restoration of joint function (depending on the stage of the disease) and improvement of its mobility. Moreover, the effect of treatment is often more lasting than that of traditional therapy.
The technique is economically accessible, does not require preparation and rehabilitation, and there is no need for anesthesia. After it is performed there are no side effects or complications. The procedure can be performed in an outpatient setting.
Pros and cons of prosthetics
If the operation to install the prosthesis is performed efficiently, the patient can soon begin to walk and restore a normal lifestyle. Success is largely determined by the quality of the implant, as well as the skill of the doctor. An important aspect is luck, which you need to have in order to get into the positive part of the statistics, since in many patients prosthetics do not give the expected effect.
The reasons for “bad luck” can be poor-quality implants, errors during surgery, infection, or the individual characteristics of the patient. Despite objective improvement in joint function, pain may persist for a long time, requiring constant medication. However, in general, a mechanical joint provides a fairly high quality of life compared to baseline in patients with advanced disease.
The obvious disadvantages of prosthetics are the high cost and the undesirability of a compromise between price and quality. It is also impossible to predict the development of pain after surgery. Ideally, replacing a joint with a mechanical one should be done on both sides, and this makes the procedure even more expensive.