The term “myositis” is collective and is used to refer to those pathological conditions that are accompanied by inflammation of the skeletal muscles of various natures. Depending on the etiology of diseases and their symptoms, modern medicine divides them into several main types, which, in turn, are classified into subtypes. There are also mixed types of myositis, the symptoms of which include components of different categories of pathology. In accordance with the classification, it is customary to distinguish the following types of myositis:
- infectious;
- traumatic;
- parasitic;
- purulent;
- toxic.
In addition, the following diseases are classified as myositis:
- myositis ossificans;
- polymyositis;
- neuromyositis;
- dermatomyositis.
You can undergo a course of treatment for myositis at the CELT multidisciplinary clinic. In order to make an appointment with our specialists, you do not need to have a residence permit in the capital. Anyone can become our patient!
At CELT you can get advice from a neurologist.
- Initial consultation – 4,000
- Repeated consultation – 2,500
Make an appointment
Etiology
As already mentioned, the factors leading to the occurrence and development of myositis of the muscles of the neck, back and other parts of the body can be very different. Often the disease occurs as a result of autoimmune inflammatory processes; quite often it is provoked by a number of diseases of an infectious nature: from influenza to sore throat.
The following can lead to myositis of the muscles of the back and other parts of the body:
- injuries;
- long-term intense loads;
- muscle cramps that occur while swimming;
- long stay of the body in an uncomfortable position;
- severe hypothermia of muscles.
Do not forget about myositis caused by stress and depression.
Myositis of the thoracic spine: symptoms, causes, diagnosis, treatment
The development of myositis of the thoracic spine leads to inflammation of the intercostal muscles. This disease most often affects older people, as well as people with weak immunity, and those who often experience increased physical activity. Myositis is extremely dangerous, so if left untreated, it can become chronic and cause muscle atrophy.
Reasons for appearance
Thoracic myositis can develop due to:
- Parasitic infection;
- Weakened immunity;
- Diseases of the spinal column, for example, osteochondrosis or scoliosis;
- Increased physical activity;
- Hypothermia;
- Prolonged contact with hazardous chemicals and other toxic compounds;
- Previously received injuries.
What is chest myositis?
Depending on the number of muscles affected, the described disease is of two types. The first of these is polymyositis. In this case, only a couple of muscles become inflamed, which leads to moderate pain. The second type is dermatomyositis. It is more dangerous because... Due to chest pain, complications arise, for example, swelling of the eyelids.
There is a division of thoracic myositis into separate forms. According to this classification it is:
- Infectious;
- Parasitic;
- Acute purulent;
- Intercostal;
- Post-traumatic;
- Autoimmune.
Symptoms
In the early stages of development, chest myositis has symptoms characteristic of diseases of the heart, bronchi and lungs. In particular, unpleasant sensations appear in the chest, back pain, and muscles ache. In addition, it is not excluded:
- The appearance of a cough;
- Shortness of breath;
- Recurrent headache;
- The appearance of swelling;
- Swelling;
- Increased body temperature;
- Difficulty swallowing.
Sometimes people mistake pain due to myositis for myocardial infarction, so they use nitroglycerin. Be carefull! With the disease described, the chest muscles take the form of hard nodules, which is not typical for heart disease.
Establishing diagnosis
If you suspect that you have thoracic myositis, then visit the clinic and undergo a medical examination. Based on the results of a blood test, electromyography, magnetic resonance imaging and biopsy, the doctor will make the correct diagnosis and prescribe the most appropriate treatment. There is no point in delaying a visit to a specialist, because in this case, wasting time is not in the patient’s sphere of interest.
More about treatment
Complex therapy allows you to get rid of myositis of the thoracic spine. It includes several treatment methods at once. The first of them is taking medications to relieve pain. Doctors usually prescribe Ortofen, Diclofenac or Ketonal. In addition, it is possible to prescribe Trental or Pentoxifylline to improve blood flow and muscle relaxants that eliminate muscle spasms.
The second method of treatment is the use of ointments that have an anti-inflammatory effect. The most effective drugs are Finalgon, Apizartron and Voltaren. The exact dosage of the gel, as well as the time and frequency of its use, is determined by the attending physician.
If a patient has infectious myositis, then the most common treatment method is antibiotics. If an acute purulent form of the disease is diagnosed, then an operation is prescribed, during which areas susceptible to decay are surgically removed.
Almost always, complex therapy includes massage of the back and, in particular, the thoracic spine. As a rule, the doctor prescribes a massage course consisting of 2-3 dozen sessions.
Another component of complex treatment is physiotherapeutic procedures. Among them, it is necessary to highlight magnetic therapy, ultrasound and electrophoresis.
To everything written above, it should be added that during the treatment of thoracic myositis, the patient must adhere to a diet, give up alcohol and other bad habits.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Clinical manifestations
Soft tissue MRI
- Cost: 6,000 rub.
More details
The main clinical manifestation of this pathological condition is pain localized in the inflamed muscles. So, for example, with myositis of the chest, pain is felt in it. It intensifies with pressure on the muscle tissue, and also appears more and more clearly as the disease develops and at night. Painful symptoms are accompanied by the following:
- limitation of joint mobility;
- hyperemia of the skin over the affected area;
- feeling of weakness in the muscles;
- atrophy of skeletal muscles (with the development of the disease).
Pectoralis minor syndrome
Pectoralis minor syndrome is when this muscle pinches the nerves and vessels located next to it.
Pectoralis minor syndrome is also called Wright's syndrome, Wright-Mendlovich syndrome or hyperabduction syndrome. It was described in 1945 by two American doctors - Wright and Mendlovitch, independently of each other. The word "hyperabduction" means significant abduction of the arm to the side.
The pectoralis minor muscle is located on the ribs, just below the collarbone. It has the shape of an elongated triangle, the apex of which faces the shoulder joint and the base faces the sternum. Directly under the muscle, more precisely, between the muscle and the ribs, nerves and blood vessels pass. They go from the cervical spine to the arm to provide innervation and blood supply to the arm. This arrangement of the neurovascular bundle, when it lies on the ribs and is covered with muscle on top, resembles a tunnel. When there is spasm or shortening of the pectoralis minor muscle, in this tunnel, between the muscle and the ribs, pinching of the neurovascular bundle occurs - this is the pectoralis minor muscle syndrome or Wright Mendlovich syndrome. And at its core, this is tunnel syndrome. It can occur when the arm is moved to the side for a long time, when the muscle tightens and presses the bundle to the ribs. This is possible during surgery, an IV, deep sleep, or during certain types of work that require this hand position. Significant abduction of the arm - hyperabduction - gave another name to this syndrome - hyperabduction syndrome.
Our doctors
Pankov Alexander Rostislavovich
Neurologist
40 years of experience
Make an appointment
Novikova Larisa Vaganovna
Neuropathologist, Candidate of Medical Sciences, doctor of the highest category
Experience 39 years
Make an appointment
Symptoms
The muscles most often affected are the neck, lumbar region, chest, and calf muscles. Severe pain forces a person to take a forced position. Patients try to avoid sudden movements and sometimes try to breathe shallowly if the painful process involves the muscles of the abdomen and back.
Sometimes pain can go away after a few days if the person is provided with warmth, rest, care and painkillers. Very often, without proper treatment, the disease can become chronic. The pain may worsen in the cold. The affected muscles swell, become dense, tense, and nodules can be felt in them.
Myositis
MYASTHENIAS is a neurological disease caused by a disorder of neuromuscular transmission, manifested by weakness and pathological fatigue of skeletal (striated) muscles.
Myasthenia gravis is associated with the formation of antibodies against receptors located at the junction of nerve and muscle tissue (neuromuscular synapse), which causes a disruption in the conduction of impulses to the muscle. The thymus gland appears to play an active role in the autoimmune reaction.
Clinical picture. Myasthenia gravis can occur at any age, but the highest probability is observed in 2 age categories: 20-40 years (during this period women are more often affected) and 65-75 years (during this period women and men are affected equally often). In most cases, the disease involves the eye muscles; patients complain of drooping eyelids and double vision. Over the next 1-2 years, in most patients, the process may spread with the addition of weakness of the facial and bulbar muscles (impaired swallowing and choking, hoarseness and unclear speech), weakness of the neck muscles (inability to hold the head), as well as muscles of the limbs and torso. But in a quarter of cases, the disease does not spread beyond the external muscles of the eye (ocular form). Less commonly, the disease begins with bulbar disorders (dysphagia-impaired swallowing or dysphonia-hoarseness) or weakness in the limbs. If by the end of the 2nd year generalization has not occurred, then the process will most likely remain local.
Evidence in favor of myasthenia gravis:
- Marked fluctuations in symptoms throughout the day and from day to day;
- Early asymmetrical involvement of the external eye muscles with intact pupillary reactions;
- An increase in symptoms in the form of muscle weakness during physical activity (for example, increased dysphagia during eating, and dysphonia during a conversation) (the phenomenon of pathological muscle fatigue) and the phenomenon of generalization of muscle weakness (for example, increased ptosis after stress on the arm muscles);
- Selectivity of muscle involvement (neck flexors are often weaker than extensors, and in the arms, weakness is more pronounced in the forearm extensors). Preservation of tendon reflexes, absence of sensory disturbances, pelvic disorders and amyotrophies.
Patients with generalized myasthenia sometimes experience rapid deterioration of their condition with the development of respiratory failure associated with weakness of the respiratory muscles or bulbar muscles (myasthenic crisis). It can occur suddenly due to an unfavorable course of the disease (sometimes a crisis is the first manifestation of myasthenia gravis), as a result of impaired absorption of an antichloroesterase agent (AChES), or as a complication of an infection or taking medications that interfere with neuromuscular transmission, for example, magnesium. Severe respiratory failure during a crisis can develop very quickly, within a few minutes. Its approach is indicated by: shortness of breath, inability to swallow saliva and keep the head straight, weakening of the voice, orthopnea (forced sitting position taken by the patient to facilitate breathing with severe shortness of breath). In this case, patients require emergency hospitalization.
Less commonly, the increase in muscle weakness and respiratory failure is caused by an overdose of AChES, an excessive amount of which blocks neuromuscular transmission (cholinergic crisis). Clinically manifests itself: narrow pupils, constant muscle contractions and twitching, increased secretion of the salivary gland, increased peristalsis of the gastrointestinal tract, diarrhea, vomiting, bradycardia.
Diagnostics. To confirm the diagnosis, a proserine test is performed (2 ml of proserine solution is injected subcutaneously, after which the effect is observed for 40 minutes). Before the test, muscle weakness is aggravated by loading. The diagnosis is confirmed using electroneuromyography. Antibodies to acetylcholine receptors can be detected in the vast majority of patients. In adults with a confirmed diagnosis of myasthenia gravis, CT of the anterior mediastinum is indicated to exclude thymoma, which is detected in 10-15% of patients. In others, hyperplasia or, much less frequently, atrophy of the thymus gland may be detected. With myasthenia gravis, thyrotoxicosis, thyroiditis, rheumatoid arthritis, systemic lupus erythematosus and other autoimmune diseases are more common.
Treatment. The most commonly used antichloinesterase agents (ACHES): kalimine, prozerin. When taken orally, its effect begins within 10-30 minutes, reaches a peak after 2 hours, and then gradually weakens over 2 hours. Although Kalimin is effective in most patients, only a small proportion of them experience complete remission of symptoms. Frequent side effects are abdominal pain, nausea, diarrhea, increased salivation.
Corticosteroids (prednisolone) are prescribed if kalimine is insufficiently effective. They cause improvement in 70-90% of patients, but in the first 3 weeks, especially if treatment is started with a high dose, muscle weakness (including bulbar and respiratory) may increase.
Immunosuppressants (azathioprine, cyclosporine A and cyclophosphamide) are prescribed for generalized or bulbar forms of corticosteroid intolerance, as well as in cases where the side effects of steroids do not allow an effective dose to be achieved.
In some cases, surgical treatment and removal of the thymus gland are indicated. Thymectomy is indicated in young patients (under 60 years of age) with a generalized form of the disease, as well as in the presence of thymoma.
If signs of myasthenic crisis appear, the patient is urgently hospitalized in the intensive care unit. The patient is given oxygen (via a mask or nasal catheter). In the absence of signs of AChES overdose (!), 1-2 ml of proserin solution is administered subcutaneously. To eliminate side effects, atropine is administered simultaneously. The best results during a crisis are achieved by plasmapheresis (usually 5-6 sessions over 2 weeks). A good effect can be obtained with the help of intravenous administration of immunoglobulin.
Patients with myasthenia gravis should be under the supervision of a neurologist for timely correction of therapy and early detection of worsening of the disease.
Classification
Myositis of the pectoral muscles can be classified according to several criteria. According to the course, acute and chronic forms of the disease are distinguished. Acute has clear clinical symptoms and causes significant discomfort to the patient.
Without timely treatment, which should be carried out by a doctor, it can develop into chronic inflammation. With it, episodes of relative well-being (remission) are replaced by exacerbation.
Important! Separate, more common forms of pathology are dermatomyositis (combined damage to muscles and skin) and polymyositis.
Dermatomyositis is also characterized by skin symptoms.
Also, diagnostic and treatment protocols - standard medical instructions - highlight the following variants of muscle inflammation:
- acute purulent (usually caused by infection with pathogenic bacterial flora - staphylococci, streptococci, anaerobes);
- autoimmune;
- parasitic;
- ossifying (develops after injuries - bruises, sprains);
- intercostal (characterized by predominant damage to the intercostal muscles).
Treatment
- corticosteroids;
- immunosuppressants (methotrexate, azathioprine, mycophenolate mofetil, rituximab, tacrolimus)
- intravenous immunoglobulin;
- gentle motor mode (until inflammation subsides).
In acute illness, glucocorticoids (prednisone) are the treatment of choice for initiating therapy. For severe illness with dysphagia or respiratory muscle weakness, pulse corticosteroid therapy (methylprednisolone) is indicated. A decrease or normalization of enzyme levels is observed after 6–12 weeks, after which the dose of prednisone is gradually reduced. At the same time, to minimize the effects of corticosteroids, a second (non-steroidal) drug (methotrexate, tacrolimus or azathioprine) is prescribed.
Causes of thoracic myositis
The skeletal muscles of the human chest are constantly in action, even when other muscle groups are resting - after all, we breathe continuously. Under unfavorable conditions, the muscles of the thoracic region are susceptible to inflammation - thoracic myositis. Let's call these conditions:
- previous diseases (viral, infectious), metabolic problems;
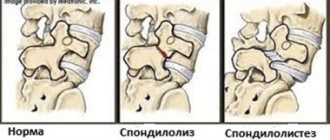
- pathologies of the thoracic spine;
- cold, damp, drafts;
- long-term preservation of anatomically incorrect posture;
- overwork of the pectoral muscles;
- injuries;
- local infection.
The risk group includes people engaged in sedentary work, as well as heavy physical labor.
Questions for the doctor
Specialist in the treatment of myositis
Which doctor treats myositis? From time to time I am bothered by vague chest pains, I would like to undergo a full examination.
Hello! If acute myositis develops, it is most logical to contact your local physician. The doctor will issue a certificate of temporary incapacity for work for the entire period of active inflammation, draw up a diagnostic plan (perhaps it will include consultations with specialized specialists) and treatment.
After the acute stage of the disease subsides, its causes should be understood. Here you may need to be examined by an infectious disease specialist, immunologist, endocrinologist, parasitologist, rheumatologist, neurologist, traumatologist, vertebrologist and other doctors.
Diagnostics
In diagnosing the disease, the first place is taken by:
- Collection of complaints and medical history. The specialist should find out what exactly is bothering the patient, whether he associates the appearance of negative symptoms with anything, and whether he has received treatment.
- Clinical examination. During examination and palpation, it is possible to identify tension in muscle fibers and the presence of individual seals.
- Laboratory tests. Markers of inflammation (leukocytosis, acceleration of ESR) appear in the CBC, and in the biochemical analysis there are signs of increased activity of muscle tissue enzymes.
- Instrumental tests (electromyography, CT).
- Biopsy with histological and cytological examination.
Examination and palpation will allow you to make a preliminary diagnosis