Spondylolisthesis (spon + dee + lo + lis + thee + sis) is a spinal pathology in which one of the vertebrae slips forward or backward in relation to the adjacent vertebra. Slipping of the upper vertebra forward relative to the underlying one is called anterolisthesis, and slipping backward is called retrolisthesis.
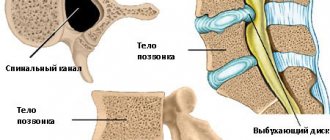
Spondylolisthesis (vertebral displacement) can lead to spinal deformity, as well as narrowing of the spinal canal (central spinal stenosis) or compression of the exiting nerve roots (foraminal stenosis).
Spondylolisthesis most often occurs in the lower back (lumbar spine), but can also occur in the thoracic and cervical regions. Treatment for vertebral displacement will depend on the degree of disruption of the biomechanics of the spine and the effect on nearby nerve structures and can be either conservative or surgical.
Causes of spondylolisthesis (vertebral displacement)
Spondylolisthesis has several main causes. Doctors have developed a classification system based on the different causes of spondylolisthesis.
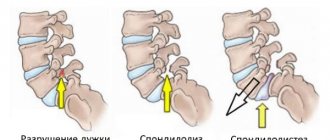
Type I: It is also called dysplastic or congenital spondylolisthesis. Thus, type I spondylolisthesis is a defect of the articular processes of the vertebra. This defect usually occurs at the junction of the lumbar spine and the sacrum: area L5-S1. The defect causes the L5 vertebra to slip forward relative to the sacrum.
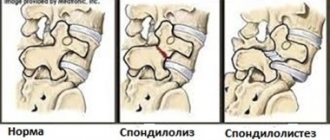
Type II: Also called isthmic, this is the most common type of spondylolisthesis. In type II spondylolisthesis, there is a problem with the pars interarticularis, a specific area of the vertebra. . Isthmic spondylolisthesis is further divided into subtypes:
- Type II A: Gymnasts, weightlifters and football players are especially susceptible to this type of spondylolisthesis. This type of vertebral displacement is caused by multiple microdestructions in the pars interarticularis area, which arise due to hyperextension and excessive loads. The vertebral arches in type II A are completely broken.
- Type II B: This type is also caused by microfractures. The difference, however, is that the arms do not break completely. Instead, bone tissue grows and the arches become longer as they regenerate. Longer arches may force the vertebra to move forward.
- Type II C: Like Type II A, this type has a complete fracture and is caused by acute trauma. For example, an impact from a car accident can destroy the temples.
A fracture of the arch can lead to the appearance of a moving part of the bone; the disconnected inferior articular process may move. This bone fragment, also called a Gill fragment, can impinge on a nerve root and often requires surgical removal of the bone fragment.
Problems with the pars interarticularis can also be called spondylolysis. The word is similar to spondylolisthesis, and the two are somewhat related. Microdestructions in the pars interarticularis - often occur in gymnasts, football players and weightlifters - are a form of spondylolysis. Fractures of the arches are called spondylolysis; If a vertebra slips forward because it is not held in place properly, it is called spondylolisthesis.
Type III: Aging can also cause spondylolisthesis. As a person ages, degeneration of the spinal structures occurs. Usually, the intervertebral discs degrade first. The older a person is, the less water and proteoglycans there are in the discs - and this leads to a decrease in the shock-absorbing functions of the discs. The discs become thinner and the load on the facet joints increases. The joints become hypermobile and the vertebra can end up sliding forward because the facet joints cannot effectively hold the vertebra in place. Typical degenerative spondylolisthesis usually develops in the L4-L5 region and is more common in women over 50 years of age.
Type IV: Similar to Type II C, Type IV involves a fracture. However, it is a fracture of any other part of the vertebra other than the pars interarticularis. For example, the facet joints may collapse, separating the front part of the vertebra from the back part.
Type V: Tumors in the spine can also cause spondylolisthesis because they weaken the bones and can cause fractures that separate the vertebrae, leading to instability and potential slippage.
Type VI: develops after surgical treatment of the spine. It is also known as iatrogenic spondylolisthesis, and is usually associated with postoperative instability of the spinal motion segments.
Why do disks become misaligned?
One of the factors of this problem may be deformation of the vertebral discs, when the nucleus pulposus falls out of the space between the vertebrae and creates compression on the nerve endings.
Displacement of the intervertebral structure occurs for several reasons:
- degeneration processes in the tissues of cartilage, fibrous ring and vertebral bones;
- sudden, inaccurate movements, when lifting heavy objects, awkward bends;
- weakened muscles due to physical inactivity, metabolic failure and deficiency of vitamins and microelements;
- age-related changes leading to shrinkage of the fibrous ring and curvature of the spine;
- presence of a cyst or tumor;
- as a result of injury, shock or inflammation.
Symptoms of spondylolisthesis
Symptoms of spondylolisthesis with minor mechanical disturbance of the location of the vertebra may be limited to discomfort after physical activity.
As the vertebra moves, conditions arise for a compression effect on the spinal cord (with anterolisthesis) and on the nerve roots (retrolisthesis). Mechanical impact on nerve structures can lead to symptoms of compression of the spinal cord or roots.
With severe compression of the spinal cord, serious complications such as cauda equina syndrome may occur, which requires emergency surgical intervention.
Most often, the following symptoms appear with spondylolisthesis:
- Pain in the lower back (neck) increases when turning or bending
- Pain in arms or legs
- Pain that runs down the back of the leg, pain in the buttocks
- Weakness in legs, arms
- Tingling or numbness in the extremities
- Muscle discomfort
- Muscle spasms
- Difficulty walking
- Bladder and bowel dysfunction (cauda equina syndrome)
Why is a slipped disc in the lower back dangerous?
Displacement of the lumbar vertebrae is a dangerous condition, which in severe cases can lead to paralysis of the lower limbs and disruption of the internal organs of the abdominal cavity and pelvis.
Inside the spinal column is the spinal canal. This is the receptacle for the spinal cord, the central part of the autonomic nervous system that controls the functions of the entire human body. When the spinal cord is damaged, innervation occurs. This can cause intestinal paralysis, impaired urine output, and paresis of the muscles of the lower extremities. But most often, slipped discs in the lower back do not lead to such catastrophic consequences. And this is even worse for the patient's health.
For example, if a serious disc displacement occurs with paresis of the lower extremities, then medical assistance will be provided in a timely manner, the patient will be forced to seek it. If the displacement is insignificant, then the clinical manifestations may be quite “tolerable”. In this situation, patients do not seek help for months. Meanwhile, they experience serious pathological changes against the background of spinal cord ischemia. The process of gradual degeneration of the nerve fiber begins. This will lead to unpredictable consequences in the future. Total disturbances of innervation may occur, and disruption of the functioning of all internal organs of the abdominal cavity is observed. The most serious and common complication is a violation of the tone of the vascular bed of the lower extremities and the pelvic cavity.
In men, such displacement of the vertebral disc in the lower back often leads to erectile dysfunction, impotence, the development of atherosclerosis and obliterating endarteritis of the lower extremities. In women, such a pathology can provoke the formation of hemorrhoids in the anus, the development of varicose veins of the lower extremities, and prolapse of the internal pelvic organs.
Diagnosis of vertebral displacement
As a rule, it is impossible to obtain visual signs of spondylolisthesis (vertebral displacement) based on the examination of the patient.
Patients usually complain of back pain and occasional pain in the legs or arms. Misalignment of the vertebrae (spondylolisthesis) can often cause muscle spasms or stiffness in the harness tendons.
The diagnosis of vertebral displacement is easily made using simple radiographs. A lateral x-ray can clearly show the presence of slippage of one vertebra in relation to another.
Spondylolisthesis is measured as the percentage of displacement of a vertebra compared to the adjacent vertebra.
- Grade I is a displacement of up to 25%.
- Grade II ranges from 26% to 50%.
- Grade III ranges from 51% to 75%.
- Grade IV ranges from 76% to 100%.
- Grade V or spondyloptosis occurs when a vertebra has completely fallen out of the underlying vertebra.
If the patient complains of pain, numbness, tingling or weakness in the legs, the doctor may order additional tests. These symptoms may be caused by stenosis or narrowing of the foramina and compression of the nerve roots. A CT scan or MRI may help identify nerve compression associated with vertebral misalignment. Sometimes a PET scan can help determine whether the bone at the defect site is active. This may help in choosing treatment tactics.
Cervical disc replacement (prosthetics)
Natural segments of the upper section have the smallest shapes and are characterized by greater mobility, this is how nature designed our spine for its harmonious work. Therefore, the cervical disc analogue is smaller in size and has a higher mobility potential than the lumbar disc. In the cervical spine, replacement of the intervertebral component is performed through an anterior cervical approach. Indications, contraindications, anesthetic management, intraoperative monitoring are similar to prosthetics of lumbar structures. We will describe the main technical aspects of the surgical procedure for implantation of cervical endoprostheses.
X-ray after surgery.
- The surgeon carefully cuts vertically through the soft tissue from the front of the neck. The length of the incision is 3.5-5 cm.
- Important neck structures are very carefully moved to the side. We remind you that the doctor performs all actions using powerful optical and x-ray equipment, namely, a microscope with multiple magnification (up to 50 times) and a tomography machine.
- The approach to the vertebrae and disc is cleared, the wound is fixed with a microsurgical retractor. Now the problematic C-disc is completely removed using microdiscectomy.
- After a total discectomy has been performed, the vertebral bones are prepared for installation of the implant system.
- An implant is attached to the space freed from cartilage tissue on the prepared edges of the vertebrae. The implanted product is checked for quality of fixation and functionality.
- At the final stage, the wound is closed with surgical sutures using subcutaneous suture technology. When the wound heals, the scar from the operation will be barely noticeable.
The patient should be activated as soon as possible - a few hours later on the same day or the next day. Since the manipulations were carried out in the neck area, it will be necessary to follow a special diet; on the first day the patient only drinks, then includes pureed, thin meals.
Immediately after surgery.
Treatment of vertebral displacement
- Initial treatment for spondylolisthesis (displacement of the vertebrae) is conservative and based on symptoms.
- A short period of rest or avoidance of activities such as heavy lifting, bending, and athletics may help reduce symptoms.
- Physical therapy can help increase range of motion in the lumbar or cervical spine, relieve muscle spasms, and strengthen core muscles.
A physical therapy program is one of the most effective treatments for spondylolisthesis for two main reasons: (1) It can help strengthen the muscles that support the spine, and (2) it can teach the patient how to maintain spinal function and prevent further progression of vertebral misalignment.
Physical therapy includes both passive and active treatment methods.
- Passive treatments help relax the body. They are called passive because the patient does not actively participate. A physical therapy program may begin with passive treatment to allow the body to heal, especially if the patient has pars interarticularis fractures.
- But the main goal of physical therapy is active treatment. These are therapeutic exercises that strengthen the body and help prevent the recurrence of possible pain associated with a misaligned vertebra.
Passive treatment
The doctor may prescribe passive procedures such as:
- Deep tissue massage: This method aims to relieve spasm and chronic muscle tension that occurs due to the body's adaptation to biomechanical disorders associated with vertebral misalignment.
- Hot and cold therapy: alternating hot and cold therapy. By using heat, blood flow can be achieved to a specific area and the increased blood flow brings more oxygen and nutrients to that area. Blood is also needed to remove the byproducts created by muscle spasms and also aids in healing.
- Cold therapy, also called cryotherapy, slows blood circulation and helps reduce inflammation, muscle spasms and pain. Ice packs can be used for cryotherapy, but currently a special physiotherapeutic hardware technique called cryotherapy is used to cool tissues.
- TENS (transcutaneous electrical nerve stimulation): TENS helps reduce muscle spasms and it can also increase the production of endorphins, natural pain relievers.
- Ultrasound: By increasing blood circulation, ultrasound helps reduce muscle spasms, swelling, stiffness and pain. The sound waves penetrate deep into muscle tissue, creating heat that enhances circulation and healing.
Active treatments
In the active portion of physical therapy, the physical therapy therapist will teach the patient various exercises to improve flexibility, strength, stability of the spinal column and restore range of motion. The physical exercise program (physical therapy) is individualized, taking into account health and medical history. Exercises for one person may not be suitable for another person with spondylolisthesis. Thus, the exercise therapy doctor selects an individual exercise program for each patient and the task of the set of exercises is to create a muscle corset that will compensate for biomechanical disorders associated with vertebral displacement.
If necessary, the patient receives information from a physical therapy doctor on how to correct his posture and incorporate ergonomic principles into daily activities. This is all part of the physical self-care or self-medication aspect: through physical therapy, the patient learns good habits and principles to better care for the body.
Types of displacements and their causes
A displaced vertebra can change position relative to the adjacent one or remain in the same state. The first option is typical for unstable displacement. The vertebra can slide sideways or forward. With a stable displacement, the displaced vertebra does not move.
Displacement in the lower back can be caused by various factors:
- Arch defects and congenital disorders of the spine.
- Injuries, overuse, grueling training.
- Scoliosis.
- Tumors, arthrosis.
- Sedentary lifestyle.
Intervertebral discs often become displaced precisely after herbs or heavy physical labor. Pathology is a frequent companion of professional athletes. Spondylolisthesis occurs more often in men.
Surgical treatment of vertebral displacement (spondylolisthesis)
Surgical treatment may be recommended if there is severe displacement of the vertebra or there is no effect of conservative treatment.
The type of surgery depends on the type of spondylolisthesis. Patients with isthmic spondylolisthesis may undergo surgical reconstruction of the defective part of the vertebra. If an MRI scan or PET scan shows that the bone is active at the site of the defect, then it will be restored when the arches are reconstructed. This surgery involves removing any scar tissue from the defect and placing a bone graft in the area, followed by screw fixation.
If there are signs of compression of nerve structures, surgery may include decompression to create more space for the nerve roots to exit the spine. Decompression is often combined with vertebral fusion, which can be performed either with or without screws. In some cases, the vertebrae are returned to their normal position before fusion is performed, and in other cases, only fusion can correct the misalignment of the vertebra. Outcomes and recovery after surgery depend on a comprehensive rehabilitation program.
Symptoms of lumbar spinal disc displacement
The first symptoms of lumbar disc displacement can be noticed when their physiological position is disrupted. This may be a sharp pain, a feeling of stiffness, or the inability to make one or another movement. Most often, the pathology is provoked by an awkward movement, for example, turning the body. Displacement is possible when trying to lift an unusually heavy load.
Subsequently, clinical symptoms of lumbar spinal disc displacement are divided into inflammatory, compensatory and neurological. Compensatory signs include excessive muscle tension in the affected area. Inflammatory processes include redness of the skin, local increase in temperature and swelling of the subcutaneous tissue.
When displacement occurs, neurological manifestations often come to the fore:
- numbness of certain areas of the lower back, buttocks, thighs and legs (depending on the degree of compression and the segment of compression in the dura mater of the spinal cord);
- the appearance of paresthesia (tingling, crawling sensation, itching);
- decreased muscle strength in the lower extremities;
- rapid leg fatigue during habitual physical activity;
- change in skin color (pallor due to impaired vascular tone);
- reduction in muscle mass and atrophy, which affects the appearance of the lower limb;
- constant feeling of cold in the affected area;
- disruption of urination and bowel movements.
If such clinical symptoms appear, you should immediately consult a neurologist or vertebrologist. He will conduct an examination and order an x-ray examination. Only indirect signs will be visible in the picture. An MRI is required to establish an accurate diagnosis. During this study, the doctor will be able to assess the position of the intervertebral discs, their condition and the degree of compression of the hard membranes of the spinal cord.
Complications and prognosis of spondylolisthesis
Complications of a misaligned vertebrae (spondylolisthesis) include chronic pain in the lower back or legs, and numbness, tingling, or weakness in the legs. Severe nerve compression can cause problems with bowel or bladder control, but this complication is very rare.
The prognosis for patients with spondylolisthesis is good. Most patients respond well to conservative treatment.
If severe symptoms are present, surgery may help relieve symptoms by decompressing nerve structures.
Complications of the disease
As a result of displacement of the vertebrae, compression of the intervertebral disc occurs, followed by its complete destruction, the appearance of an intervertebral hernia and pinched nerves.
In the last stages of the disease, the spinal cord with the nerve roots extending from it is included in the pathological process, resulting in unbearable pain. Depending on the location of the displacement, disturbances in the functioning of other organs are observed.
- Advanced displacement in the cervical spine is a path to hypertension, amnesia, blindness, deafness, neuralgia, progression of ENT diseases, and malfunction of the thyroid gland.
- With spondylolisthesis of the lumbosacral spine, treatment will require the pelvic organs (one of the causes of infertility), the genitourinary system, and the intestines.
- When the thoracic vertebrae are displaced, asthma develops, chronic bronchitis and pneumonia worsen. Pathologies begin in the work of the heart muscle and digestion, ulcers, gastritis, pancreatitis, duodenitis and pyelonephritis develop.