What do you need to know about grade 1 lumbosacral osteochondrosis?
Osteochondrosis of the 1st degree of the lumbar region is usually characterized as minor damage to the intervertebral discs with the appearance of a small amount of connective tissue between the vertebrae. This is the beginning of degenerative processes that are progressive in nature. Osteochondrosis of the lumbar region in itself is a serious disease, but in grade 1 it responds better to conservative therapy. The transition of the disease from the first to the second degree begins approximately a month after the first symptoms appear, so if you suspect osteochondrosis, you should consult a doctor immediately.
Symptoms of osteochondrosis
With the gradual destruction of intervertebral discs, the nerve roots of the spine may be compressed, which can cause various symptoms.
2.1. Pain in the lumbar region
With lumbar osteochondrosis of the 1st degree, changes in the spine are insignificant, so the pain is aching and not intense. Pain may occur during rotational movements of the body, lifting heavy objects, or accompany the patient constantly.
2.2. Tightness in the lumbar joint, a crunching sound is heard
Stiffness and tightness of the lumbar joint, a characteristic crunch when moving - these are typical manifestations of osteochondrosis of the lumbar spine of the 1st degree, which cannot be ignored.
2.3. Possible lumbago that radiates to the leg
A lumbago is a short-term sharp pain that usually occurs when moving. With osteochondrosis of the lumbar spine of 1st degree, this symptom does not always occur, but is often the reason for seeking medical help.
Osteochondrosis of the cervical spine
The cervical region is distinguished by the following features:
- this is the only part of the spine where there is not an intervertebral disc everywhere between the vertebrae: it is absent between the 1st vertebra and the back of the head, as well as between the 1st and 2nd cervical vertebrae;
- the lateral parts of the underlying vertebrae cover the overlying vertebrae from the sides: it turns out that the latter seem to be sitting in a “saddle”;
- The edges of the cervical vertebral bodies are elongated and slightly resemble a hook pointing upward, which is why they are called “hooked.” Such a “hook” and the area of the overlying vertebra do not just touch: between them there is the same joint as in the limbs: on top the articulating surfaces are covered with articular cartilage, and the articular capsule wraps the joint. These joints allow you to perform additional movements unique to this department - bending and rotation. But they “carry” additional problems - they can develop arthrosis (thinning of articular cartilage). And this is where osteophytes are formed. This is dangerous: osteophytes can compress nerve fibers or blood vessels passing in these sections.
With the development of osteochondrosis in the cervical region, when the intervertebral discs become thinner and the vertebrae themselves seem to sag, the nutrition of the joint between the “hook” of the underlying vertebra and the area of the body of the overlying vertebra is disrupted. In this case, arthrosis of this joint becomes a complication of osteochondrosis.
All types of movements are possible in the cervical spinal segment:
- extension and flexion;
- bending to the sides;
- turns,
Moreover, the volume of these movements is quite large. This represents a danger in terms of the development of osteochondrosis, characteristic only of the cervical spine.
The greatest mobility is observed in the joint between the 4th and 5th, as well as the 5th and 6th cervical vertebrae (10, 11). Osteochondrosis does not affect the articular surfaces between the 1st vertebra and the back of the head, as well as the articular cartilage between the 1st and 2nd vertebrae.
The following important structures pass through the cervical spine:
- on the lateral surfaces of all cervical vertebrae, in their transverse processes, there are openings so that the vertebral artery passes here, carrying blood to the brain;
- inside the first cervical vertebra (it is very different from “ordinary” cervical vertebrae) the transition of the brain stem to the spinal cord occurs;
- Below the 1st cervical vertebra, the first cervical roots of the spinal nerves begin to emerge from the spinal cord. Next, between the two vertebrae (upper and lower) one pair of spinal nerves emerges (between vertebrae 1 and 2, 1 pair of nerves emerges, between 2 and 3 – the second, and so on). The first three of them go to the neck and its organs (thyroid gland, pharynx, larynx, trachea), partially to the eyes and ears. The fourth pair of spinal nerves goes to the main respiratory muscle - the diaphragm; the fifth to seventh pairs innervate (provide nerve signals) to the arms.
With osteochondrosis and its next stage - intervertebral disc herniation, any of these structures can be infringed. These are very life-threatening conditions. But most often, osteochondrosis develops in the lower cervical regions, pinching either the 5th, 6th, or 7th root of the spinal nerve, which is why sensitivity (tactile, temperature, vibration) and mobility of one of the arms is impaired, and pain occurs in it (with that sides where the intervertebral foramen has narrowed).
Causes of the disease
Osteochondrosis of the lumbar spine is a common ailment, but grade 1 is less common in medical practice than others due to late patients seeking help. It is worth knowing that various factors contribute to the development of the disease.
3.1. Severe physical strain, heavy lifting
Excessive stress on the spine provokes tension and swelling of the muscles that nourish the cartilage of the intervertebral discs. Systematic loads provoke degenerative processes in the spine.
3.2. Excess body weight
Excess weight is another serious factor that provokes stress on the lumbar spine and subsequently grade 1 osteochondrosis, which quickly develops.
3.3. Low physical activity
With a sedentary lifestyle, the spinal muscles atrophy and cease to perform their function - maintaining the spine in the correct position. This causes destruction of the spinal discs.
3.4. Poor posture
In case of poor posture, grade 1 lumbar spine osteochondrosis can occur under the influence of many factors: mechanical damage to the discs due to displacement of the vertebrae, atrophy of the vertebral muscles.
Diagnostics
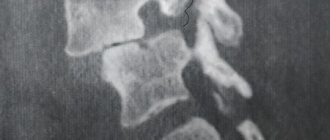
Osteochondrosis of the lumbar spine of the 1st degree can be detected using the following diagnostic methods: x-ray:
- identifies the location of damage and the location of pinched nerve root;
- blood test for biochemistry: allows you to identify a lack of microelements, which is often the cause of osteochondrosis.
MRI or CT may be prescribed as an additional research method. It is strictly not recommended to make a diagnosis on your own and self-medicate, since grade 1 osteochondrosis of the lumbar spine is easily disguised as other diseases.
Forecast
Osteochondrosis of the cervical spine of the first degree can be eliminated with timely treatment . It should be treated necessarily, since when it progresses to more serious stages, the disease can provoke the development of radicular syndromes.
In addition, the development of osteochondrosis may have other complications : hernias and protusions, impaired cardiovascular activity (development of hypotension or hypertension). All diseases lead to complicated symptoms and disruption of other body systems.
Treatment of osteochondrosis at the first stage completely eliminates the symptoms of the disease and optimizes the normal activity of the musculoskeletal system of the cervical spine.
Treatment
Treatment of the disease must be comprehensive - it is prescribed after a final diagnosis and additional research. For grade 1 lumbar osteochondrosis, conservative methods are sufficient.
5.1. Drug therapy
Drug treatment of osteochondrosis is aimed at eliminating symptoms. For osteochondrosis of the lumbar spine of the first degree, the following groups of drugs can be prescribed:
- anti-inflammatory drugs – relieve inflammation, swelling and pain;
- chondoprotectors – normalize metabolism and strengthen intervertebral discs;
- ointments – have a local anti-inflammatory and analgesic effect.
For grade 1 osteochondrosis of the lumbar spine, it is recommended to combine these methods with injections, including to block pain in the acute period of the disease.
5.2. Massage
For osteochondrosis of the lumbar spine, massage must be done carefully and with the consent of a neurologist
, this also applies to stage 1 of the disease. The main function of massage is to restore blood supply to muscles and their elasticity, and relieve pain.
5.3. Physiotherapy
For grade 1 lumbar osteochondrosis, physiotherapeutic procedures give positive results. They relax muscles and reduce inflammation by improving blood flow in the body. Only a doctor can prescribe physical therapy as a treatment method.
5.4. Physiotherapy
It is the main method of treating the disease, as it can bring good results. Strengthens the muscle corset and restores its functions, improves blood circulation and joint condition. Osteochondrosis of the 1st degree of the lumbar region is the stage of the disease at which exercise therapy gives the best results. However, exercise therapy will be effective provided that the exercises are performed regularly.
5.5. Traditional methods of treatment
Traditional methods are used when it is necessary to relieve symptoms; they are not excluded as an auxiliary treatment. However, they cannot replace qualified medical care. For grade 1 osteochondrosis, traditional methods involve applying compresses to the lumbar back.
Massage
Quite a useful procedure for this disease. The most important thing is to contact an experienced specialist who has an idea of how to work with first-degree osteochondrosis.
The duration of the course is at least 10 sessions.
The massage should be measured and calm. Excessive pressure on the affected area must be avoided.
The purpose of the massage is to normalize blood circulation and nutrition of the brain, reduce muscle spasm and improve the patient’s condition.
Massage is not for everyone; there are contraindications:
- Presence of tumors;
- Diseases of the cardiovascular system;
- Osteomyelitis;
- Women during pregnancy.
It is quite possible to relieve spasms and strengthen muscles at home. Professional massagers are specially designed for this purpose.
Gymnastics for a cervical hernia on the Drevmass simulator is quite effective, look at the video: “cervical osteochondrosis - self-massage of the neck.”
Disease prevention
If therapy is prescribed correctly, then pain and lumbago with osteochondrosis of the lumbar spine of the 1st degree disappear quickly. However, if you do not take care of prevention to restore the body, the disease may return. To prevent this from happening, you should follow the following recommendations:
- proper nutrition: the daily diet should contain enough vitamins and microelements to prevent degenerative processes in the intervertebral space;
- comfortable conditions: the workplace and bed should be comfortable so that the back muscles relax;
- control over weight and physical activity: will reduce the risk of osteochondrosis;
- active lifestyle: physical exercise strengthens muscles and relieves tone, therefore has a beneficial effect on the condition of the spine.
You need to understand that preventing grade 1 osteochondrosis of the lumbar spine is much easier than treating it.
Exercise therapy
Therapeutic exercise is an integral component in the complex treatment of the disease. With its help, muscles warm up, blood circulation improves and tissue nutrition is normalized.
Classes can be performed at home, a warm-up is carried out beforehand.
Exercises should be performed at a calm pace.
If pain occurs, stop exercising.
Exercises for first degree osteochondrosis:
Important! You can perform exercises only on the recommendation of a doctor and in the absence of pain.