Osteocondritis of the spine
Osteochondrosis of the spine is divided into several types. This:
- Osteochondrosis of the cervical spine.
- Osteochondrosis of the thoracic region.
- Lumbar osteochondrosis.
- Osteochondrosis of the sacral region.
Most often, lumbar and sacral osteochondrosis are considered as a single disease - osteochondrosis of the lumbosacral spine. This is due to the structural features of these areas of the back (we will look at this in the relevant sections).
In some cases, osteochondrosis of the coccyx may develop when the articular cartilage between the sacrum (in adults, these are 5 fused vertebrae) and the coccyx (it consists of 3-5 vertebrae) is affected. This disease most often occurs in women after spontaneous childbirth (especially when the mother has a narrow pelvis or the fetal weight is more than 4 kg), but can develop with injuries, operations and malformations of this part of the spine. Due to the structural features of the sacrococcygeal joint (the absence of a nucleus pulposus - a central shock-absorbing area that exists between the vertebrae of the cervical, thoracic and lumbar regions), damage to the articular cartilage in it is more correctly called arthrosis of the sacrococcygeal joint than osteochondrosis.
Osteochondrosis can also develop in more than one part of the spine. When such a process develops in more than two, it is called widespread.
The symptoms of each type of disease are discussed in detail in the article “Symptoms and signs of osteochondrosis.”
A little more about terminology. Scientists (4) believe that the phrase “intervertebral osteochondrosis” is unacceptable. Firstly, as a result of this process, both the vertebral bodies are affected (this is displayed in the prefix “osteo-”), and articular cartilage - the endplates of the vertebral bodies (“-chondrosis”). That is, not only the intervertebral discs suffer, but also the structures surrounding them. Therefore, it would be correct to say “osteochondrosis of the spine,” and not in any other way.
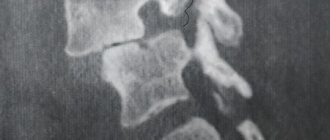
Diagnostic features
Only a specialist can make a diagnosis after a thorough examination.
It is important to remember that the symptoms of a degenerative-dystrophic disease are nonspecific, which implies the need to consult a doctor who can rule out the presence of other ailments, in particular various neoplasms that can provoke similar symptoms.
In order to determine the localization of the pathology, an x-ray examination is prescribed. Clarification and confirmation of the presumptive diagnosis is carried out using magnetic resonance imaging, which provides high-quality images of each layer of the spinal column.
A wide range of nonspecific symptoms often leads to a false diagnosis and, as a consequence, incorrect treatment of lumbar osteochondrosis. Based on this, we can come to the conclusion that it is important to carry out a comprehensive diagnosis by visiting different specialists, including: vertebrologist, neurologist, nephrourologist, gastroenterologist and surgeon.
Osteochondrosis of the cervical spine
The cervical region is distinguished by the following features:
- this is the only part of the spine where there is not an intervertebral disc everywhere between the vertebrae: it is absent between the 1st vertebra and the back of the head, as well as between the 1st and 2nd cervical vertebrae;
- the lateral parts of the underlying vertebrae cover the overlying vertebrae from the sides: it turns out that the latter seem to be sitting in a “saddle”;
- The edges of the cervical vertebral bodies are elongated and slightly resemble a hook pointing upward, which is why they are called “hooked.” Such a “hook” and the area of the overlying vertebra do not just touch: between them there is the same joint as in the limbs: on top the articulating surfaces are covered with articular cartilage, and the articular capsule wraps the joint. These joints allow you to perform additional movements unique to this department - bending and rotation. But they “carry” additional problems - they can develop arthrosis (thinning of articular cartilage). And this is where osteophytes are formed. This is dangerous: osteophytes can compress nerve fibers or blood vessels passing in these sections.
With the development of osteochondrosis in the cervical region, when the intervertebral discs become thinner and the vertebrae themselves seem to sag, the nutrition of the joint between the “hook” of the underlying vertebra and the area of the body of the overlying vertebra is disrupted. In this case, arthrosis of this joint becomes a complication of osteochondrosis.
All types of movements are possible in the cervical spinal segment:
- extension and flexion;
- bending to the sides;
- turns,
Moreover, the volume of these movements is quite large. This represents a danger in terms of the development of osteochondrosis, characteristic only of the cervical spine.
The greatest mobility is observed in the joint between the 4th and 5th, as well as the 5th and 6th cervical vertebrae (10, 11). Osteochondrosis does not affect the articular surfaces between the 1st vertebra and the back of the head, as well as the articular cartilage between the 1st and 2nd vertebrae.
The following important structures pass through the cervical spine:
- on the lateral surfaces of all cervical vertebrae, in their transverse processes, there are openings so that the vertebral artery passes here, carrying blood to the brain;
- inside the first cervical vertebra (it is very different from “ordinary” cervical vertebrae) the transition of the brain stem to the spinal cord occurs;
- Below the 1st cervical vertebra, the first cervical roots of the spinal nerves begin to emerge from the spinal cord. Next, between the two vertebrae (upper and lower) one pair of spinal nerves emerges (between vertebrae 1 and 2, 1 pair of nerves emerges, between 2 and 3 – the second, and so on). The first three of them go to the neck and its organs (thyroid gland, pharynx, larynx, trachea), partially to the eyes and ears. The fourth pair of spinal nerves goes to the main respiratory muscle - the diaphragm; the fifth to seventh pairs innervate (provide nerve signals) to the arms.
With osteochondrosis and its next stage - intervertebral disc herniation, any of these structures can be infringed. These are very life-threatening conditions. But most often, osteochondrosis develops in the lower cervical regions, pinching either the 5th, 6th, or 7th root of the spinal nerve, which is why sensitivity (tactile, temperature, vibration) and mobility of one of the arms is impaired, and pain occurs in it (with that sides where the intervertebral foramen has narrowed).
Rehabilitation and lifestyle restoration
The patient may be prescribed a special diet that will improve metabolic processes and help saturate the body with vitamins, nutrients and minerals. For osteochondrosis, it is recommended to eat in small portions, about 5-6 times a day. The diet of those suffering from osteochondrosis should include fermented milk and dairy products, lean meat, fish and poultry, as well as jellied meat, olive oil and jellied dishes.
You should limit your intake of flour and confectionery products, and also eat less salty and sweet foods. During the day, it is important to drink at least 1.5 liters of liquid: preferably water. You should drink less strong tea, coffee, carbonated and alcoholic drinks.
Osteochondrosis of the thoracic region
This form of osteochondrosis is quite rare. This is due to the small amount of mobility in the thoracic region.
Each of the thoracic vertebrae is connected not only to the vertebrae (above and below), but also to the ribs (each vertebra is connected to a pair of ribs). This provides stability to the thoracic region and limits the mobility of the spine.
The openings through which the spinal nerves exit are smaller than in other sections. There is already a canal through which the spinal cord passes. Therefore, its even greater narrowing with the growth of osteophytes (bone “spikes” from the vertebrae) can lead to a violation of the blood supply to the spinal cord (spinal stroke).
As part of the thoracic roots of the spinal nerves (there are 12 of them, like the vertebrae), a large number of nerves of the autonomic nervous system pass through. Therefore, when nerve fibers in the thoracic region are infringed, in addition to disrupting the functioning of the organs to which they go:
- from the root between the last cervical and first thoracic vertebrae, part of the nerve fibers goes to the eye (pupil, orbicularis oculi muscles);
- from the first two segments - to the hands;
- from the second and the remaining ten - to the organs of the thoracic cavity (heart, lungs, large vessels), to the organs of the abdominal cavity (liver, stomach) and retroperitoneal space (pancreas, kidneys) (1),
Symptoms of dysfunction of the autonomic nervous system will also appear: arrhythmias, anxiety or fear of cardiac arrest, sweating, a feeling of heat (the so-called “hot flashes”), pallor, increased breathing.
In addition, the fourth segment of the spinal cord, which is located at the level of the 2nd thoracic vertebra, is a critical area for the blood supply to this organ. If the diameter of the spinal canal decreases, a spinal stroke (death of part of the spinal cord) will develop here more quickly than if the spinal cord is pinched in other places.
Osteochondrosis rarely develops in the disc between the 1st and 2nd, as well as between the 2nd and 3rd vertebrae (5). More often it occurs in the area of 6-7 thoracic vertebrae, where there is maximum backward curvature of the spine (kyphosis).
Possible consequences
The most dangerous complication is considered to be a deterioration in blood supply to the brain , as the arteries passing through the neck are compressed. The person experiences dizziness and fainting.
The main consequences are considered:
- Vascular changes.
- Hernia formation.
- Development of osteophytes.
- The mobility of the spine is impaired.
With cervical osteochondrosis of the 3rd degree, hearing loss and visual impairment may occur . Hypertension and VSD often develop. An external defect also appears - the formation of withers.
Osteochondrosis of the lumbar spine
Osteochondrosis of the lumbar spine occurs in approximately 50% of cases (2). This is due to the large load on this part of the spine (it has to withstand the weight of the body), which increases even more when squats (muscular work plus a change in the center of gravity of the body), lifting weights, and some incorrect movements (as, for example, when playing football, when you have to catch the ball, performing muscular work, moving the center of gravity not to the center, but to the edge of the joint between two vertebrae).
In addition, the lumbar spine is very mobile and connects the sedentary thoracic spine and the immobile sacral spine.
Most often, damage to the intervertebral disc, from which osteochondrosis begins, corresponds to the gap between the 4th and 5th vertebrae (here the apex of lumbar lordosis is observed - the convexity of the spine), less often - between the 5th lumbar and 1st sacral vertebrae. These segments are the most overloaded (2). The discs between the 1st and 2nd, as well as the 2nd and 3rd vertebrae are less likely to suffer, as they have good mobility (5).
At the level of the arch of the 1st lumbar vertebra, the terminal section of the spinal cord begins, and at the level of the body of the 2nd vertebra, the cauda equina departs from this organ of the central nervous system - a bundle of the roots of the spinal nerves of the lumbar, sacral and coccygeal segments (13) together with the terminal filament of the spinal cord itself. And if the upper 3 vertebrae are well fixed by ligaments, and even their damage by osteochondrosis is rarely accompanied by compression of the spinal roots (5), then the development of the dystrophic process below this level will no longer be distinguished by this feature. In this case, cauda equina syndrome may develop (14): severe, burning pain in the back, spreading to the perineum and inner thighs, urinary and fecal incontinence, impaired potency, weakness of the leg muscles or complete inability to move them.
A person may have such a congenital anomaly when the first sacral vertebra is separated from the main mass of the sacrum and becomes as if lumbar (this is called lumbarization). In this case, there is “one more vertebra” chance for the development of osteochondrosis.
There is also a congenital anomaly when the spinal canal (in which the spinal cord passes) in the lumbar region has the shape of a trefoil (5). If this is combined with the fusion of the sacrum with the fifth and last lumbar vertebra (this is called sacralization), then the sacrum greatly limits the places where the roots of the spinal nerves exit. As soon as the last mobile (lumbar) vertebrae are displaced (for example, by the formation of osteophytes), the exiting spinal nerves are immediately pinched (5).
Osteochondrosis of the sacral region
Isolated osteochondrosis of the sacral region rarely develops. This is due to the fact that the vertebrae are fused here, and the entire load is forced to be distributed across the entire department at once. Osteochondrosis in the sacrum develops when the lumbar region is damaged (due to osteochondrosis, injury or other disease), and the fused five vertebrae have to withstand increased load.
In the absence of spinal abnormalities, in order to maintain balance with the pelvic bones located at an angle, the sacrum should be located at an angle of 30 degrees to the vertical axis of the body. But if the first sacral vertebra protrudes forward a little more than necessary (due to a congenital anomaly or injury), this will limit the space for the spinal nerve roots and blood vessels emerging from the 1st sacral segment. If this is combined with sacralization (accretion of the last lumbar vertebra to the first sacral one), then the places for the roots of the 2nd sacral segment will be narrowed. Then the osteochondrosis that has developed here (especially posterior osteophytes) and its complications (intervertebral hernia) will quickly make itself felt by pain syndrome localized in the perineum and inner thighs (5).
It should be noted that sacralization of the spine does not occur immediately after birth. The fusion of the last lumbar vertebra with the sacrum begins at 13-14 years of age and ends by 23-25 years of age (5). There are situations when the first sacral vertebra remains unfused throughout life, performing the function of the 6th lumbar vertebra. Such anomalies create more prerequisites for the development of osteochondrosis here (5), and are also often combined with non-closure (complete or partial) of the sacral canal - a curved tube in which the sacral nerves pass, exiting the spine through the sacral foramina.
Osteochondrosis of the cervical and thoracic spine
Osteochondrosis of the cervical and thoracic spine occurs when a person does not pay attention to the developed degenerative process in the discs between the lower cervical vertebrae. As a result, “circles in the water” begin to diverge from such a “stone”—the underlying (thoracic) spine begins to be involved in the process.
The situation when changes in the disc and the surrounding vertebrae affect segments of the cervical and thoracic region, lying far from each other, develops less frequently.
Osteochondrosis of the lumbar and sacral region
The entire sacrum and the last vertebra of the lumbar region are the basis of the entire spine - they provide its support and experience the maximum load. If additional loads are placed on it, especially if genetic, hormonal prerequisites for this develop or a person constantly experiences a deficiency of microvibration, osteochondrosis of the lumbosacral region develops (you can read more about this here: “Causes of osteochondrosis”).
The discs between the lumbar vertebrae are usually the first to suffer, then (according to the mechanism described in the previous section) the sacrum is involved in the process. Also, lumbosacral osteochondrosis is often called a condition when the joint between the last lumbar vertebra and the sacrum undergoes degenerative changes.
Prevention
In order not to encounter third-degree osteochondrosis, you should take care of prevention in advance.
Recommendations for preventing third degree osteochondrosis:
- Do not lift too heavy objects; increase the load when training in the gym under the supervision of a trainer.
- Avoid drafts, which can lead to the development of inflammatory processes.
- Maintain the correct body position when sitting - do not hunch, do not lean to one side, and do not cross your legs over each other.
- Lead as active a lifestyle as possible - osteochondrosis is increasingly being diagnosed in people suffering from physical inactivity. If you work in an office, take the time to do a little stretching at least once every few hours. Walk more, go swimming, train yourself to start every morning with exercise.
- Wear shoes that are as comfortable as possible. This is especially true for women who spend a lot of time in heels.
- Give up bad habits that negatively affect the condition of the musculoskeletal system.
- Create a comfortable place to sleep at night by choosing a mattress and pillow that is moderately firm.
- Watch your diet and weight - the diet of a person who cares about the health of his spine and wants to prevent the development of osteochondrosis must contain vitamins, calcium, protein and phosphorus. But don't overeat. Excess body weight creates increased stress on the spine, which accelerates the development of degenerative processes.
Widespread or polysegmental
The disease develops in 12% of cases of osteochondrosis (5). This is the most severe type of disease, when degenerative processes occur in several segments (a segment is two vertebrae, upper and lower, surrounding the intervertebral disc affected by the disease) of the spine. Both segments of one department can be affected (for example, osteochondrosis of the disc between the 4th and 5th and 6-7th cervical vertebrae) and unrelated segments of different departments. For example, osteochondrosis of the disc between the 4-5 cervical vertebrae (C4-C5) and the disc between the 4th and 5th lumbar vertebrae (L4-L5) may develop.
Symptoms of common osteochondrosis consist of those that are characteristic of each lesion individually.
If osteochondrosis of all parts of the spine develops, this is called generalized osteochondrosis. Usually it develops in people whose genes “dictate” to them a special structure of the musculoskeletal system and connective tissue, and against this background the person overloads his spine.
Because with polysegmental osteochondrosis, it does not happen that an exacerbation develops simultaneously in all departments. Most often, exacerbation develops in one department, then in another. This led to the emergence of such a “everyday” diagnosis as wandering osteochondrosis. Official medicine does not recognize it and prescribes additional research for a person who has made such a “diagnosis” in order to understand the cause of his symptoms.
Youthful or juvenile
Juvenile osteochondrosis is a group of diseases that develop in children under 20 years of age. In this case, there is a violation of the blood supply in one or more cartilages located near the joints, from which bones develop (elongate) (these areas are called ossification centers).
Juvenile osteochondrosis is divided according to localization into osteochondrosis (9), which affects:
- brush;
- shoulder joint;
- tibia and fibula;
- radius and ulna bones;
- patella;
- metatarsus of the foot;
- hip joint;
- tarsus of the foot;
- hip and pelvis;
- femur (this is called Perthes disease).
- juvenile osteochondrosis after healing of congenital hip dislocation.
Juvenile spinal osteochondrosis is also called Scheuermann-Mau disease. It is based on a violation of the blood supply to the plates of cartilage that lines the vertebral body and is adjacent to the intervertebral disc. But not all of them suffer, but only some of the vertebrae. The severity of the disease depends on the angle at which the thoracic spine is concave, on the number of affected vertebrae, and the degree of their deformation. Most often it develops in boys, aged 11-18 years.
Stages (periods)
Modern literature describes spinal osteochondrosis as a chronic process prone to relapses. Developing at a young age (mainly as a result of injuries or improper movements, heavy lifting), it progresses at different rates, can slow down (remission of osteochondrosis occurs), or can proceed continuously. In old age, on the contrary, a slow course of the disease is observed.
Neurologists distinguish several stages (periods) depending on how much the intervertebral disc structures are changed:
- I period. Here, the amount of water in the nucleus pulposus, the shock-absorbing center of the intervertebral disc, decreases, and cracks appear in its fibrous ring. The nucleus pulposus is deformed and shifted to the posterior side (towards the posterior longitudinal ligament, which runs along the posterior surface of the vertebral bodies). This intradiscal movement of the nucleus pulposus causes irritation of the passing nerves (in the cervical region - sinuvertebral). This is manifested by minor pain in the neck or the corresponding part of the back, stiffness of movements, adoption of a special position in which some pain relief occurs. If osteochondrosis develops in the lumbar region, the lumbar lordosis is smoothed.
- The second period is characterized by the formation of subluxations and pathological mobility in the affected segment of the spine. This is due to the fact that the cartilage-like tissue of the disc (fibrous ring), which lies around the nucleus pulposus, begins to gradually dry out - the height of the disc decreases. Where the annulus fibrosus delaminates more, the nucleus pulposus rushes, helping to further disintegrate it (usually this happens towards the weaker posterior longitudinal ligament). This period of osteochondrosis is manifested by pain at the level of the affected segment; the muscles above and below the segment are constantly tense, trying to hold the vertebrae so as not to damage the spinal cord.
- III period is characterized by a complete rupture of the fibrous ring, so the nucleus pulposus moves through it and protrudes between the vertebrae (an intervertebral hernia is formed). The nucleus pulposus may even prolapse into the lumen of the spinal canal (disc sequestration). The cartilage covering the vertebrae becomes thinner due to the fact that the layer between them becomes smaller. Symptoms of the stage depend on which direction the intervertebral disc is displaced:
- if in the direction of the hole through which the spinal root exits, pain is felt that spreads along the nerve fibers (that is, if osteochondrosis develops in the lower cervical or upper thoracic segments, they will be felt in the arm, and if in the lumbar, then in the leg ), the sensitivity of innervated organs suffers;
- if towards the spinal canal along the midline, back pain becomes constant, mobility and sensitivity of the limbs are impaired, the function of internal organs receiving innervation from the affected segment suffers,
- if the nucleus pulposus penetrates the vertebra located above or below, the disease will be asymptomatic;
- IV period. The tissue of the affected intervertebral discs is replaced by scar tissue, due to which mobility in this spinal segment is limited or lost. In neighboring segments, the vertebrae are forced to shift, and inflammation and arthrosis develop between their processes. Osteophytes - bone outgrowths - begin to appear from the bones. The longitudinal ligament may ossify. The edges of the vertebrae deformed by osteophytes and the ossified ligaments next to them form a kind of bone brackets. This is spondyloarthrosis.
In the domestic literature you can see another classification of osteochondrosis. She distinguishes between acute, subacute and remission.
the initial stage of osteochondrosis. In rare cases, pain periodically occurs in the affected area of the spine, which quickly passes.
When the muscles trying to stabilize the spine are involved in the process, a spasm occurs in them and local vessels are compressed. Because of this, swelling develops, which compresses the nerve roots. Pain occurs. This is an acute period of the disease. If treatment is started during this period - limiting physical activity in the damaged area, using painkillers (also known as anti-inflammatory drugs), then the attack of osteochondrosis will pass in 5-7 days. Subacute or 2nd period of the disease begins.
The subacute period lasts approximately 12-14 days. If at this stage you do not overcool, do not lift heavy objects, or make sudden movements, osteochondrosis goes into remission.
Exacerbation of osteochondrosis rarely develops “on its own” if a person takes care of replenishing the microvibration deficiency in the body (this is achieved through high physical activity and/or phonation procedures) and maintaining sufficient blood supply to the affected area.
Exacerbation of osteochondrosis can be caused by:
- hypothermia;
- lifting weights;
- severe stress;
- sudden movements;
- unprofessional massage;
- drinking alcohol;
- cold;
- sudden changes in heat and cold (for example, diving into cold water after a bath or sauna);
- frequent bending;
- long stay in a bent position.
Degrees of osteochondrosis
In its development, osteochondrosis goes through certain stages. These are called grades, and depending on the grade, the doctor plans treatment.
To understand how much the disease affects work, the ability to self-care, and the adequacy of a person, domestic neurologists distinguish 5 degrees of osteochondrosis:
| Degree | Severity of pain and other symptoms | Impairment of work capacity and performance |
| 1st degree | In the first degree, the pain is insignificant, occurs during exercise, and disappears with rest. Only pain points can be detected. | Saved for any job |
| 2nd degree | The pain is not severe, it appears at rest, intensifies with exercise, but if you take a comfortable position or stop the exercise, the pain goes away. In the second degree, a change in the configuration of the spine is noticeable, tense muscles can be felt. Limited mobility of the spine | If we are talking about an employee of non-manual or light physical labor, the ability to work is preserved. If a person works hard, his ability to work is limited. A person is forced to take breaks from work and tries to avoid physical activity. |
| 3rd degree | The pain is more pronounced and intensifies with exercise. Neurological symptoms that impair work ability are identified. | Violated. Only knowledge workers can continue working. The ability to perform household activities is reduced, but self-care and the ability to move independently are preserved |
| 4th degree | In addition to severe pain, neurological symptoms also appear: dizziness, sensory disturbances | Lost for any work. Can move indoors only using crutches. Tries to move only when physiological needs need to be satisfied. |
| 5th degree | Pain and other symptoms are pronounced at rest. A person is forced to stay in bed. | Lost for any type of work. A person needs care. |
Osteochondrosis of the spine, no matter in what part it forms and no matter what degree it reaches, needs to be identified and prescribed adequate timely treatment. In this case, treatment should be comprehensive, and include not only taking medications to relieve symptoms, but also other (main) treatment methods aimed at eliminating the causes of the disease. Read more about treatment here: “Treatment of osteochondrosis at home.”
List of used literature:
- Neurology and neurosurgery / ed. A.N. Konovalova, A.V. Kozlova; E.I. Gusev, A.N. Konovalov, V.I. Skvortsova, textbook: vol. 1 – 2009
- Osteocondritis of the spine. V.A. Epifanov, A.V. Epifanov. – M, 2008
- Osteochondrosis. Yakushin M.A., Gilinskaya N.Yu., Yakushina T.N., Maratkanova T.V. Moscow Regional Research Clinical Institute. Almanac of Clinical Medicine, 2001, No. 4, Pages: 285-292.
- Clinical radiology. Guide in five volumes / ed. G.A. Zedgenidze. Volume 3. “X-ray diagnosis of injuries and diseases of bones and joints.
- Osteocondritis of the spine. Guide for doctors. N.M. Zhulev, Yu.D. Badzgaradze, S.N. Zhulev. – St. Petersburg, 1999
- Traumatology and orthopedics. Kornilov N.V.
- Orthopedics. National leadership. Mironov S.P., Kotelnikov G.P., 2008
- Traumatology and orthopedics. Kavalersky G.M.
- International Classification of Diseases, 10th Revision (ICD-10).
- Stenosis of the lumbar vertebral canal and sciatica. Verbiest H. Neurosurg Rev. 3: 75 - 89. 1988.
- Cervical osteochondrosis. Popelyansky Ya.Yu. M, 1966
- Wikipedia.
- Body resources – immunity, health, longevity. Vasiliev A.E., Kovelenov A.Yu., Kovlen D.V., Ryabchuk F.N., Fedorov V.A., St. Petersburg, 2004
Author of the article: doctor Krivega M.S. (Regional Infectious Diseases Clinical Hospital, Zaporozhye)
You can ask questions (below) on the topic of the article and we will try to answer them competently!
Probable causes
Among the probable causes of the pathology, it is customary to highlight:
- increased or insufficient load on the muscles due to non-physiological factors;
- violation of metabolic processes;
- suffered injuries, in particular not only acute, but also chronic microtrauma received in the process of playing sports;
- dysfunction of the musculoskeletal system;
- genetic predisposition to pathological processes occurring in bone and cartilage tissue;
- poor posture;
- lack of physical activity;
- features of human professional activity.
It is worth noting that uneven distribution of load along the spinal column can cause a deterioration in the quality of blood supply to the intervertebral discs, which sooner or later leads to their degeneration and final destruction.