Osteochondrosis is a dystrophic-degenerative disease of bone and cartilage tissue, which in most cases affects the vertebrae and intervertebral discs. Osteochondrosis of the sacral (lumbar) region causes significant discomfort to a person, negatively affecting not only the condition of the back, but also the lower extremities. It is impossible to delay treatment of osteochondrosis of the sacral region, since the pathological process will only progress, causing more pain. Treatment of osteochondrosis should be comprehensive and prescribed by a specialist.
At the Yusupov Hospital you can undergo a full course of treatment for osteochondrosis, including rehabilitation to restore lost functions and improve overall well-being. The treatment of osteochondrosis is carried out by experienced neurologists together with physiotherapists, which allows achieving better results in the treatment of the disease.
How does osteochondrosis of the lumbar spine occur?
Since most of the body is supported by the pelvic bone, lumbar osteochondrosis is the most common of all types of osteochondrosis.
The spine consists of the main spongy bone tissue and the intervertebral discs connecting the sections of the ridge. They consist of cartilage tissue, inside of which there is a semi-liquid core. The purpose of the intervertebral discs is to act as hinges, allowing the spine to be flexible and bend in different directions.
Osteochondrosis affects the circulatory system, when it is disrupted, the cartilage tissue of the intervertebral discs loses its strength. The process of tissue degeneration begins, the cartilage dries out and becomes brittle, begins to sag and protrude from the spinal column, unable to withstand the constant load of body weight. The affected part of the ridge begins to gradually fold and put pressure on the adjacent nerves, causing severe pain radiating to the leg. This condition is called lumboischialgia. If left untreated, the patient risks significant consequences, including paralysis of the lower body.
Osteochondrosis of the sacral spine: symptoms and treatment
Osteochondrosis of the sacral (lumbar) spine is the most common form of this pathology. In this case, the intervertebral discs, articular cartilage and sacral vertebrae are affected. The disease causes severe pain in the lumbar region and leads to temporary disability.
Osteochondrosis is a chronic disease with periods of exacerbation. It is possible to completely eliminate osteochondrosis at the initial stage of the disease, with minor disorders. If a serious pathological process develops, it will take a lot of time to normalize the condition of the spine, and special drug treatment will help stop degenerative changes. Therefore, osteochondrosis must be treated immediately after the first signs appear.
The most characteristic signs of osteochondrosis of the sacral region include:
- pain in the lumbar region during movement or at rest;
- impaired mobility of the spine in the lumbar region;
- increased sensitivity of the affected area.
As the disease progresses, pain and discomfort spread to the buttocks and lower limbs. Infringement of the nerve roots of the spine disrupts the functioning of the peripheral nerve endings that are located in the lower part of the body. The patient experiences discomfort while walking, coughing, tingling and a sensation of “pins and needles” in the feet.
During the acute period, the patient suffers from severe pain with “lumbago”. The pain may be reflected in the buttocks and legs, making movement difficult. During this period, a person’s ability to work significantly deteriorates. In severe cases, the patient is always in one position lying on his stomach, since it is painful for him to move any part of the body.
Treatment of osteochondrosis includes several measures that complement each other. It is necessary to strictly follow the doctor’s recommendations, since failure to follow the instructions will slow down the healing process or the treatment will be ineffective.
Why is osteochondrosis of the lumbar spine dangerous?
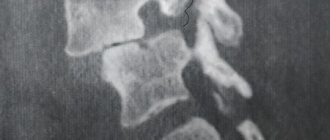
The initial stage of development of lumbar osteochondrosis appears in protrusion, when the intervertebral disc begins to go beyond its limits, protruding with a root between the vertebral sections. Further, when the disease progresses, there is a violation of the integrity of the fibrous ring from which the gel-like core flows out, this condition is called intervertebral hernia. In the process of irritation and pinching of the spinal nerve, the nerve becomes inflamed, causing severe pain, that is, lumbar osteochondrosis ultimately progresses to radiculitis.
Another consequence that is likely in the absence of therapeutic measures for lumbar osteochondrosis is sciatica. Sciatica is an inflammation of the sciatic nerve. In this condition, the patient experiences severe pain in the lumbar region, which is reflected by pain in the leg, which may be accompanied by muscle numbness. Due to severe pain, a person tries to avoid putting pressure on the painful side, curving the spine, which further aggravates the blood circulation of the discs, provoking a further process of destruction.
Another possible consequence of lumbar osteochondrosis is acquired compression myelopathy, in which the spinal canal narrows due to disc proliferation, impairing blood circulation.
Due to acquired instability of the spine, the column begins to sag from the sacral area, affecting adjacent organs. Women can get problems with the uterus, ovaries, men risk impairing potency.
And finally, the most dangerous consequence of lumbar osteochondrosis is the acquisition of cauda equina syndrome. In its advanced form, the disease affects all nerves from the first to the last vertebra, resulting in complete or partial paralysis of the legs and buttocks.
What is lumbosacral osteochondrosis
In addition to the 33 bones that make up the vertebral column, the human spinal cord also includes cartilaginous intervertebral discs. They provide stability to the spine against vertical loads, and also play the role of a spring, softening movements - it is thanks to them that our bones do not rub against each other, and our back bends. Together with muscles and ligaments, they are involved in the human body adopting various positions. Without these cartilage "spacers", we would not be able to run, jump and walk without suffering from excruciating headaches and injuries. However, over time, they tend to wear out - this is facilitated by the genetic “weakness” of cartilage tissue, and uneven distribution of load (for example, with poor posture), and poor nutrition, and many other factors that relate to the lifestyle of a modern person. The disease is characterized by a chronic course with periodic relapses. A complete cure is impossible, but timely treatment of osteochondrosis of the lumbar spine gives an almost 100% effect and returns to normal life.
Degenerative changes in the cartilage tissue of the spine lead to degeneration of the intervertebral discs. It is expressed in discomfort when moving, muscle hypertonicity, sharp shooting or constant aching pain. The consequence of abrasion of the intervertebral discs is deterioration of tissue trophism, the appearance of microcracks in the bones and osteophytes, protrusion of the spinal cord, and compression of internal organs. For this reason, lumbar osteochondrosis is called a disease of the whole body - it is capable of triggering a chain of metabolic disorders that affect the abdominal and pelvic organs (primarily the gastrointestinal tract and genitourinary system), the spinal cord and brain, and so on. Radicular syndrome, or radiculopathy, caused by this disease can cause neuralgic pain in the heart and even the stomach. Sometimes leg paresis and other severe symptoms of osteochondrosis of the lumbar spine are observed.
When the disease is localized in the lumbar region, vertebral displacements often occur due to sudden everyday movements. In this case, it becomes difficult for patients to walk and sit, an inflammatory process begins, the relief of which requires drug treatment, physiotherapy, a special exercise therapy program for osteochondrosis of the lumbar spine and observation by an orthopedist. In some cases, realignment of the vertebrae is required - a rather painful procedure, after which significant relief occurs after 1-2 days. It can only be carried out by a chiropractor - an osteopath and a vertebroneurologist.
Causes of lumbar osteochondrosis
The reasons why this disease is acquired most often include the following:
- low intensity physical activity;
- diseases of the thyroid gland, cardiovascular system, gastrointestinal tract;
- high physical activity, weightlifting;
- diseases of the vertebral joints, in particular rheumatoid arthritis
- vertebral underdevelopment;
- flat feet;
- spinal injuries, especially those in the lumbar and cruciate regions;
- incorrect metabolism;
- spinal degeneration associated with age-related changes.
The risk group for lumbar osteochondrosis includes people who:
- have a curvature of the spine;
- suffer from obesity and metabolic disorders;
- are in a bent position for a long time;
- have a hereditary predisposition;
- are in an environment of increased stress;
- have sleep disorders, get little rest;
- subject the body to hypothermia;
- are representatives of such professions as loaders, builders, drivers, and also have specialties related to constant presence at the computer.
Osteochondrosis of the sacral spine: drug therapy
One of the components of the treatment of osteochondrosis of the sacral spine is drug treatment. Taking medications helps remove inflammation and pain, relax muscles, and stop the degenerative process. For osteochondrosis, the following types of medications are used:
- non-steroidal anti-inflammatory drugs. They help eliminate inflammation and act as a pain reliever;
- painkillers. If non-steroidal anti-inflammatory drugs do not cope with pain, the patient is prescribed additional stronger analgesics;
- muscle relaxants. Helps relieve muscle spasms;
- chondroprotectors. Restore and strengthen bone and joint tissue, slow down the progression of the degenerative-dystrophic process;
- Vitamin and mineral complexes. B vitamins, which are usually prescribed for osteochondrosis, improve nerve conduction, and multivitamins have a strengthening effect on the body.
When osteochondrosis worsens, the patient is prescribed “blockades”. This is the introduction of an anesthetic directly into the affected area using an injection. This way you can quickly eliminate acute pain and begin the main course of treatment.
Symptoms of lumbar osteochondrosis
In addition to the pain that those suffering from lumbar osteochondrosis experience, especially during periods of heavy stress, there are also other symptoms of this disease, which manifest themselves in the following:
- dull pain that moves from the source of inflammation to the leg;
- increased pain when lifting something heavy, changing body position, coughing, sneezing;
- when you stay in one position for a long time, blood accumulates in the lesion, and at the slightest attempt to change position, sharp pain occurs;
- constant tension in the back muscles;
- lumbar lumbago at the slightest hypothermia;
- numbness of the thigh, gluteal muscles, lower leg and foot;
- tingling sensation in the legs;
- arterial spasm to the point of pulselessness;
- pathology of sweat glands;
- drying of the skin in the area of pain and loss of sensitivity.
How to treat lumbar osteochondrosis
The question of how to treat osteochondrosis of the lumbar spine - with drugs or non-drug therapy - cannot be answered unambiguously. Treatment of the disease is carried out in several directions:
- elimination of symptoms
that reduce the patient’s quality of life; - partial regeneration of connective tissue
; - implementation of a preventive program
that prevents the progression of destructive processes in cartilage and bone tissues (maintaining a muscle corset, general tone, etc.).
Cartilage is devoid of nerve endings and blood vessels - this determines the specifics of diagnosis and treatment of osteochondrosis. Firstly, cartilage cannot hurt, and therefore self-diagnosis of the disease is difficult and the vast majority of patients turn to an orthopedist or vertebroneurologist already with lumbar osteochondrosis of the 2nd or 3rd degree. The further the destruction of cartilage goes, the more stress the already worn out discs experience, the faster the disease progresses, and the more difficult it is to achieve positive changes. The reason for this lies in the fact that the cellular restoration of cartilage occurs very slowly - tissue nutrition occurs mainly in a diffuse manner. Therefore, a general improvement in the patient’s condition plays an important role on the path to remission. The treatment of lumbar osteochondrosis necessarily includes diet, maintenance medications for 1-3 months, as well as special gymnastic exercises. In exercise, separate time is allocated for warm-ups, which stimulate the nutrition of adjacent tissues, and therefore cartilage. Warm-ups must alternate between episodes of exercise, be it sitting at the computer or long walking.
Sometimes the doctor may prescribe the wearing of compression devices - for example, corsets, bandages to support the spine in the correct position. This measure is effective for concomitant postural disorders.
Drug treatment of osteochondrosis of the lumbar spine
Drugs for the treatment of osteochondrosis of the lumbar spine include oral and external anti-inflammatory drugs, muscle relaxants, analgesics, chondroprotectors, as well as drugs to improve metabolism (B vitamins and others) and blood circulation, glucocorticosteroids, neurotransmitters, enzymes. With reduced immunity and susceptibility to infectious diseases, immunomodulators are used. Constant pain can lead to depression, which also requires treatment. If the patient suffers from convulsions or swelling, anticonvulsants and diuretics are also prescribed. Tablets for lumbar osteochondrosis, suspensions, injections, gels and applicators do not need to be used constantly - usually the doctor prescribes an individual maintenance course at significant intervals. In the acute phase, with extremely severe pain, a specialist can place the so-called. paravertebral blockade - an injection of an anesthetic into the place where the nerve root exits the spine.
Sacral osteochondrosis: treatment and diagnosis in Moscow
Before starting treatment, it is very important to establish the exact type of disease and its location. In Moscow, diagnosis and treatment of osteochondrosis is carried out efficiently at the Yusupov Hospital. The hospital's diagnostic center is equipped with the latest technology, which allows you to quickly and accurately identify pathology, and this is important for the speedy start of adequate therapy.
Treatment of osteochondrosis at the Yusupov Hospital is performed by experienced neurologists, physiotherapists, rehabilitation specialists and other specialists. The hospital staff includes qualified exercise therapy instructors, massage therapists, and reflexologists. Extensive experience and high professionalism of specialists allow us to achieve maximum results in the treatment of the most complex cases of osteochondrosis. The course of therapy is selected individually, taking into account all the characteristics of the patient, his condition and physical capabilities. This promotes smooth and reliable recovery of the body and improved health.
You can make an appointment with neurologists, rehabilitation specialists, physiotherapists and other clinic specialists, find out information about the work of the diagnostic center and other questions of interest by calling the Yusupov Hospital.
Osteochondrosis of the sacral region: physiotherapy
Physiotherapeutic methods of treating osteochondrosis are as important as medications. Without their implementation, it is impossible to achieve positive results in the treatment of osteochondrosis. Physiotherapy begins after the end of the acute period of the disease. The procedures are performed in a medical facility under the supervision of specialists. In the future, some of them (for example, exercise therapy) can continue to be performed at home.
Physiotherapy methods include:
- physical therapy (physical therapy);
- massage;
- spinal traction;
- reflexology (acupuncture);
- hardware methods (electrophoresis, ultrasound, laser therapy, magnetic therapy).
The procedures are prescribed by neurologists and a physiotherapist. They must be completed in a course of 10 sessions. If necessary, the course of physiotherapy is repeated after a certain period of time.